Slides and Transcript
Slide 1 of 10
So we’ve talked about how to understand these three different mood syndromes, how to assess and diagnose them and how to treat them. Let’s return to our case vignette, our case of Mary C.
Slide 2 of 10
She’s our 27-year-old single woman who comes in after having been on oral contraceptive pills for many years, going off them and experiencing some severe symptoms in the premenstrual period.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 10
After a complete evaluation, you educate Mary C. about PMS and PMDD in that first visit and you explained to her why you need prospective charting to diagnose.
You educate her about lifestyle modifications and using vitamin and herbal supplements.
And then you give her a rating chart and set a followup appointment for the next month. You give her preliminary information about treatment with SSRIs and oral contraceptives.
References:
- National Curriculum in Reproductive Psychiatry http://ncrptraining.org
Slide 4 of 10
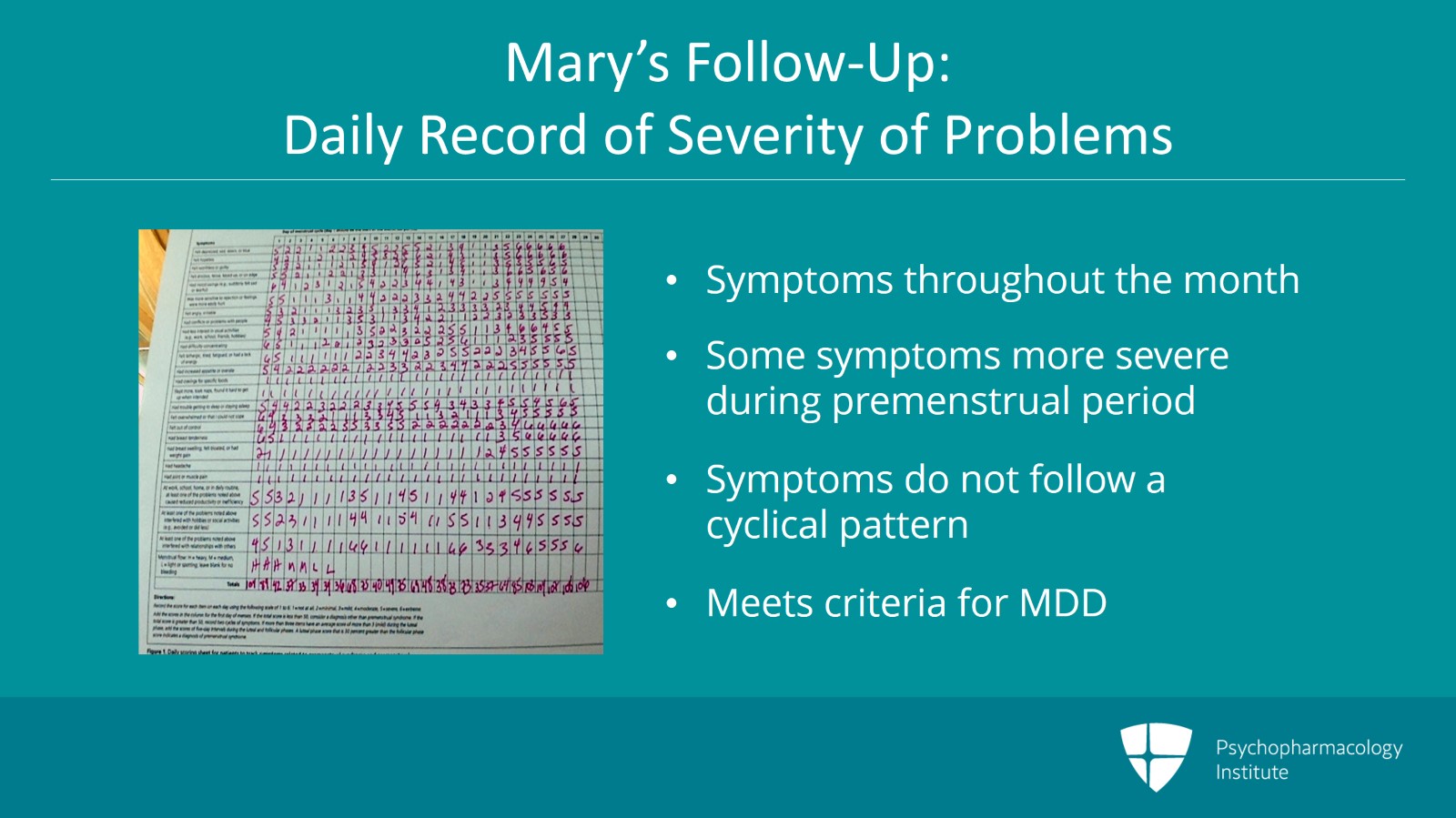
When she returns in a month, she presents the following mood tracker. You remember the Daily Record of Severity of Problems that we talked about earlier. Well, as you can see from this mood tracker, Mary has symptoms throughout the entire month. You can see that there are many symptoms that she doesn’t experience at all such as the ones that are marked with a number 1 going all the way across the month and that there definitely are symptoms that are more severe in the premenstrual period.
