Slides and Transcript
Slide 1 of 11
Next in our discussion is childhood and adolescent bipolar depression. As we know, the reason why this is called bipolar disorder is because it has two poles for this mood disorder. You have the depressive episodes and you have the manias and the hypomanias.
Slide 2 of 11
Now, people with bipolar disorder as well-known spend roughly two-thirds of the time of their illness in depression. And this is why most of the struggle in life in someone with bipolar disorder is a struggle with depression.
Like adult literature as we talk about children with this condition, the data on effective treatment for bipolar depression unfortunately is not that available. Treatment of bipolar depression is a clinical challenge in children the way it is with adults. And this is due to a number of factors which I’ll try to summarize here.
*References*
References:
- Judd, L. L., & Akiskal, H. S. (2003). The prevalence and disability of bipolar spectrum disorders in the US population: re-analysis of the ECA database taking into account subthreshold cases. Journal of affective disorders, 73(1-2), 123-131.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 11
The first challenge from a clinical standpoint is the risk of switching to mania or acceleration of cycling of the mood episodes, the two poles whether the depression or the mania, when we use antidepressants which in turn in themselves have a questionable efficacy in bipolar depression per se.
Now, although there is possibly less switching when using certain medications such as more serotonergic agents more than noradrenergic agents, so using the SSRI, for example, it would be better than using a tricyclic antidepressant or an SNRI.
