Slides and Transcript
Slide 1 of 12
In this third video, we consider medical comorbidities and other special groups in the treatment of major depression that could change the basic or default algorithm.
We want you to think about these before you start to look at what we recommend because these are items that could change the basic algorithm or your basic approach. They also may require you to coordinate more closely than usual with other medical specialists that are treating this patient.
Slide 2 of 12
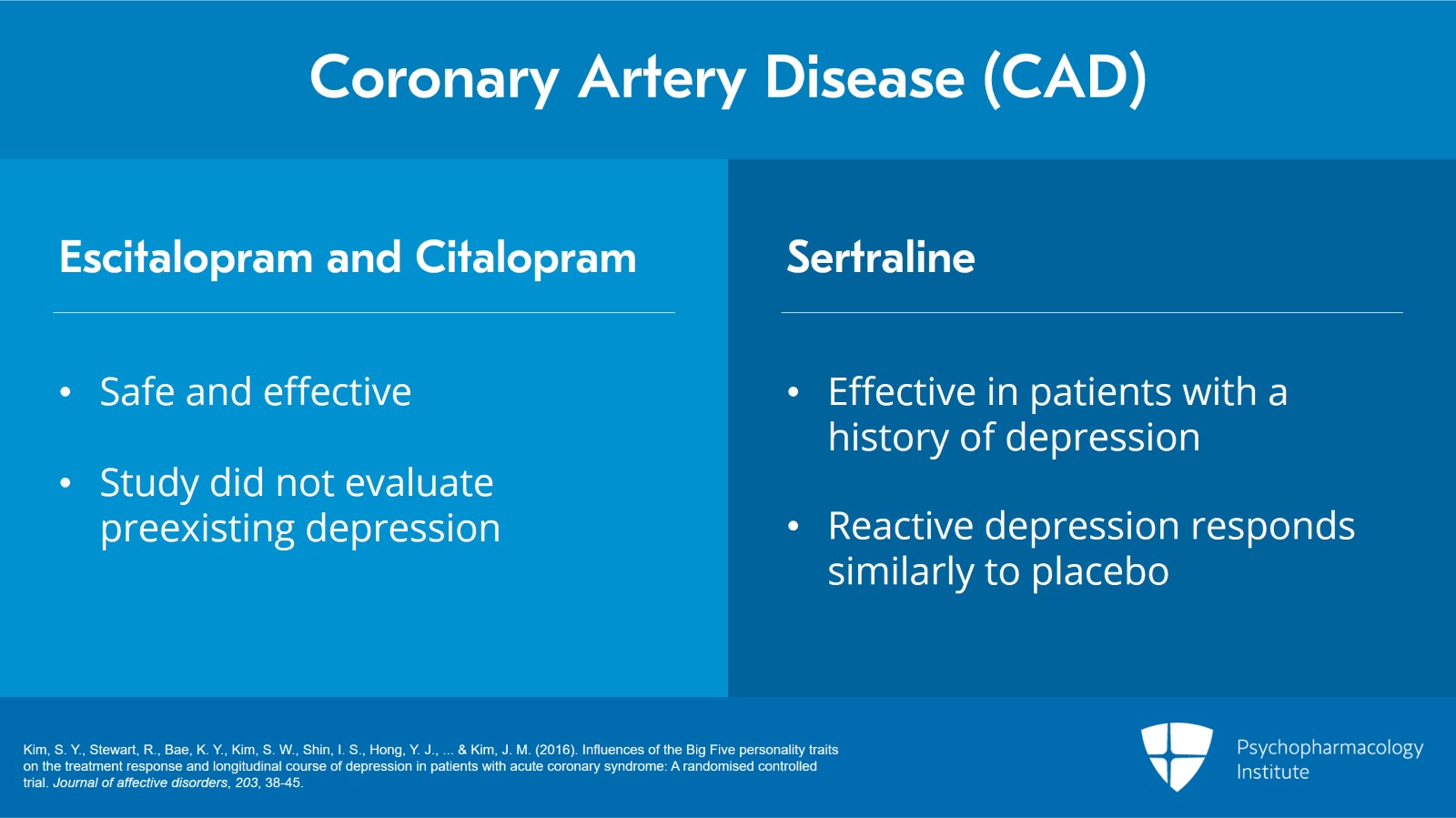
The first one I’m going to discuss is coronary artery disease.