She has a lot of 5’s and 6’s in the premenstrual weeks. But you can also see that Mary has symptoms that are present, some of them severe throughout the month.
What that means is that her symptoms actually do not present a typical cyclical pattern. They are worse in the premenstrual period but they’re also present in other times of the month.
In addition, for a complete clinical interview, you realized that she meets criteria for a major depressive episode using DSM-5 criteria. So what does that mean? What does Mary have? Does she have PMS, PMDD or PME?
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 10
The answer is PME. She has premenstrual exacerbation of an existing mood disorder.
This syndrome is seen in women who have a mood disorder. It could be major depressive disorder or bipolar disorder who are not clinically stable. Their mood will worsen during the luteal phase. It’s often accompanied by irritability and you can think of it as PMS in addition to a mood disorder.
It is not well studied. There’s very little evidence about this but it may be a marker for difficult to treat or a worse course of illness in mood disordered women. Because it’s not very well studied, we don’t have any treatment studies that apply specifically to PME. So we must rely on clinical experience.
References:
- Yonkers, K. A., O'Brien, P. S., & Eriksson, E. (2008). Premenstrual syndrome. The Lancet, 371(9619), 1200-1210.
Slide 6 of 10
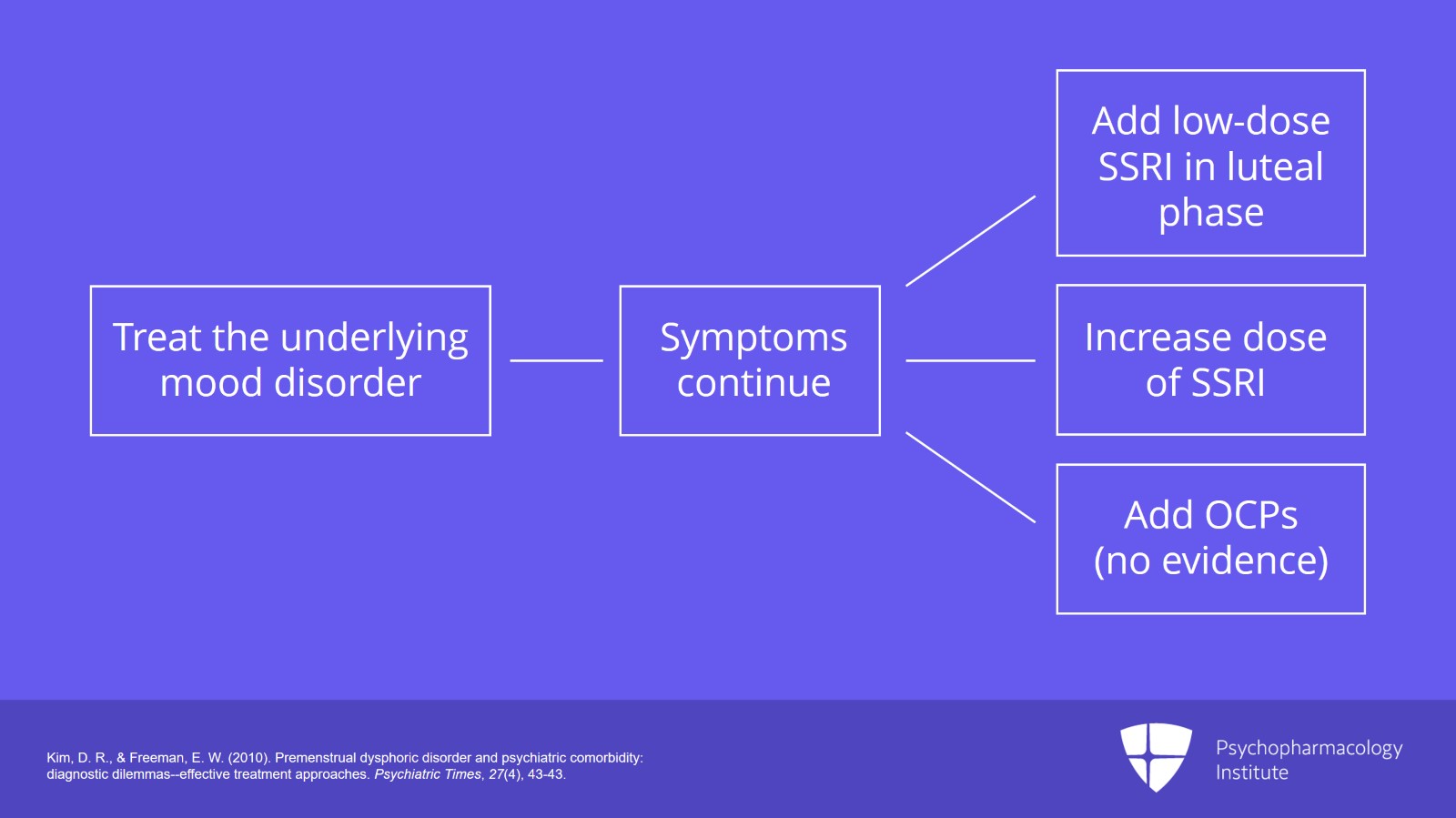
The most important thing to do is to treat the underlying mood disorder. You’ll want to use an evidence-based treatment for the mood disorder she has.
So if she has bipolar II, for example, she’s going to need a mood stabilizer, not an antidepressant.
For many patients, those premenstrual symptoms will disappear once the mood disorder is sufficiently treated.
For those women who continue to have premenstrual symptoms after you’ve treated the underlying mood disorder, you can add a low-dose serotonergic agent in the luteal phase only or increase her dose if that’s what she’s already taking or you can add an oral contraceptive pill although again as we’ve seen in the previous part of this video, we don’t have evidence that oral contraceptive pills will actually help women who have PME.
