Slides and Transcript
Slide 1 of 10
This is video 3 of the bipolar mania algorithm discussion. And in this video, we continue the discussion of co-occurring conditions that could affect the main algorithm that you should assess before commencing to use the algorithm’s recommendations. In this video, we’re going to discuss agitation requiring parenteral management, some medical comorbidities and anxiety disorders.
Slide 2 of 10
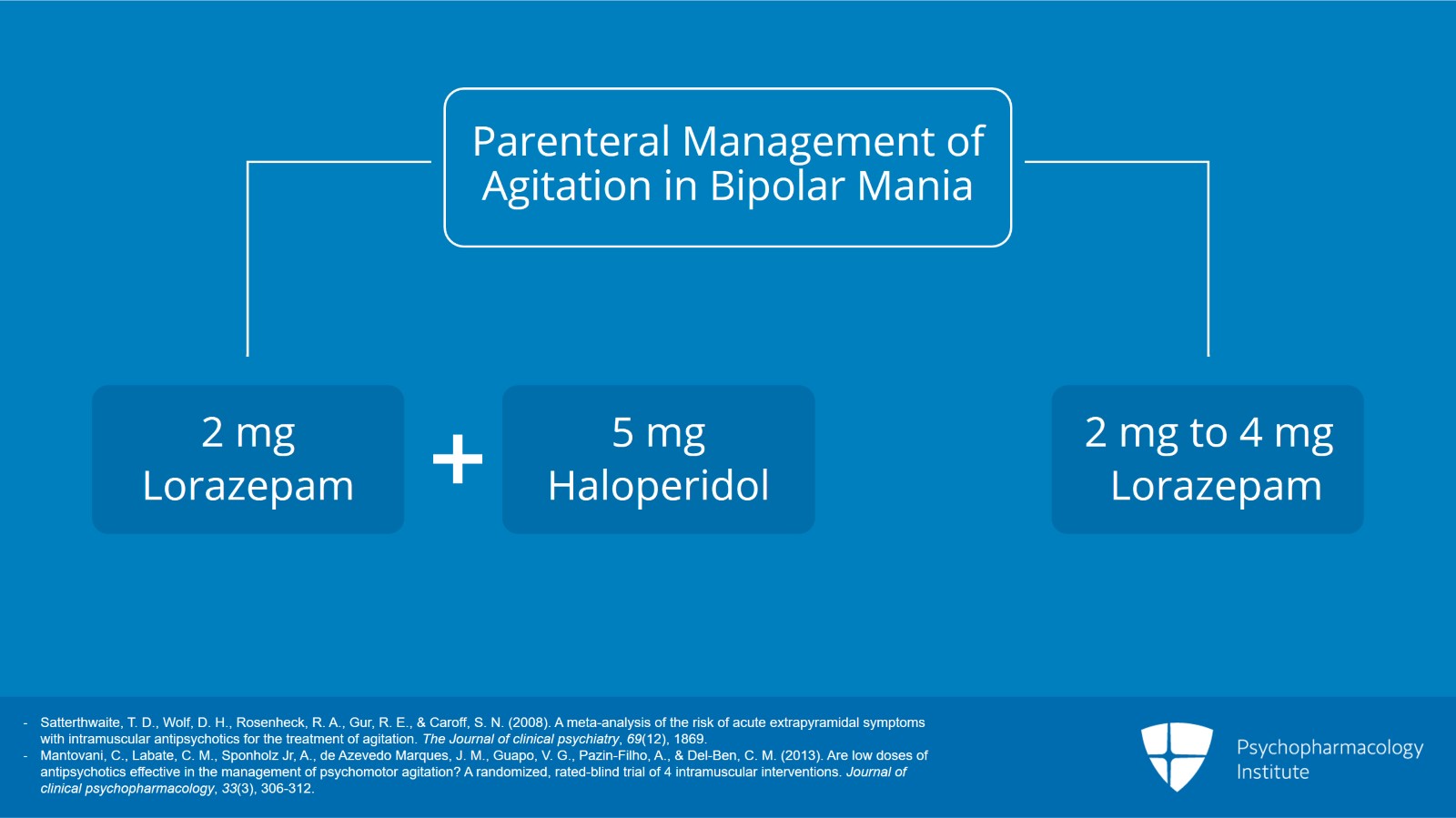
So what does one do if your manic patient is agitated and requires some immediate IM or parenteral management? Having reviewed this literature, we still feel that the longstanding preferred choice is still the preferred choice and that is using a combination of lorazepam or other benzodiazepine and haloperidol. Those two medications can be combined in the same syringe and a typical dose would be 2 mg of the lorazepam, 5 mg of haloperidol. Another option would be lorazepam alone, 2 to 4 mg IM.
