Slides and Transcript
Slide 2 of 27
So glutamatergic agents have really become more and more popular in OCD treatment strategy. Glutamate is the primary excitatory CNS neurotransmitter. We first knew that there may be an issue with glutamate in OCD, because of genetic studies that were done about 20 years ago that implicated the SLC1A1 transporter. And animal studies have also implicated synaptic protein SAPAP3, again also related to glutamate. And so there were secondary evidence from neuroimaging and neurochemical data that generally support that there seems to be a glutamatergic problem in the treatment in OCD.
References:
- Coelho, D. R. A., Yang, C., Suriaga, A., et al. (2025). Glutamatergic medications for obsessive-compulsive and related disorders: A systematic review and meta-analysis. JAMA Network Open, 8(1), e2452963. https://doi.org/10.1001/jamanetworkopen.2024.52963
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 27
So one of the medications that is most commonly used nowadays is memantine. It’s a non-competitive NMDA receptor antagonist. Now, it’s approved for Alzheimer’s disease. One of the very early studies did show that 6 of 14 patients improved. This was a case series that was done. They gave memantine to 14 patients; 6 of them responded. And you can see that the responders had a much greater decrease in their Y-BOCS compared to people who were non-responders. So if you respond to memantine, you seem to respond fairly robustly.
References:
- Aboujaoude, E., Barry, J. J., & Gamel, N. (2009). Memantine augmentation in treatment-resistant obsessive-compulsive disorder: an open-label trial. Journal of Clinical Psychopharmacology, 29(1), 51–55. https://doi.org/10.1097/JCP.0b013e318192e9a4
Slide 4 of 27
There was a single blind treatment in an intensive residential program where 44 patients, at the OCD institute. There were 22 who received memantine, and noticed that the Y-BOCS decreased much greater in the memantine group than in the group that was not getting memantine. And so 35% of the memantine group were related as very much improved. Only 7.1% of control subjects were related as improved. So even though the Y-BOCS decrease doesn’t look very large, the clinical improvement on the CGI was actually pretty high. And that often is the case with OCD. Sometimes, small changes in the Y-BOCS can cause a big clinical improvement in the patient.
References:
- Stewart, S. E., Jenike, E. A., Hezel, D. M., Stack, D. E., Dodman, N. H., Shuster, L., & Jenike, M. A. (2010). A single-blinded case-control study of memantine in severe obsessive-compulsive disorder. Journal of Clinical Psychopharmacology, 30(1), 34-39. https://doi.org/10.1097/JCP.0b013e3181c856de
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 27
So memantine. The bottom line is this has been shown to work in two double-blind placebo-controlled trials. One was in treatment-resistant patients and one was in treatment-responsive patients. So memantine works in both treatment-resistant and treatment-responsive patients. It really should be used at a minimum of 20 mg daily, and we can dose it as high as 40 mg a day.
References:
- Aboujaoude, E., Barry, J. J., & Gamel, N. (2009). Memantine augmentation in treatment-resistant obsessive-compulsive disorder: an open-label trial. Journal of Clinical Psychopharmacology, 29(1), 51–55. https://doi.org/10.1097/JCP.0b013e318192e9a4
- Stewart, S. E., Jenike, E. A., Hezel, D. M., Stack, D. E., Dodman, N. H., Shuster, L., & Jenike, M. A. (2010). A single-blinded case-control study of memantine in severe obsessive-compulsive disorder. Journal of Clinical Psychopharmacology, 30(1), 34-39. https://doi.org/10.1097/JCP.0b013e3181c856de
Slide 6 of 27
Memantine may be especially useful for compulsions. Many patients will report to me that their obsessions remain the same, but they no longer feel the great urge to actually do the compulsion. It is the reason now that it is my first-line augmentation outside of clomipramine, just because it has a good response and because the side effect profile was so low. We have less side effects than the second-generation antipsychotics although there is much less evidence with memantine than the second-generation antipsychotics. That’s why I believe it makes a much better first- or second-line augmenter.