Escitalopram and citalopram are two SSRIs that have been shown to be safe and effective for treatment of depression in patients with various levels of severity of coronary artery disease including recent heart attacks.
But the sertraline study was particularly interesting because they found that the effectiveness of sertraline was limited to patients who had a history of other depressive episodes prior to the onset of the coronary artery disease and its complications. For patients who develop their first depression with the onset of the coronary problem, there was actually no difference with placebo for the sertraline.
So in other words, these people had a reactive depression to the circumstances. They didn’t have a history of recurrent depression and then this was just the latest precipant for it. So reactive depressions tend to be no different from placebo in their response rates to pharmacotherapy.
So I’m not saying you should never treat these depressed people with coronary artery disease who’ve never been depressed before but certainly keep this study in mind because at the least if you do start an antidepressant you may want to be sure they really need it and if it’s worth the side effects that they’re getting later on.
Now, there’s also a study with escitalopram in the same population showing efficacy but in that study they did not evaluate this question of whether preexisting depression predicted outcome. So we don’t know if that’s also true for escitalopram.
References:
- Kim, S. Y., Stewart, R., Bae, K. Y., Kim, S. W., Shin, I. S., Hong, Y. J., … & Kim, J. M. (2016). Influences of the Big Five personality traits on the treatment response and longitudinal course of depression in patients with acute coronary syndrome: A randomised controlled trial. Journal of affective disorders, 203, 38-45.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 12
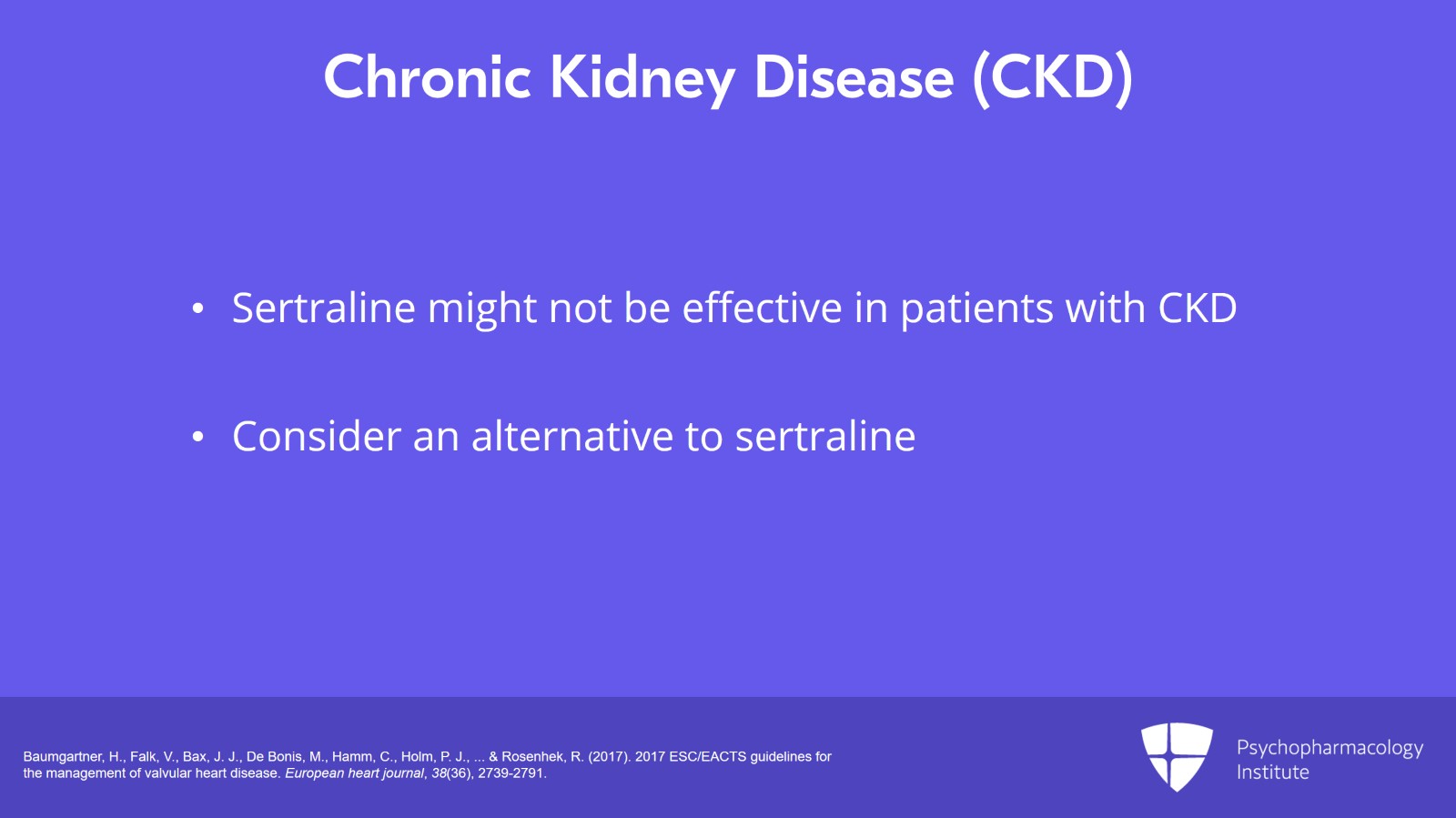
Now, another medical comorbidity is chronic kidney disease that is associated with depression.
It seems that sertraline might not be effective in depressions with patients with chronic kidney disease. These were chronic but not at the level of requiring dialysis.
So you might consider an alternative to sertraline because at least that antidepressant, although we do recommend it as one of our first line antidepressants for others, it didn’t seem effective for these patients with chronic kidney disease.
References:
- Baumgartner, H., Falk, V., Bax, J. J., De Bonis, M., Hamm, C., Holm, P. J., … & Rosenhek, R. (2017). 2017 ESC/EACTS guidelines for the management of valvular heart disease. European heart journal, 38(36), 2739-2791.
Slide 4 of 12
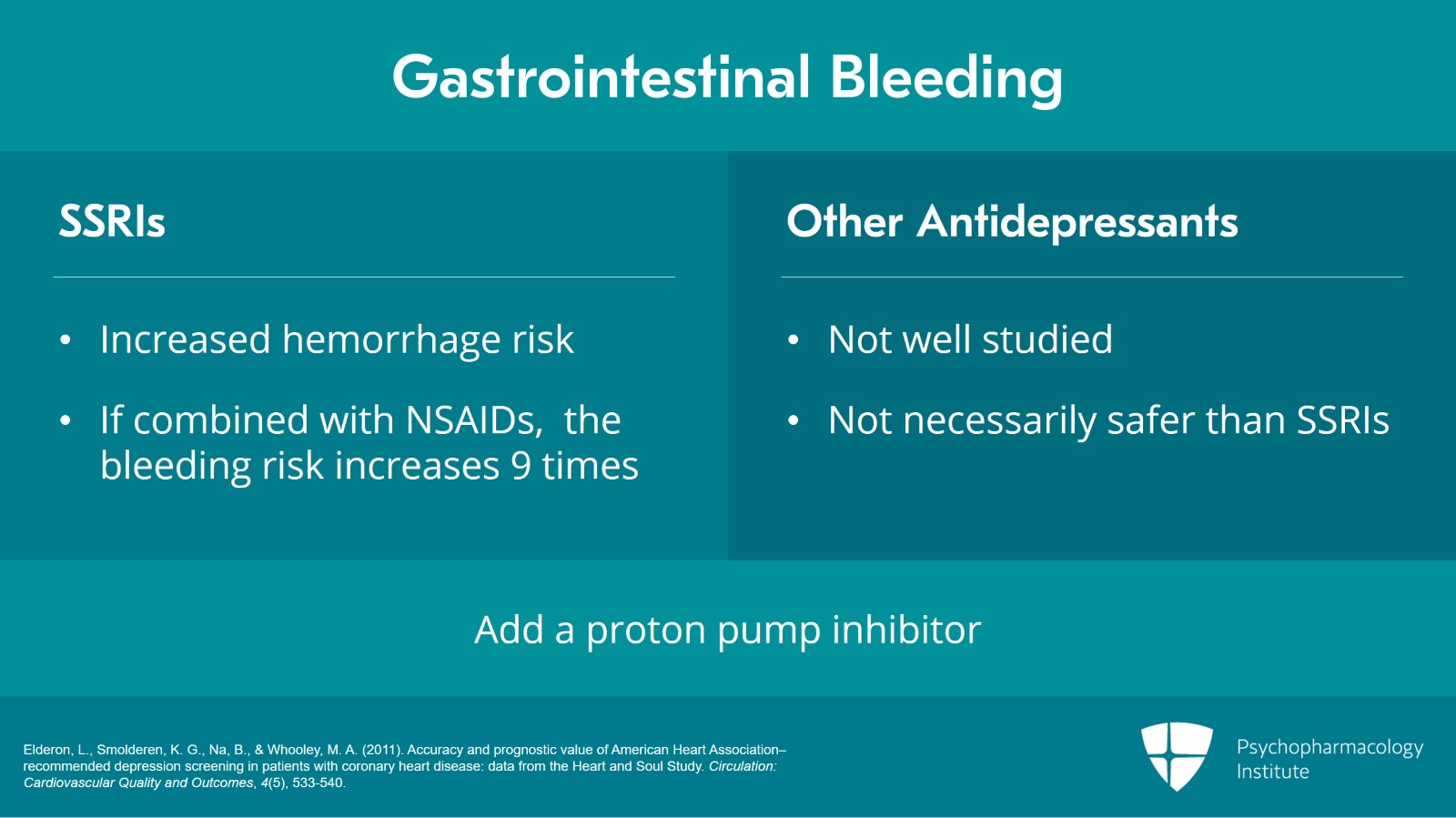
The next medical comorbidity to consider is gastrointestinal bleeding difficulties.
SSRIs increase hemorrhage risk from many kinds of hemorrhage not just gastrointestinal but that type of bleeding has been particularly well studied.