References:
- Kim, D. R., & Freeman, E. W. (2010). Premenstrual dysphoric disorder and psychiatric comorbidity: diagnostic dilemmas–effective treatment approaches. Psychiatric Times, 27(4), 43-43.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 10
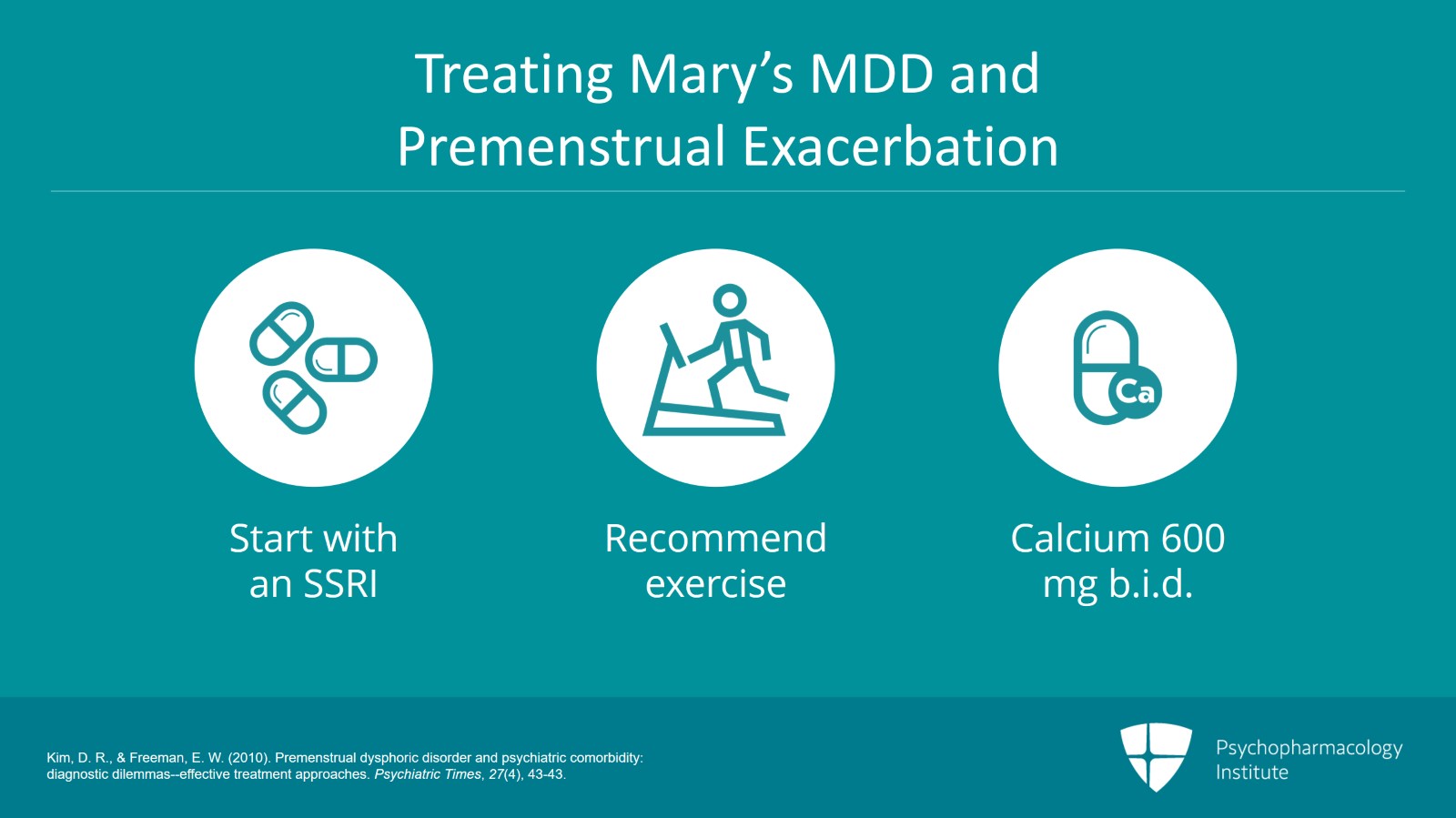
So in this particular case, what are we going to do with Mary C.? We’ve determined that she has major depressive disorder and that she has premenstrual worsening. How are we going to treat her?
Well, SSRI is the first-line treatment here because she appears to have MDD with premenstrual exacerbation. Lifestyle and complementary treatments may help as well.
So the clinician may also recommend exercise and calcium 600 mg b.i.d.
The choice of SSRI will depend on the patient’s personal and family history of SSRI use as well as any preferences concerning side effects and rapidity of titration.
References:
- Kim, D. R., & Freeman, E. W. (2010). Premenstrual dysphoric disorder and psychiatric comorbidity: diagnostic dilemmas–effective treatment approaches. Psychiatric Times, 27(4), 43-43.