References:
- Satterthwaite, T. D., Wolf, D. H., Rosenheck, R. A., Gur, R. E., & Caroff, S. N. (2008). A meta-analysis of the risk of acute extrapyramidal symptoms with intramuscular antipsychotics for the treatment of agitation. The Journal of clinical psychiatry, 69(12), 1869.
- Mantovani, C., Labate, C. M., Sponholz Jr, A., de Azevedo Marques, J. M., Guapo, V. G., Pazin-Filho, A., & Del-Ben, C. M. (2013). Are low doses of antipsychotics effective in the management of psychomotor agitation? A randomized, rated-blind trial of 4 intramuscular interventions. Journal of clinical psychopharmacology, 33(3), 306-312.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 10
We recommend avoiding IM chlorpromazine which some clinicians do still use especially of my generation where it was the standard for so long. A Cochrane review by Ahmed in 2010 of the pertinent evidence found that IM chlorpromazine is associated with significant risks of sudden severe hypotension, a problem you don’t get with the lorazepam plus haloperidol option.
References:
- Ahmed, U., Jones, H., & Adams, C. E. (2010). Chlorpromazine for psychosis induced aggression or agitation. Cochrane database of systematic reviews, (4).
Slide 4 of 10
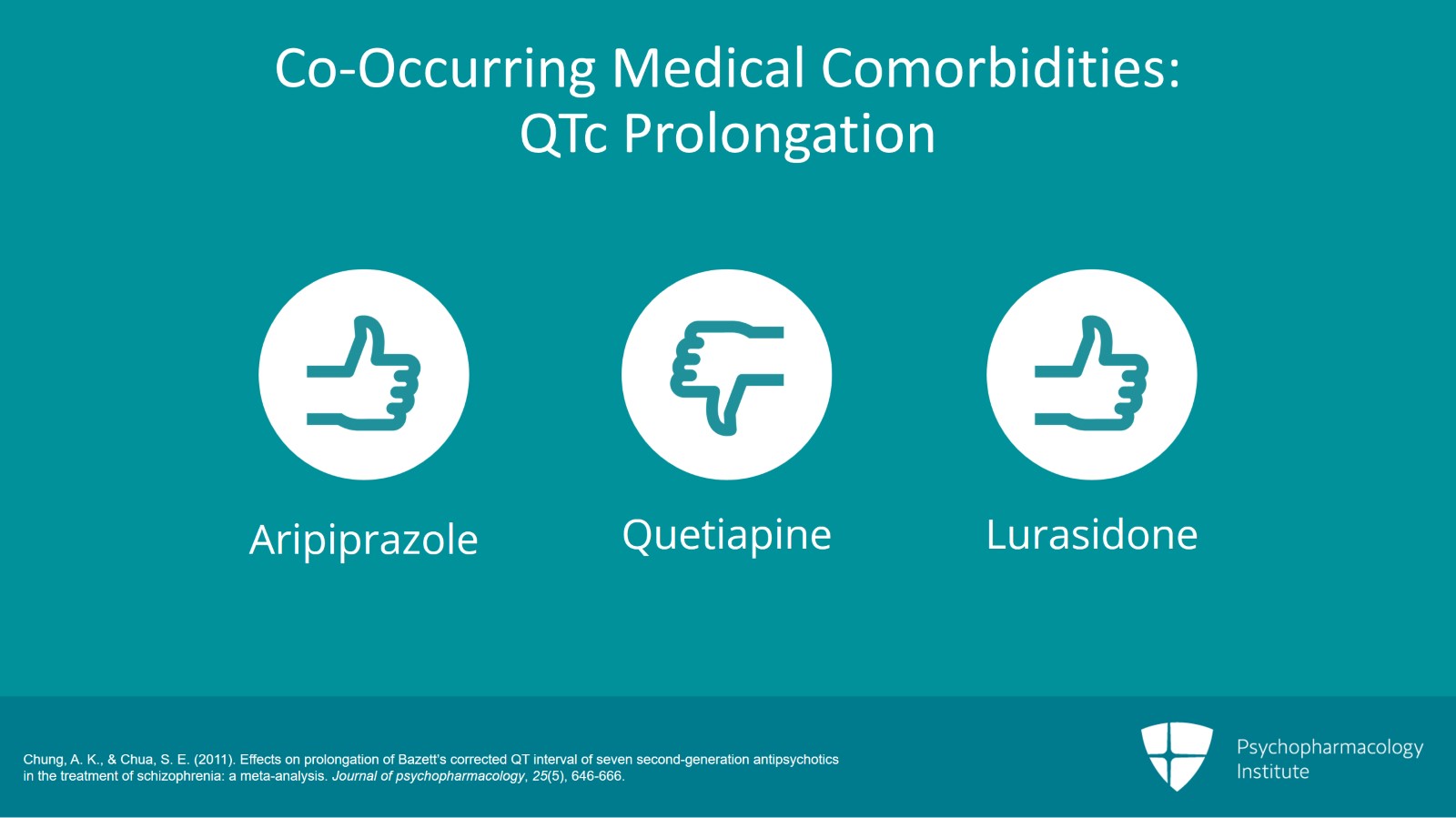
Next, we have certain medical comorbidities that could be an issue with the selection of medication in the algorithm. What if they have problems with QTc prolongation? That’s an issue with quite a few psychiatric and non-psychiatric medications. A review of the propensity of different medications to cause QTc prolongation found that aripiprazole was the clear favorite. So that would be preferred over drugs like quetiapine, for example, which has quite high QTc prolongation. Lurasidone was not reviewed at the time by Chung and colleagues but that also seems to have low QTc prolongation although it is not approved for treatment of bipolar mania.
References:
- Chung, A. K., & Chua, S. E. (2011). Effects on prolongation of Bazett’s corrected QT interval of seven second-generation antipsychotics in the treatment of schizophrenia: a meta-analysis. Journal of psychopharmacology, 25(5), 646-666.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 10
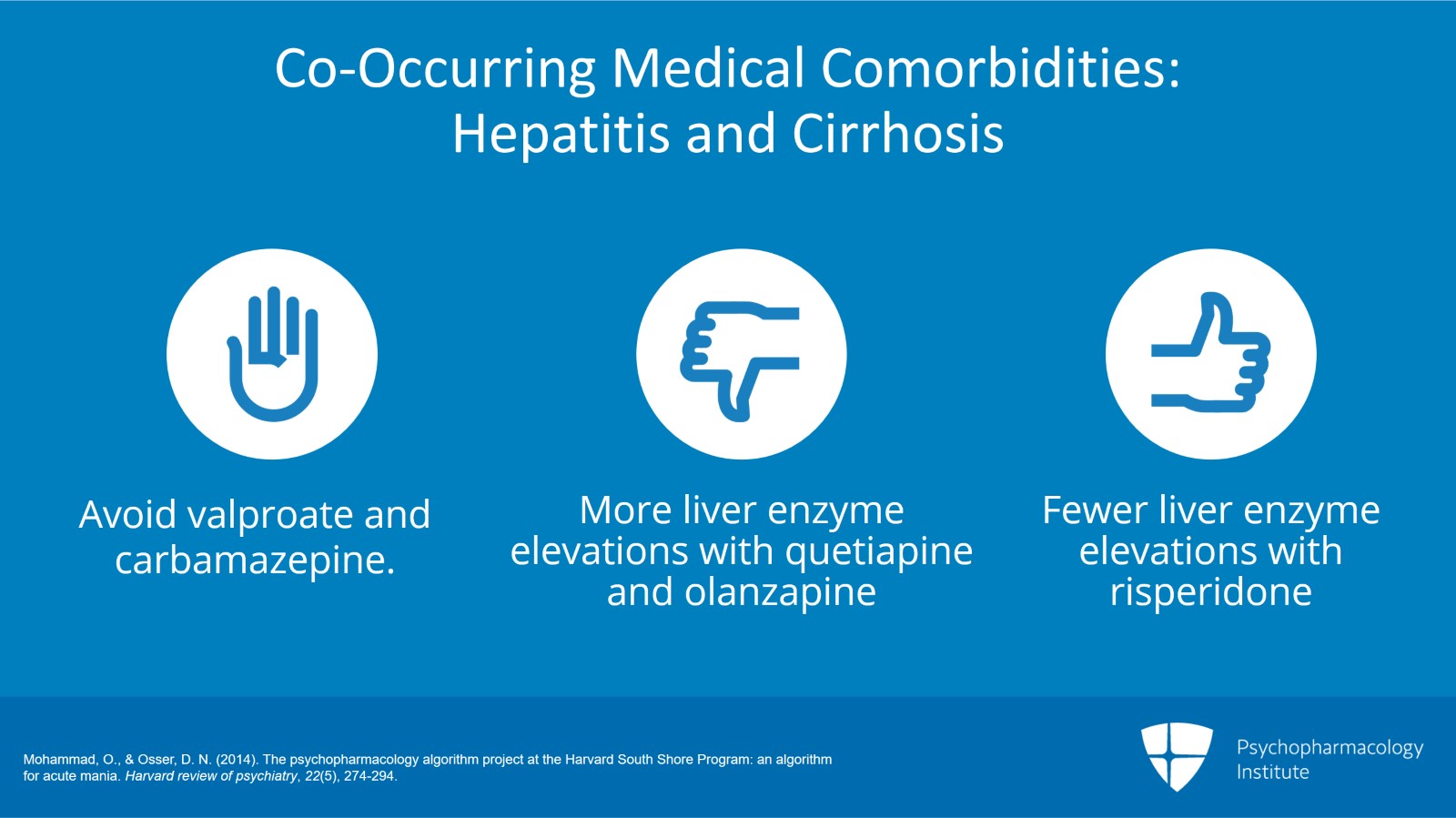
Another medical comorbidity of concern is hepatitis and cirrhosis. You probably should avoid valproate and carbamazepine in that situation. Among the atypical antipsychotics, the ones with the most liver function test elevations are quetiapine and olanzapine. Lesser elevations are seen with risperidone and some of the others.
References:
- Mohammad, O., & Osser, D. N. (2014). The psychopharmacology algorithm project at the Harvard South Shore Program: an algorithm for acute mania. Harvard review of psychiatry, 22(5), 274-294.
Slide 6 of 10
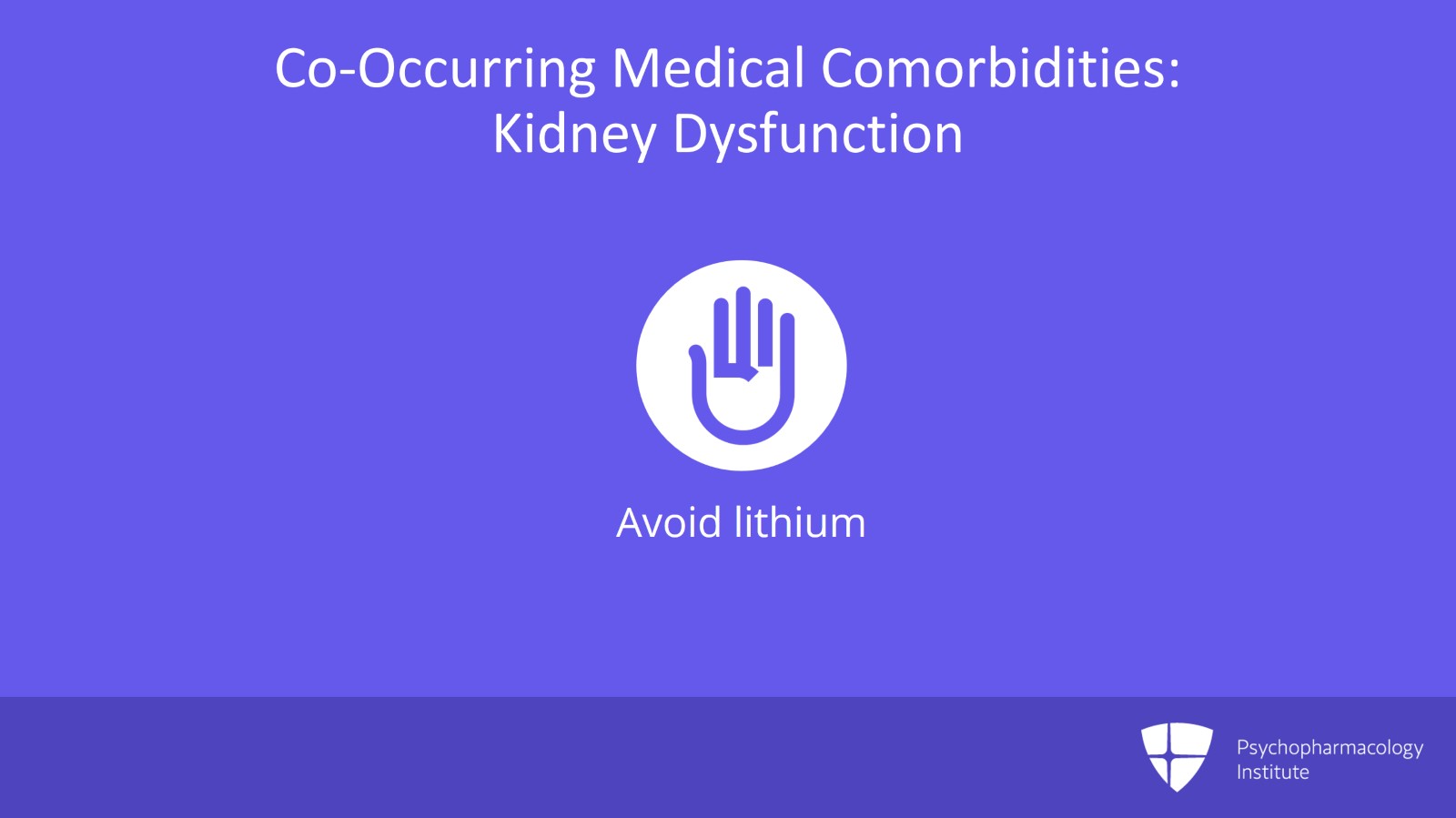
Then there are patients with renal filtration problems, kidney dysfunction. You probably need to avoid lithium for them.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 10
