Slides and Transcript
Slide 1 of 14
In this next section, we’re going to talk about antipsychotics and their association with QT prolongation…
Slide 2 of 14
…and we’ll start by talking about first generation antipsychotics. So the low potency phenothiazines which include medications like thioridazine, chlorpromazine and mesoridazine are the first-generation antipsychotics that are most associated with QT prolongation. And as a class, first-generation antipsychotics are linked to greater QT prolongation than are second generation agents. But it’s important to recognize that this effect is primarily driven by those low potency phenothiazines. In terms of their risk for torsade, the difference between first and second generation antipsychotics does not appear to be statistically significant.
References:
- Carrà, G., Crocamo, C., Bartoli, F., Lax, A., Tremolada, M., Lucii, C., … & Castellazzi, M. (2016). First‐generation antipsychotics and QTc: any role for mediating variables?. Human Psychopharmacology: Clinical and Experimental, 31(4), 313-318.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 14
In addition to the low potency phenothiazines, the other first generation antipsychotic that is most commonly associated with QT prolongation is haloperidol. The association of haloperidol with QT prolongation though remains somewhat controversial. A recent meta-analysis found that the effects of haloperidol on the QT interval are actually very similar to several second generation antipsychotic agents. That being said, there are other studies that suggest a greater risk for ventricular arrhythmias or sudden cardiac death with haloperidol.
References:
- Carrà, G., Crocamo, C., Bartoli, F., Lax, A., Tremolada, M., Lucii, C., … & Castellazzi, M. (2016). First‐generation antipsychotics and QTc: any role for mediating variables?. Human Psychopharmacology: Clinical and Experimental, 31(4), 313-318.
Slide 4 of 14
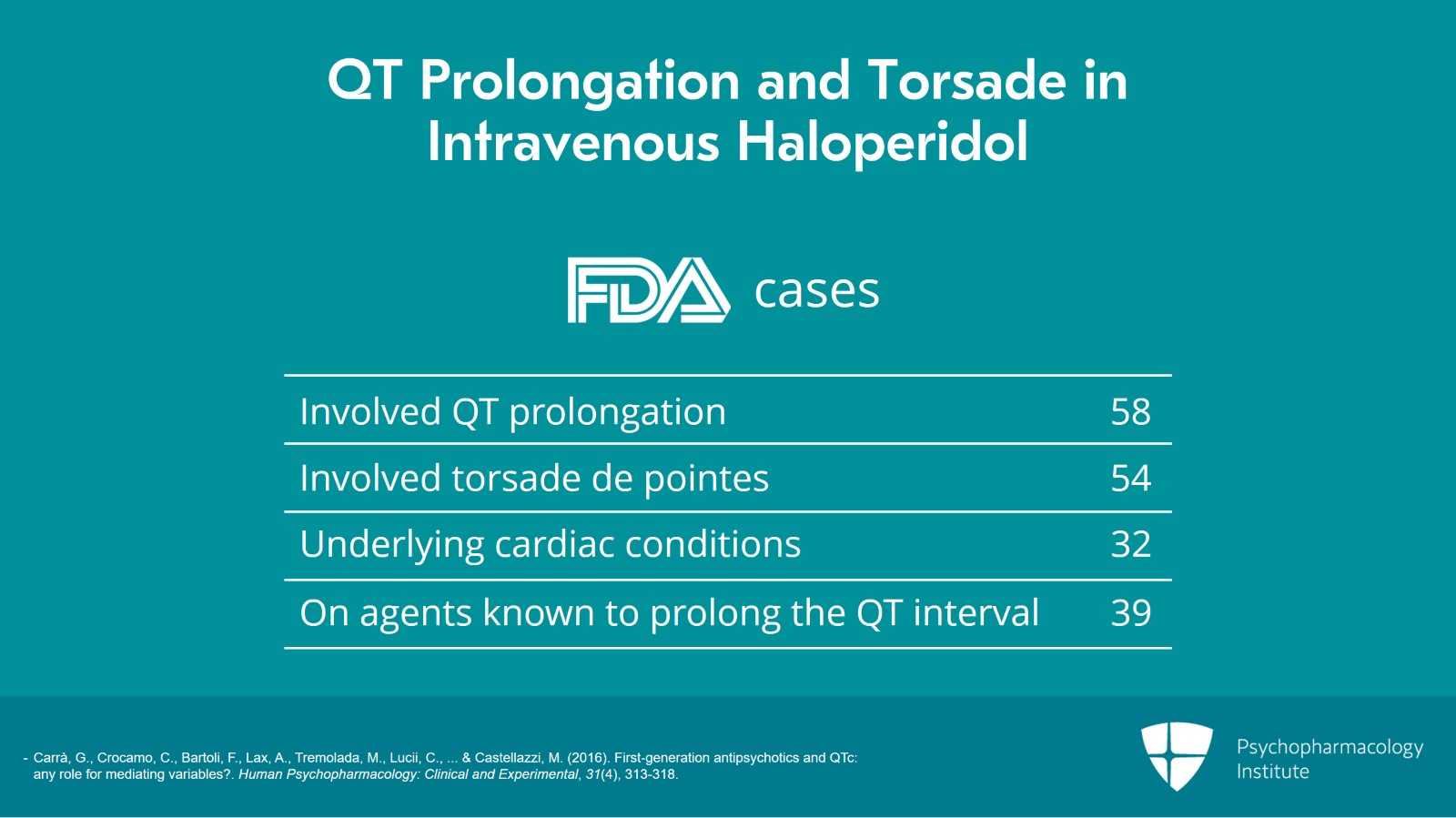
One of the forms of haloperidol that has been most associated with QT prolongation and torsade is the intravenous form. There had been 70 cases total reported to the FDA; 58 of those involved QT prolongation; 54 of those involved torsade de pointes. It’s important to recognize though that almost all of those cases had other significant risk factors for QT prolongation. Thirty-two of the patients had underlying cardiac conditions and 39 were on other agents that are known to prolong the QT interval. So the association of intravenous haloperidol with QT prolongation or torsade does remain somewhat controversial and there is not strong evidence that intravenous haloperidol separates out from oral or intramuscular haloperidol.