Slide 8 of 10
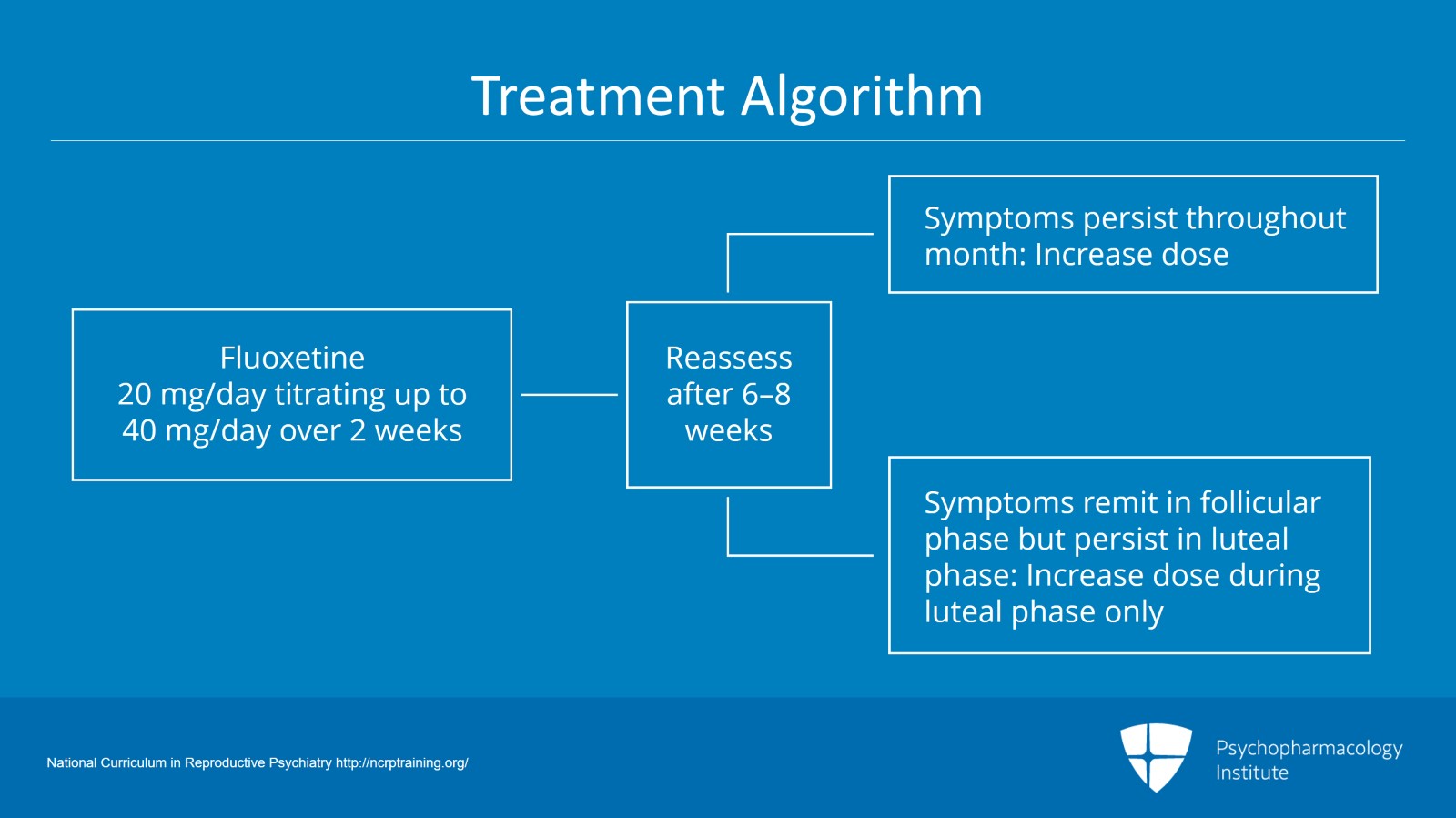
In this case, the physician chooses to start fluoxetine 20 mg titrating up to 40 mg over a period of two weeks. The clinician will reassess mood after six to eight weeks on this dose.
If the medication is helping but there are still some symptoms throughout the month, the dose should be raised.
If symptoms in the follicular phase have remitted but there are still some symptoms in the luteal phase, the physician may elect to increase the dosage in the luteal phase only if that’s what the patient prefers either by starting at ovulation or at the day of symptom onset.
The patient should be seen ideally biweekly or at a minimum monthly through the titration phase with a decrease in frequency once stability is achieved.
References:
- National Curriculum in Reproductive Psychiatry http://ncrptraining.org/
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 10
Key points of this section. For women who have PME or premenstrual exacerbation of an underlying mood disorder, it’s important to treat the underlying mood disorder to remission first.
The choice of which SSRI to use depends on patient history and preference. Evidence will support the use of most SSRIs for this so it really doesn’t matter from an evidence base which one you use for treating the disorder.
If the mood disorder remits during the follicular phase but the patient is still symptomatic in the luteal phase, you can add luteal phase dosing, if she’s already taking an SSRI by increasing the dose during the luteal phase, if she’s not already taking one by adding a small dose during luteal phase only.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.