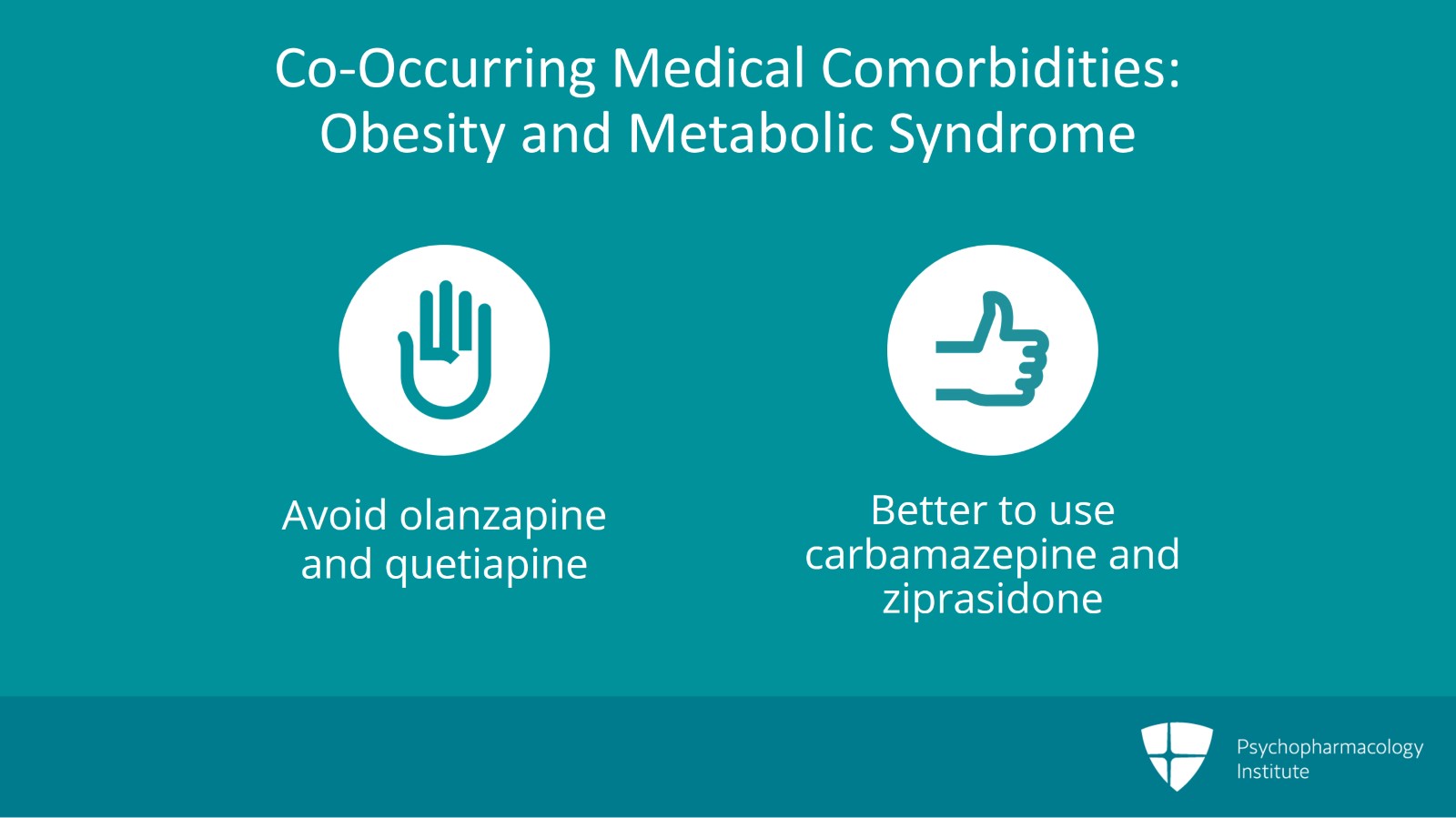
And finally, there are people with obesity, metabolic syndrome, a very common problem that you encounter. You probably want to avoid the worst offenders of olanzapine and quetiapine. The best options in terms of not causing weight gain would be carbamazepine and ziprasidone.
Slide 8 of 10
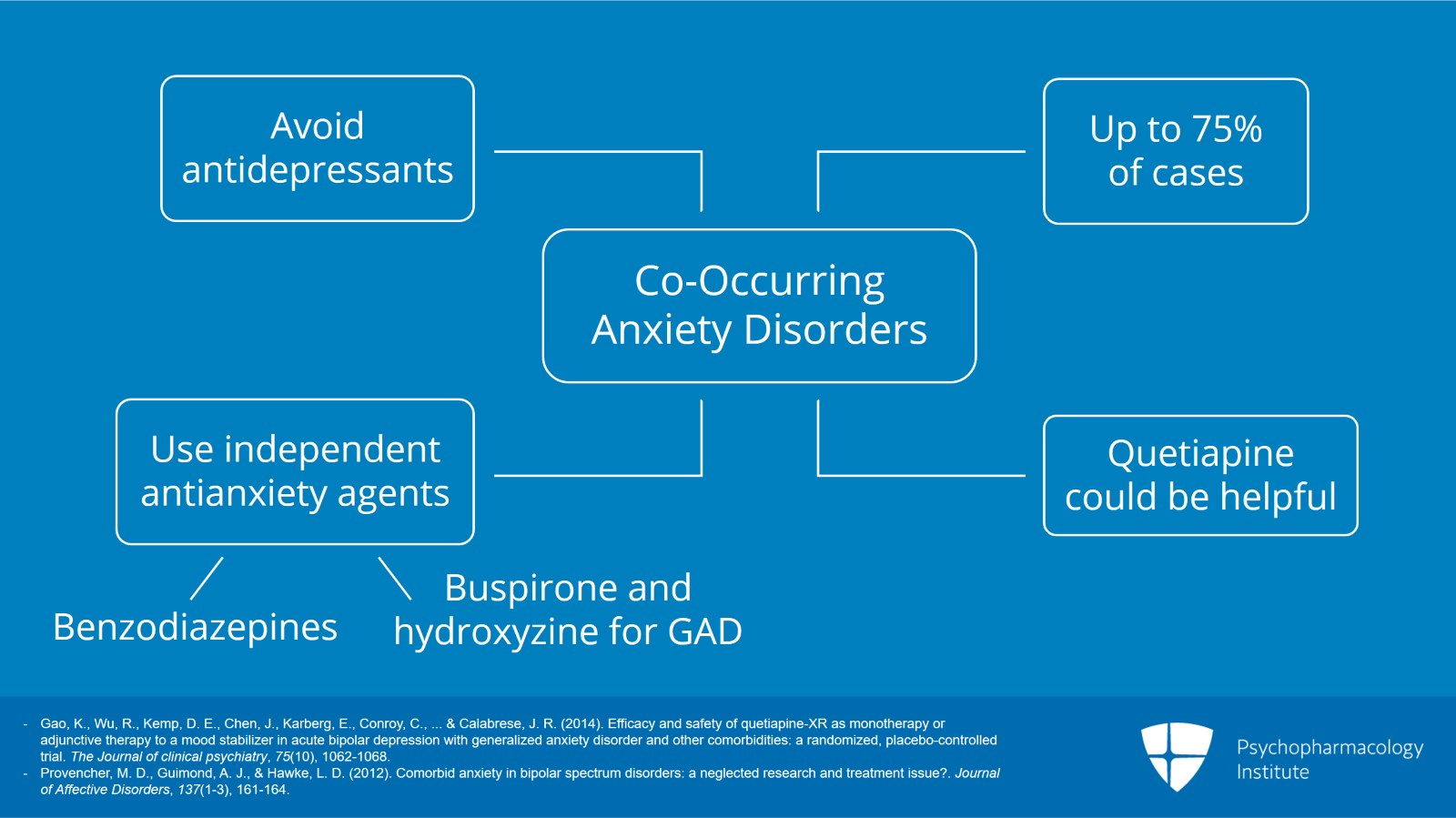
Finally, there are anxiety disorders. They are also very commonly comorbid with bipolar mania. In fact, up to 75% of patients with mania may have significant anxiety symptoms. And studies have suggested that their prognosis is reduced compared to the few that don’t have anxiety. So what can you do for that anxiety? Well, antidepressants, certainly controversial at best to be adding an antidepressant for anxiety in a patient with mania. We recommend against it even though we see some people continuing antidepressants in such patients hoping that that’s somehow