Switching is more common in antidepressants in general even though SSRIs might seem a little better option. But switching is more common in children and young adults than in older adults.
*References*
References:
- Tondo, L., Vázquez, G., & Baldessarini, R. J. (2010). Mania associated with antidepressant treatment: comprehensive meta‐analytic review. Acta Psychiatrica Scandinavica, 121(6), 404-414.
Slide 4 of 11
The second clinical challenge and aspect of the treatment of bipolar depression in the youth is that with the exception of lithium and quetiapine which can be effective as monotherapies there is often a need to use polypharmacy and combine medications together. Now, that in itself imposes an increased risk of childhood obesity and diabetes with this combination, say for example, of an atypical antipsychotic with an SSRI.
*References*
References:
- Detke, H. C., DelBello, M. P., Landry, J., & Usher, R. W. (2015). Olanzapine/Fluoxetine combination in children and adolescents with bipolar I depression: a randomized, double-blind, placebo-controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry, 54(3), 217-224.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 11
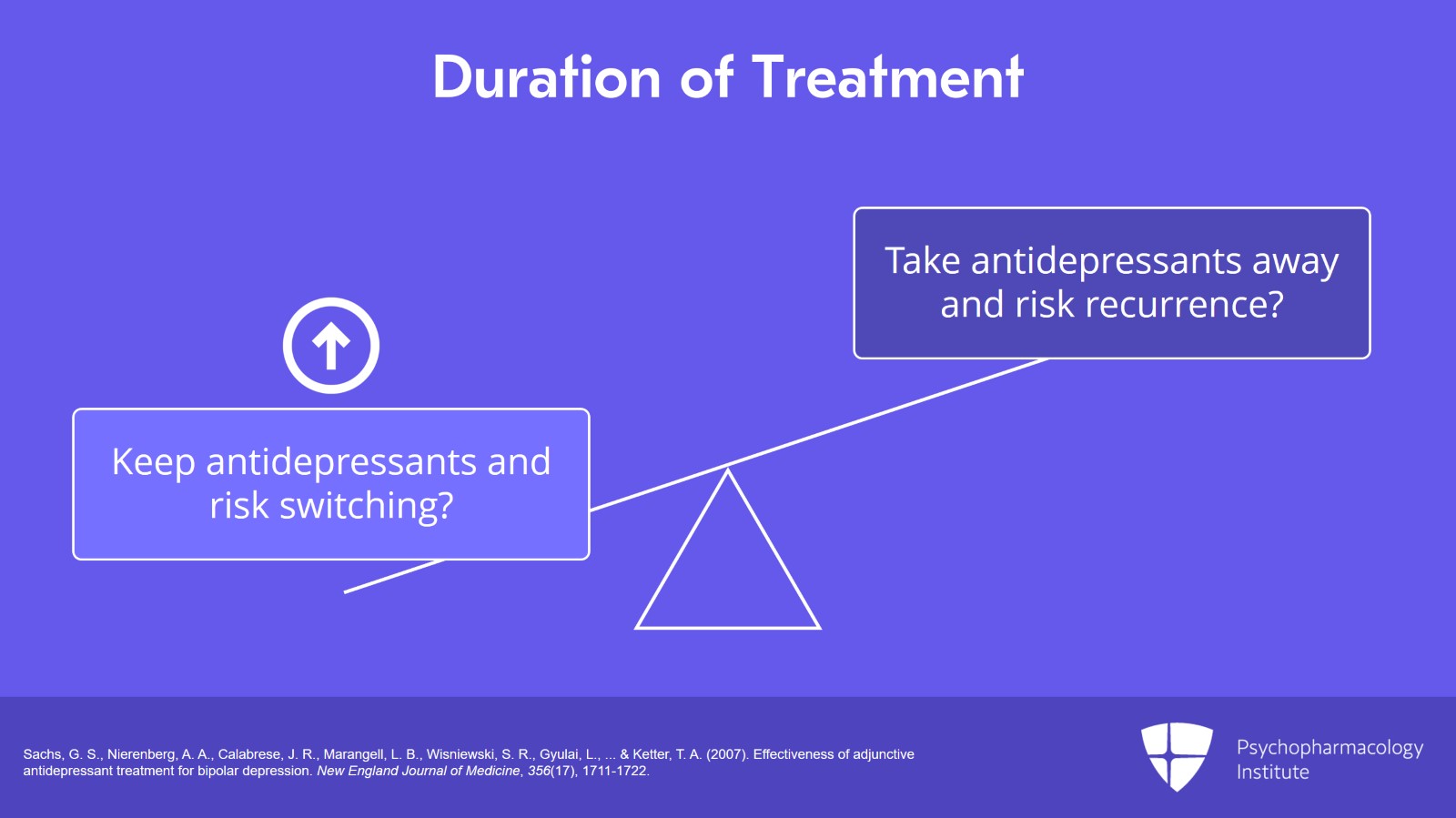
The third clinical challenge is that there is a lack of clear guideline as to how long to keep antidepressants on board for someone with bipolar depression especially after symptoms resolve. Do we keep the SSRIs on, for example? Or do we take them away? And this, mind you, is an important thing to keep in mind just because of the risk of switching and this in itself as we said is a little more frequent in the youth more than adults.
Hence, we have to discuss the pros and cons of keeping an antidepressant medication with the clear advent of helping depressed mood versus taking it away and risking a recurrence of the depressive episode.
*References*