And studies have shown that if you have an SSRI being combined with an NSAID, a non-steroid anti-inflammatory like ibuprofen, gastrointestinal bleeding risk can be nine times as likely versus controls.
Other antidepressants are not well studied in terms of their anticoagulant effects but do seem to not be any safer, drugs like mirtazapine and bupropion.
There’s a review article on this issue and concludes that they’re not necessarily safer.
One thing that will help though is adding a proton pump inhibitor like omeprazole. This decreases the risk of gastrointestinal bleeding to only slightly above controls who are not on SSRIs. So you would most be worried about using an SSRI or other antidepressants if they’re on an NSAID and you’re going to start an antidepressant and there are no proton pump inhibitors on board.
References:
- Elderon, L., Smolderen, K. G., Na, B., & Whooley, M. A. (2011). Accuracy and prognostic value of American Heart Association–recommended depression screening in patients with coronary heart disease: data from the Heart and Soul Study. Circulation: Cardiovascular Quality and Outcomes, 4(5), 533-540.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 12
The next comorbidity to mention is cardiac arrhythmias.
As you would not be surprised to hear, you probably should avoid tricyclic antidepressants and MAOIs which we don’t recommend at the top of the algorithms but in some cases they are recommended. So you should give second consideration if there are cardiac arrhythmias.