References:
- Grant, J. E., Chesivoir, E., Valle, S., Ehsan, D., & Chamberlain, S. R. (2023). Double-blind placebo-controlled study of memantine in trichotillomania and skin-picking disorder. The American Journal of Psychiatry, 180(5), 348–356. https://doi.org/10.1176/appi.ajp.20220737
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 27
Memantine has now been shown to be more effective for body-focused repetitive behaviors in a single trial. So body-focused repetitive behaviors are issues with skin picking, hair pulling or other types of body-focused behaviors. And you may use the memantine instead of NAC for BFRBs because being that it’s a prescription medication I think we can ensure better formulation as opposed to what you’re buying over the counter.
References:
- Grant, J. E., Chesivoir, E., Valle, S., Ehsan, D., & Chamberlain, S. R. (2023). Double-blind placebo-controlled study of memantine in trichotillomania and skin-picking disorder. The American Journal of Psychiatry, 180(5), 348–356. https://doi.org/10.1176/appi.ajp.20220737
Slide 8 of 27
Another glutamatergic medication with some good evidence for OCD is riluzole. Riluzole is a calcium and sodium channel blocker that’s approved for amyotrophic lateral sclerosis. So it inhibits synaptic glutamate release, and enhances glutamate uptake by the astrocytes.
References:
- Pittenger, C., Bloch, M. H., Wasylink, S., Billingslea, E., Simpson, R., Jakubovski, E., Kelmendi, B., Sanacora, G., & Coric, V. (2015). Riluzole augmentation in treatment-refractory obsessive-compulsive disorder: A pilot randomized placebo-controlled trial. The Journal of Clinical Psychiatry, 76(8), 1075–1084. https://doi.org/10.4088/JCP.14m09123
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 27
Now, with riluzole, one issue is that the patients require monthly monitoring of their transaminases. Their liver enzymes often go up with riluzole and we need to check and make sure that it goes down over time. It seems to be a transient elevation only, so we monitor once a month for three months and then every three months for a year, and then periodically after that. I will monitor on a monthly basis or every three months at a minimum until the LFTs have gone back down to their baseline range and then after that periodically.
References:
- Pittenger, C., Bloch, M. H., Wasylink, S., Billingslea, E., Simpson, R., Jakubovski, E., Kelmendi, B., Sanacora, G., & Coric, V. (2015). Riluzole augmentation in treatment-refractory obsessive-compulsive disorder: A pilot randomized placebo-controlled trial. The Journal of Clinical Psychiatry, 76(8), 1075–1084. https://doi.org/10.4088/JCP.14m09123
Slide 10 of 27
Riluzole has been shown to be effective in both case series and in open label trials. It worked in one randomized controlled trial. What was interesting, there was a subset of patients that it worked for only in their obsessions but in the other subset of people that it did not work. It seems to be effective also in children but interestingly riluzole is not effective as an add-on in children, and was only effective as a single agent. In adults, it was effective as an augmenter to SSRIs. It seems to improve mood and anxiety as well as obsessions and also is well tolerated except for the LFTs.
References:
- Coelho, D. R. A., Yang, C., Suriaga, A., et al. (2025). Glutamatergic medications for obsessive-compulsive and related disorders: A systematic review and meta-analysis. JAMA Network Open, 8(1), e2452963. https://doi.org/10.1001/jamanetworkopen.2024.52963
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 27
So there are some favorable results in open label and case series trials. So there’s a 12-week open label trial at 100 mg a day. 7 of 13 responders were at the typical 100 mg a day, some were up to 200. And they had a greater than 35% reduction in their Y-BOCS with no adverse effects.
References:
- Coric, V., Taskiran, S., Pittenger, C., Wasylink, S., Mathalon, D. H., Valentine, G., Saksa, J., Wu, Y. T., Gueorguieva, R., Sanacora, G., Malison, R. T., & Krystal, J. H. (2005). Riluzole augmentation in treatment-resistant obsessive-compulsive disorder: an open-label trial. Biological Psychiatry, 58(5), 424-428. https://doi.org/10.1016/j.biopsych.2005.04.043
Slide 12 of 27
Another riluzole trial, 4 of 6 responders at 100 mg a day showed a greater than 39% reduction in their Y-BOCS. That is a significant improvement. But again, no significant difference in a followup double-blind, randomized controlled trial.