References:
- Sachs, G. S., Nierenberg, A. A., Calabrese, J. R., Marangell, L. B., Wisniewski, S. R., Gyulai, L., … & Ketter, T. A. (2007). Effectiveness of adjunctive antidepressant treatment for bipolar depression. New England Journal of Medicine, 356(17), 1711-1722.
Slide 6 of 11
What are some of the agents that are worth considering in childhood bipolar depression?
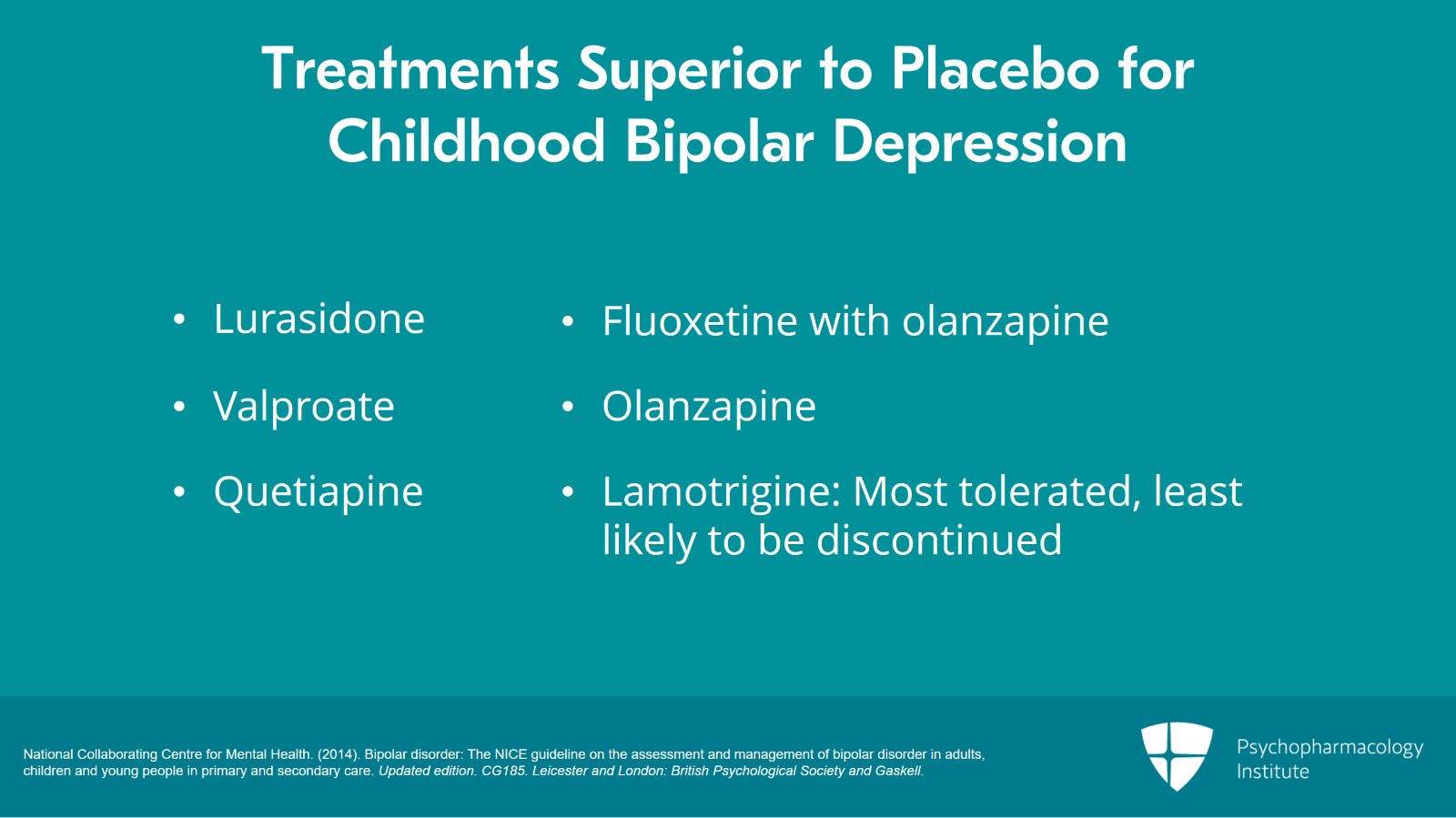
In the NICE Guidelines, there was a meta-analysis of pharmacological interventions that met criteria to be included in analysis. Those are the studies that met the burden that the NICE Network set as a standard for their analysis. They found that there are only six treatments that have superiority to placebo including lurasidone, valproate, quetiapine, fluoxetine with olanzapine, olanzapine alone and lamotrigine. Interestingly, valproate was received by the lowest number of people in the analysis. And lamotrigine was the most tolerated and the least likely to be discontinued.
*References*
References:
- National Collaborating Centre for Mental Health. (2014). Bipolar disorder: The NICE guideline on the assessment and management of bipolar disorder in adults, children and young people in primary and secondary care. Updated edition. CG185. Leicester and London: British Psychological Society and Gaskell.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 11
Imipramine, lithium, moclobemide, paroxetine and ziprasidone were actually not superior to placebo.
*References*
References:
- National Collaborating Centre for Mental Health. (2014). Bipolar disorder: The NICE guideline on the assessment and management of bipolar disorder in adults, children and young people in primary and secondary care. Updated edition. CG185. Leicester and London: British Psychological Society and Gaskell.