Sertraline appears to be safe in patients at risk of arrhythmias following a myocardial infarction though but we do not recommend citalopram because of the concerns about QTc prolongation with that antidepressant.
Escitalopram is okay but don’t exceed the maximum dose of 20 mg because above that it does increase QTc significantly.
References:
- Glassman, A. H., O'Connor, C. M., Califf, R. M., Swedberg, K., Schwartz, P., Bigger Jr, J. T., … & Landau, C. (2002). Sertraline treatment of major depression in patients with acute MI or unstable angina. Jama, 288(6), 701-709.
Slide 6 of 12
Next consideration is depression in women of childbearing potential and pregnant women.
We talk about childbearing potential because of course pregnancy is very often unplanned. Up to 50% of pregnancies are unplanned. So you don’t know when the next pregnancy is coming on in a person who is of childbearing capacity. Anyway, depression is important to treat in pregnant women certainly. Depressed women adhere poorly with prenatal care. They don’t do well on many levels. And if they stop their antidepressants during pregnancy, relapse rates can be 43%.
References:
- Cohen, L. S., Soares, C. N., Vitonis, A. F., Otto, M. W., & Harlow, B. L. (2006). Risk for new onset of depression during the menopausal transition: the Harvard study of moods and cycles. Archives of general psychiatry, 63(4), 385-390.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 12
So we do want to treat but there are some issues to be thought about with SSRIs in pregnancy.
They may increase risk of postpartum hemorrhage, premature delivery and other postnatal complications although the studies that show these are hard to interpret because of confounding by indication.
It may be that the women who got the SSRIs were for some reason more likely to have those complications and it wasn’t the SSRI actually causing them. But certainly, you should discuss these issues before using them. There also may be some risk of speech and language disorders in the offspring of patients treated with SSRIs but again it could be confounding by indication.
References:
- Brown, A. S., Gyllenberg, D., Malm, H., McKeague, I. W., Hinkka-Yli-Salomäki, S., Artama, M., … & Sourander, A. (2016). Association of selective serotonin reuptake inhibitor exposure during pregnancy with speech, scholastic, and motor disorders in offspring. JAMA psychiatry, 73(11), 1163-1170.
Slide 8 of 12
The one antidepressant we would avoid would be paroxetine which has a D rating due to atrial septal defect risk.
References:
- Reefhuis, J., Devine, O., Friedman, J. M., Louik, C., & Honein, M. A. (2015). Specific SSRIs and birth defects: bayesian analysis to interpret new data in the context of previous reports. bmj, 351, h3190.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 12
The next risk group is older adults defined as over 65.
SSRIs and venlafaxine are associated with higher rates of hyponatremia. So you need to be on the lookout for that.
In patients with intolerable hyponatremia, you might consider mirtazapine which seems not to do that.
All the SSRIs seem equally problematic. SSRIs, TCAs and other antidepressants also have been associated with more falls in the elderly.
And consider ECT particularly right unilateral ultra-brief ECT in older adults with severe depression.
References:
- Greenblatt, H. K., & Greenblatt, D. J. (2016). Antidepressant-associated hyponatremia in the elderly. Journal of clinical psychopharmacology, 36(6), 545-549.
Slide 10 of 12
So in conclusion, the key points of this lecture today is that depression comorbid with coronary artery disease and chronic kidney disease may not respond as well if the patient never had depression before developing these problems. By not responding well I mean not respond compared with placebo. So these depressions may be more like an adjustment disorder.
We are recommending avoiding citalopram because of QTc problems. And escitalopram is okay but don’t exceed 20 mg again in these people with coronary artery disease.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 12
Avoid combining SSRIs with NSAIDs due to the GI hemorrhage risk unless the patient is also on a proton pump inhibitor. The fourth key point is avoid paroxetine in women of childbearing potential because of the risks of atrial septal defect. And finally, watch for hyponatremia and fall risk from antidepressants in the elderly.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.