References:
- Carrà, G., Crocamo, C., Bartoli, F., Lax, A., Tremolada, M., Lucii, C., … & Castellazzi, M. (2016). First‐generation antipsychotics and QTc: any role for mediating variables?. Human Psychopharmacology: Clinical and Experimental, 31(4), 313-318.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 14
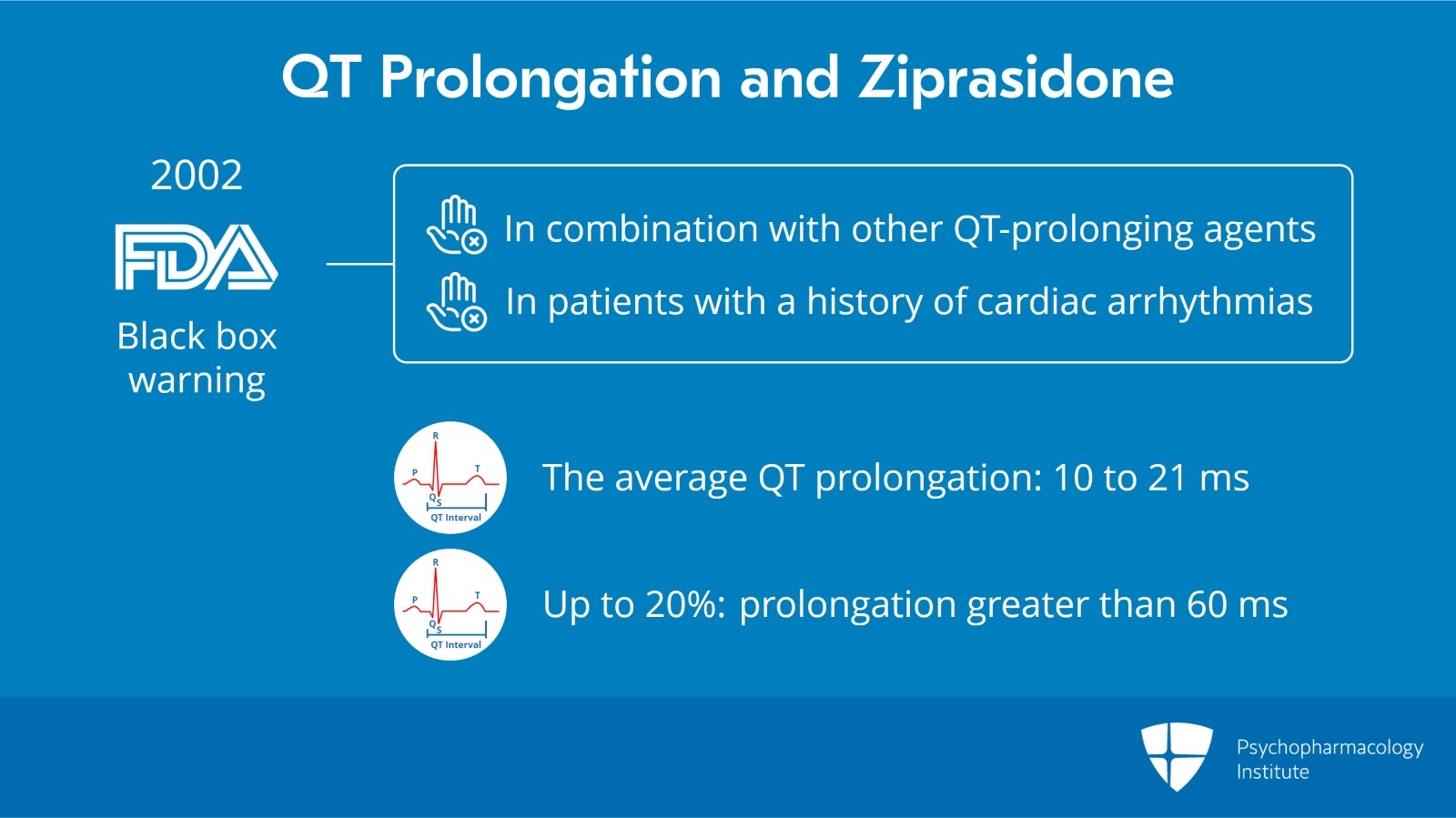
With regard to second generation antipsychotics, ziprasidone is the agent that most people associate with QT prolongation. In 2002, the FDA issued a black box warning for ziprasidone urging prescribers to avoid use in combination with other QT prolonging agents or in patients with a history of cardiac arrhythmias. The average QT prolongation with ziprasidone is somewhere between 10 ms to 21 ms but up to 20% of patients experience an increase greater than 60 ms.
Slide 6 of 14
And in a meta-analysis that compared all of the second generation antipsychotics as well as a couple of the first generation antipsychotics, ziprasidone actually performed the worst in that study. It was similar to iloperidone but slightly worse.