Slide 8 of 11
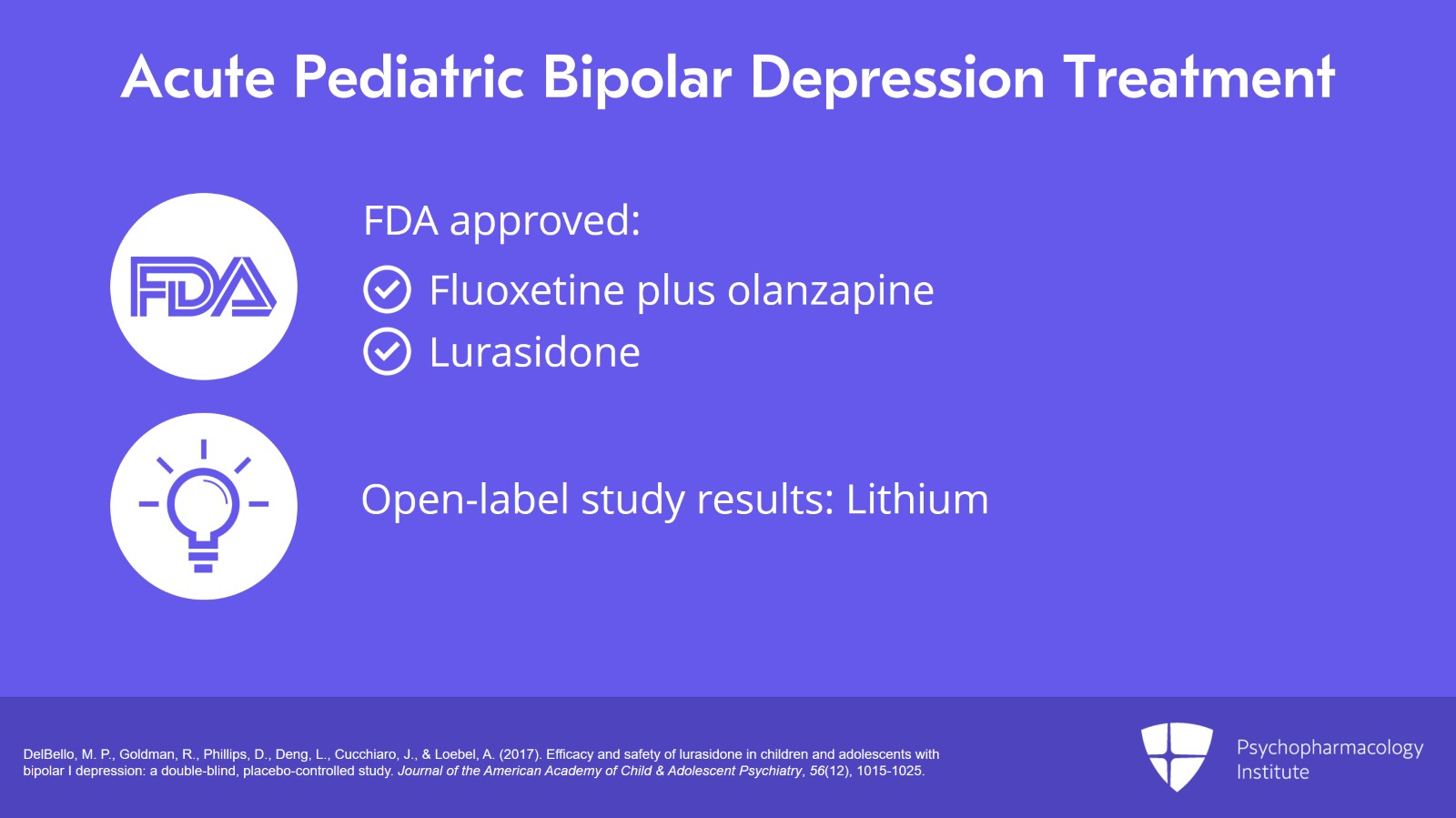
It is worth noting that only fluoxetine plus olanzapine in combination and lurasidone are FDA approved for treatment of acute pediatric bipolar depression.
It is important to note that the data we have on lithium for off-label treatment of bipolar depression is based on open label study, not randomized controlled trial.
*References*
References:
- DelBello, M. P., Goldman, R., Phillips, D., Deng, L., Cucchiaro, J., & Loebel, A. (2017). Efficacy and safety of lurasidone in children and adolescents with bipolar I depression: a double-blind, placebo-controlled study. Journal of the American Academy of Child & Adolescent Psychiatry, 56(12), 1015-1025.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 11
So how effective is lithium for bipolar depression?