going to help with the anxiety. You might think of using quetiapine among the antipsychotics because that actually has been studied in generalized anxiety disorder and found to be better than placebo. Should you pick it especially for manic patients who are anxious? Maybe but we don’t have strong support for it. We would say that probably the helpful approach might be to pick an independent anti-anxiety agent that’s not an antidepressant. So that could include benzodiazepines, if appropriate in people who are not substance abusers. Buspirone and hydroxyzine for generalized anxiety disorder at least might have a role.
References:
- Gao, K., Wu, R., Kemp, D. E., Chen, J., Karberg, E., Conroy, C., … & Calabrese, J. R. (2014). Efficacy and safety of quetiapine-XR as monotherapy or adjunctive therapy to a mood stabilizer in acute bipolar depression with generalized anxiety disorder and other comorbidities: a randomized, placebo-controlled trial. The Journal of clinical psychiatry, 75(10), 1062-1068.
- Provencher, M. D., Guimond, A. J., & Hawke, L. D. (2012). Comorbid anxiety in bipolar spectrum disorders: a neglected research and treatment issue?. Journal of Affective Disorders, 137(1-3), 161-164.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 10
So in summary for video 3, for co-occurring diagnoses and conditions that we discussed, if there’s emerging agitation in mania requiring intramuscular treatment, we recommend haloperidol plus a benzodiazepine. That’s still the most effective with the least side effects. For the various medical comorbidities we discussed in this lesson, the one that comes up perhaps the most often is “what can I give that has the least weight gain?” and ziprasidone and carbamazepine would lead the list for considering that taking into account cost effectiveness as well. And comorbid anxiety may be managed with benzodiazepines. Buspirone and hydroxyzine may sometimes help.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.