References:
- Grant, P., Lougee, L., Hirschtritt, M., & Swedo, S. E. (2007). An open-label trial of riluzole, a glutamate antagonist, in children with treatment-resistant obsessive-compulsive disorder. Journal of Child and Adolescent Psychopharmacology, 17(6), 761–767. https://doi.org/10.1089/cap.2007.0021
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 27
Now, it was treatment-resistant children. There was a large amount of them. 17 had comorbid autism. 85% completed the trial. The Y-BOCS in the riluzole group decreased from 27 to a little under 22. In the placebo group, they decreased from 29 to 22.5. So it’s a fairly significant decrease even in the placebo group. So there were about the same number of patient responders in both groups. So what’s important to note is glutamatergic agents don’t act the same in children as they do in adults. And overall, the data seem to be a little more consistent with adults.
References:
- Grant, P. J., Joseph, L. A., Farmer, C. A., Luckenbaugh, D. A., Lougee, L. C., Zarate, C. A., Jr, & Swedo, S. E. (2014). 12-week, placebo-controlled trial of add-on riluzole in the treatment of childhood-onset obsessive-compulsive disorder. Neuropsychopharmacology, 39(6), 1453–1459. https://doi.org/10.1038/npp.2013.343
Slide 14 of 27
Let’s talk about N-acetylcysteine. It’s an amino acid derivative that modulates glutamate transmission. Everyone has used it in their residency. And it’s an inhaled version for acetaminophen overdose. Note that the randomized controlled trials have either been mixed or negative when used as an augmenter to OCD.
References:
- Costa, D. L. C., Diniz, J. B., Requena, G., Joaquim, M. A., Pittenger, C., Bloch, M. H., Miguel, E. C., & Shavitt, R. G. (2017). Randomized, double-blind, placebo-controlled trial of N-acetylcysteine augmentation for treatment-resistant obsessive-compulsive disorder. The Journal of Clinical Psychiatry, 78(7), e766–e773. https://doi.org/10.4088/JCP.16m11101
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 27
Now, it has been shown to be effective in body-focused repetitive behaviors. So you can use it for BFRB. However, we do not recommend it for OCD at this time. And as of this point, I’m typically recommending memantine over NAC for BFRB simply because that we can give a prescription medication where we can be more assured of the formulation.
References:
- Costa, D. L. C., Diniz, J. B., Requena, G., Joaquim, M. A., Pittenger, C., Bloch, M. H., Miguel, E. C., & Shavitt, R. G. (2017). Randomized, double-blind, placebo-controlled trial of N-acetylcysteine augmentation for treatment-resistant obsessive-compulsive disorder. The Journal of Clinical Psychiatry, 78(7), e766–e773. https://doi.org/10.4088/JCP.16m11101
Slide 16 of 27
There’s another glutamatergic agent called D-cycloserine. This was originally a tuberculin medication and may accelerate extinction learning. It seems to be well tolerated with only GI distress, dizziness, and anxiety being the major side effects.
References:
- Kvale, G., Hansen, B., Hagen, K., Abramowitz, J. S., Børtveit, T., Craske, M. G., Franklin, M. E., Haseth, S., Himle, J. A., Hystad, S., Kristensen, U. B., Launes, G., Lund, A., Solem, S., & Öst, L. G. (2020). Effect of D-cycloserine on the effect of concentrated exposure and response prevention in difficult-to-treat obsessive-compulsive disorder: A randomized clinical trial. JAMA Network Open, 3(8), e2013249. https://doi.org/10.1001/jamanetworkopen.2020.13249
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 27
There have been a number of different studies done with D-cycloserine. So in a 2020 study, they either gave doses of 100 or 250 at lunchtime in the middle of a four-day long ERP session. No differences were noted with placebo but because it was an intensive ERP session, the intensive ERP seemed to probably overpower what the D-cycloserine did.