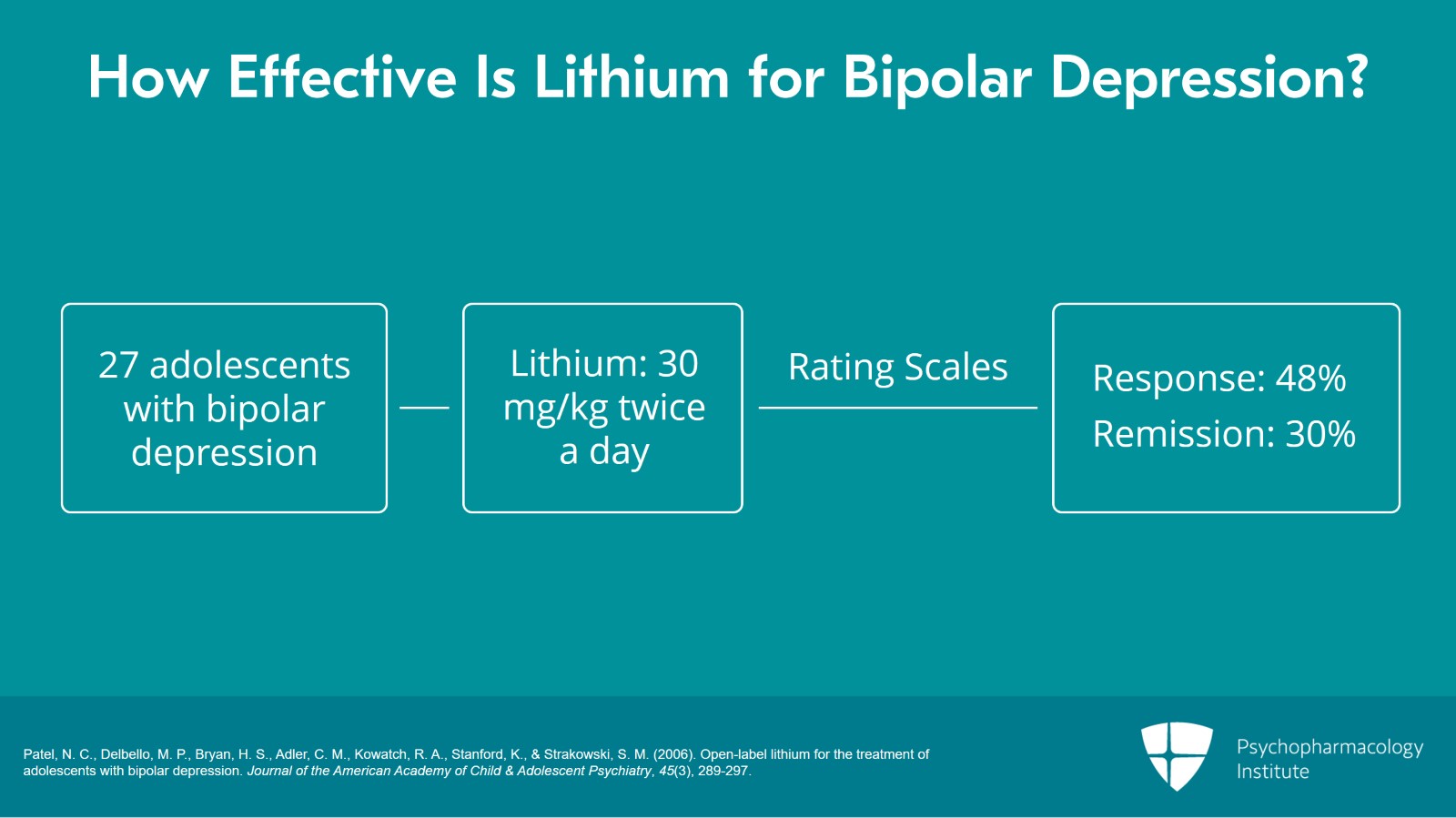
In a study that included 27 adolescents with an episode of depression with a bipolar disorder diagnosis, it was an open label study that gave 30 mg/kg of lithium twice a day and they adjusted the dose to therapeutic serum level of lithium of 1.0 to 1.2 mEq/L. To check for the effectiveness of this intervention, they included rating scales such as the Children’s Depression Rating Scale, the revised version, and the Clinical Global Impression Scale for Bipolar Disorder.
What were the results? The results showed that scores significantly decreased from baseline to endpoint resulting in a large effect size of 1.7. Response and remission rates both seemed to be better. For the response, it was roughly about 48%. And for the remission, it was roughly about 30% of this patient population.
*References*
References:
- Patel, N. C., Delbello, M. P., Bryan, H. S., Adler, C. M., Kowatch, R. A., Stanford, K., & Strakowski, S. M. (2006). Open-label lithium for the treatment of adolescents with bipolar depression. Journal of the American Academy of Child & Adolescent Psychiatry, 45(3), 289-297.
Slide 10 of 11
To summarize, bipolar depression is equally, if not more challenging of a condition to treat in children than adults with bipolar depression.
The second point is only two FDA-approved agents are there and these are namely lurasidone and olanzapine plus fluoxetine.
The third take home point is that lithium might be very effective and should be seriously considered as an option although this continues to be in need for more evidence from research in this population.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.