References:
- Kvale, G., Hansen, B., Hagen, K., Abramowitz, J. S., Børtveit, T., Craske, M. G., Franklin, M. E., Haseth, S., Himle, J. A., Hystad, S., Kristensen, U. B., Launes, G., Lund, A., Solem, S., & Öst, L. G. (2020). Effect of D-cycloserine on the effect of concentrated exposure and response prevention in difficult-to-treat obsessive-compulsive disorder: A randomized clinical trial. JAMA Network Open, 3(8), e2013249. https://doi.org/10.1001/jamanetworkopen.2020.13249
Slide 18 of 27
There have been numerous different protocols that had been done with D-cycloserine. Some studies have shown advantage for D-cycloserine if you give it before or during the treatment and they seem to get a more rapid response with the ERP. However, that goes away with additional treatment. So in other words, even in the best-case scenario, D-cycloserine seems to help the initial response to ERP but the end result is no different than it is with people not on D-cycloserine. At this point, there is no timing and dosing that is still standard for D-cycloserine. As a result, it’s really not ready for primetime. It’s a medication that really should only be used in research studies and it’s less accessible in children.
References:
- Kvale, G., Hansen, B., Hagen, K., Abramowitz, J. S., Børtveit, T., Craske, M. G., Franklin, M. E., Haseth, S., Himle, J. A., Hystad, S., Kristensen, U. B., Launes, G., Lund, A., Solem, S., & Öst, L. G. (2020). Effect of D-cycloserine on the effect of concentrated exposure and response prevention in difficult-to-treat obsessive-compulsive disorder: A randomized clinical trial. JAMA Network Open, 3(8), e2013249. https://doi.org/10.1001/jamanetworkopen.2020.13249
- Andersson, E., Hedman, E., Enander, J., et al. (2015). d-Cycloserine vs placebo as adjunct to cognitive behavioral therapy for obsessive-compulsive disorder and interaction with antidepressants: A randomized clinical trial. JAMA Psychiatry, 72(7), 659-667. https://doi.org/10.1001/jamapsychiatry.2015.0546
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 27
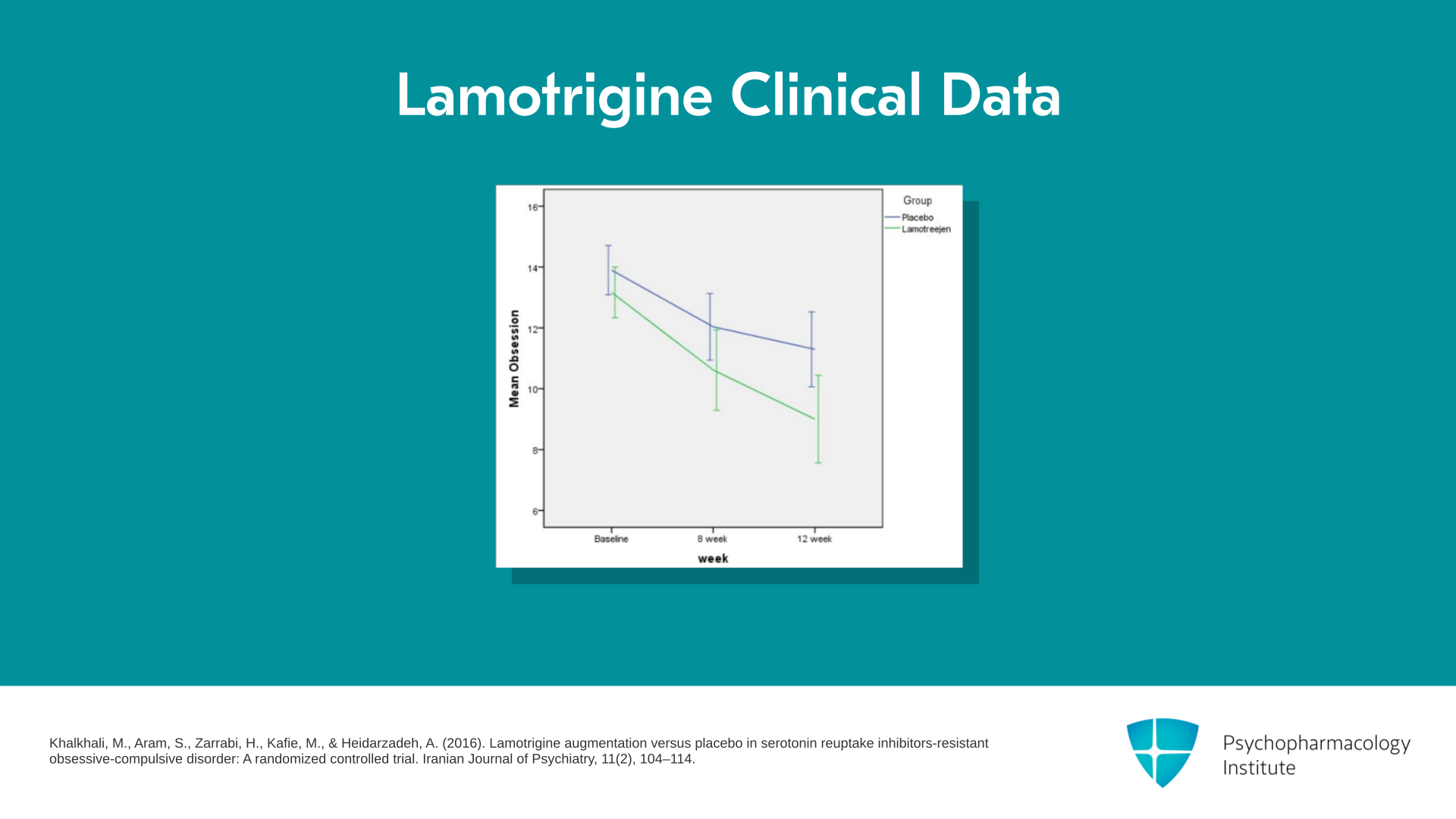
There is another glutamatergic medication that has been showing some good data, lamotrigine. Lamotrigine is an anticonvulsant with some anti-glutamatergic properties, and there was one double-blind, randomized controlled trial that showed improvement. The study group had a significant decrease compared to the placebo group with a p of 0.015.
References:
- Khalkhali, M., Aram, S., Zarrabi, H., Kafie, M., & Heidarzadeh, A. (2016). Lamotrigine augmentation versus placebo in serotonin reuptake inhibitors-resistant obsessive-compulsive disorder: A randomized controlled trial. Iranian Journal of Psychiatry, 11(2), 104–114.
Slide 20 of 27
There was another double-bind, randomized controlled trial that had 33 completers and significant clinical global improvement in the active group. Now, patients who have comorbid schizoaffective disorder may show even more improvement though right now we need more studies.
References:
- Bruno, A., Micò, U., Pandolfo, G., Mallamace, D., Abenavoli, E., Di Nardo, F., D'Arrigo, C., Spina, E., Zoccali, R. A., & Muscatello, M. R. (2012). Lamotrigine augmentation of serotonin reuptake inhibitors in treatment-resistant obsessive-compulsive disorder: a double-blind, placebo-controlled study. Journal of Psychopharmacology, 26(11), 1456–1462. https://doi.org/10.1177/0269881111431751
- Poyurovsky, M., Glick, I., & Koran, L. (2008). Lamotrigine augmentation in schizophrenia and schizoaffective patients with obsessive-compulsive symptoms. Journal of Psychopharmacology, 24(6), 861-866. https://doi.org/10.1177/0269881108099215
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 21 of 27
There have only been these two small studies with lamotrigine, it seems that lamotrigine may be effective as an augmenter to the SSRI, but it seems to be particularly good with comorbid mood or psychotic disorders. So I typically will think about lamotrigine augmentation if my patients have comorbid bipolar disorder or comorbid schizophrenia.
References:
- Pittenger, C., Brennan, B. P., Koran, L., Mathews, C. A., Nestadt, G., Pato, M., Phillips, K. A., Rodriguez, C. I., Simpson, H. B., Skapinakis, P., Stein, D. J., & Storch, E. A. (2021). Specialty knowledge and competency standards for pharmacotherapy for adult obsessive-compulsive disorder. Psychiatry Research, 300, 113853. https://doi.org/10.1016/j.psychres.2021.113853
Slide 22 of 27
There are other glutamatergic medications that have been studied as well such as ketamine, which is a non-competitive NMDA antagonist. Ketamine seems to have a robust anti-obsessional effect, but it’s fairly transient of an antidepressant effect. There is some possible benefit in unmedicated patients. However, in medicated patients who are on SSRIs, the benefit seems to be minimal. And in the initial studies, it actually triggered suicidal ideations into patients.
References:
- Rodriguez, C. I., Kegeles, L. S., Levinson, A., Feng, T., Marcus, S. M., Vermes, D., Flood, P., & Simpson, H. B. (2013). Randomized controlled crossover trial of ketamine in obsessive-compulsive disorder: proof-of-concept. Neuropsychopharmacology, 38(12), 2475–2483. https://doi.org/10.1038/npp.2013.150
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 23 of 27
Note that there’s also really limited data for esketamine. Esketamine is the version that you can give in your office. So as a result, right now, we’re not recommending ketamine outside of research settings.
References:
- Martinotti, G., Chiappini, S., Pettorruso, M., Mosca, A., Miuli, A., Di Carlo, F., D'Andrea, G., Collevecchio, R., Di Muzio, I., Sensi, S. L., & Di Giannantonio, M. (2021). Therapeutic potentials of ketamine and esketamine in obsessive-compulsive disorder (OCD), substance use disorders (SUD) and eating disorders (ED): A review of the current literature. Brain Sciences, 11(7), 856. https://doi.org/10.3390/brainsci11070856
Slide 24 of 27
I want to talk about other glutamatergic medications that have been studied. Topiramate has been studied. There was one small randomized controlled trial that showed a decrease in the Y-BOCS, but a second showed no statistical improvement at all. Because of the side effects, topiramate is typically not used and generally not recommended.
References:
- Mowla, A., Khajeian, A. M., Sahraian, A., Chohedri, A. H., & Kashkoli, F. (2010). Topiramate augmentation in resistant OCD: A double-blind placebo-controlled clinical trial. CNS Spectrums, 15(11), 613–617. https://doi.org/10.1017/S1092852912000065
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 25 of 27
Pregabalin was looked at but only in case series and open label, very little data to go ahead and recommend that glutamatergic medication. Gabapentin was studied. There was one negative study with gabapentin in OCD. Unfortunately, I see gabapentin used quite a bit despite the fact that there is no data, and actually even one negative study with gabapentin in OCD. So not recommended for OCD treatment.
References:
- Kayser, R. R. (2020). Pharmacotherapy for treatment-resistant obsessive-compulsive disorder. The Journal of Clinical Psychiatry, 81(5), 19ac13182. https://doi.org/10.4088/JCP.19ac13182
- Farnia, V., Gharehbaghi, H., Alikhani, M., Almasi, A., Golshani, S., Tatari, F., Davarinejad, O., Salemi, S., Sadeghi Bahmani, D., Holsboer-Trachsler, E., & Brand, S. (2018). Efficacy and tolerability of adjunctive gabapentin and memantine in obsessive compulsive disorder: Double-blind, randomized, placebo-controlled trial. Journal of Psychiatric Research, 104, 137–143. https://doi.org/10.1016/j.jpsychires.2018.07.008
Slide 26 of 27
So the key points. Glutamatergic medications need more randomized controlled trials for greater evidence. So it’s not that the glutamatergic medications may not work. It’s just simply that the evidence isn’t there, because a lot of the research hasn’t been done. I think the risk-benefit analysis prioritizes glutamatergic medications over antipsychotic medications. Evidence for children and adults for this class of medication are very different, and we’re getting very different results with adults and children.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 27 of 27
So memantine and riluzole are the two most commonly used glutamatergic medications. There is increasing evidence for lamotrigine especially with comorbid mood and psychotic disorders. Medications like ketamine and D-cycloserine should not be used outside of a research setting. While NAC may be useful with BFRBs, it is not useful as an augmenter for OCD. Memantine may be preferred over NAC for BFRBs just due to its prescription status. Thank you.