References:
- Leucht, S., Cipriani, A., Spineli, L., Mavridis, D., Örey, D., Richter, F., … & Kissling, W. (2013). Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. The Lancet, 382(9896), 951-962
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 14
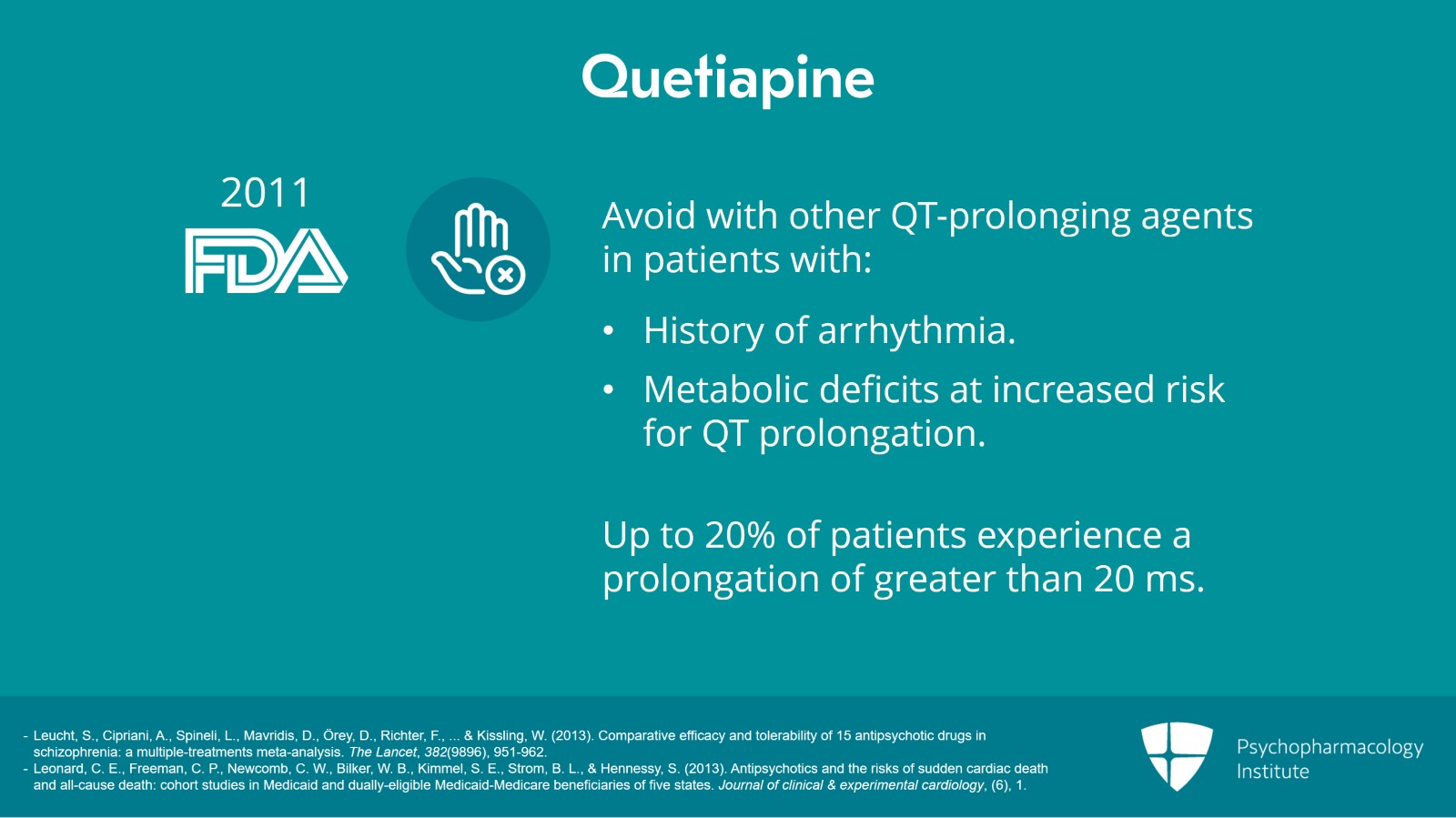
Another agent that’s sometimes highlighted in this discussion is quetiapine and that’s because in 2011 the FDA strengthened the warning around quetiapine and recommended that it be avoided in use with other QT prolonging agents in patients with a history of arrhythmia or in patients with metabolic deficits who may be at increased risk for QT prolongation.
In general, it’s felt to have relatively mild effects though there is some suggestion that up to 20% of patients experience a prolongation of greater than 20 ms which is considered more clinically significant.
References:
- Leucht, S., Cipriani, A., Spineli, L., Mavridis, D., Örey, D., Richter, F., … & Kissling, W. (2013). Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. The Lancet, 382(9896), 951-962.
- Leonard, C. E., Freeman, C. P., Newcomb, C. W., Bilker, W. B., Kimmel, S. E., Strom, B. L., & Hennessy, S. (2013). Antipsychotics and the risks of sudden cardiac death and all-cause death: cohort studies in Medicaid and dually-eligible Medicaid-Medicare beneficiaries of five states. Journal of clinical & experimental cardiology, (6), 1.
Slide 8 of 14
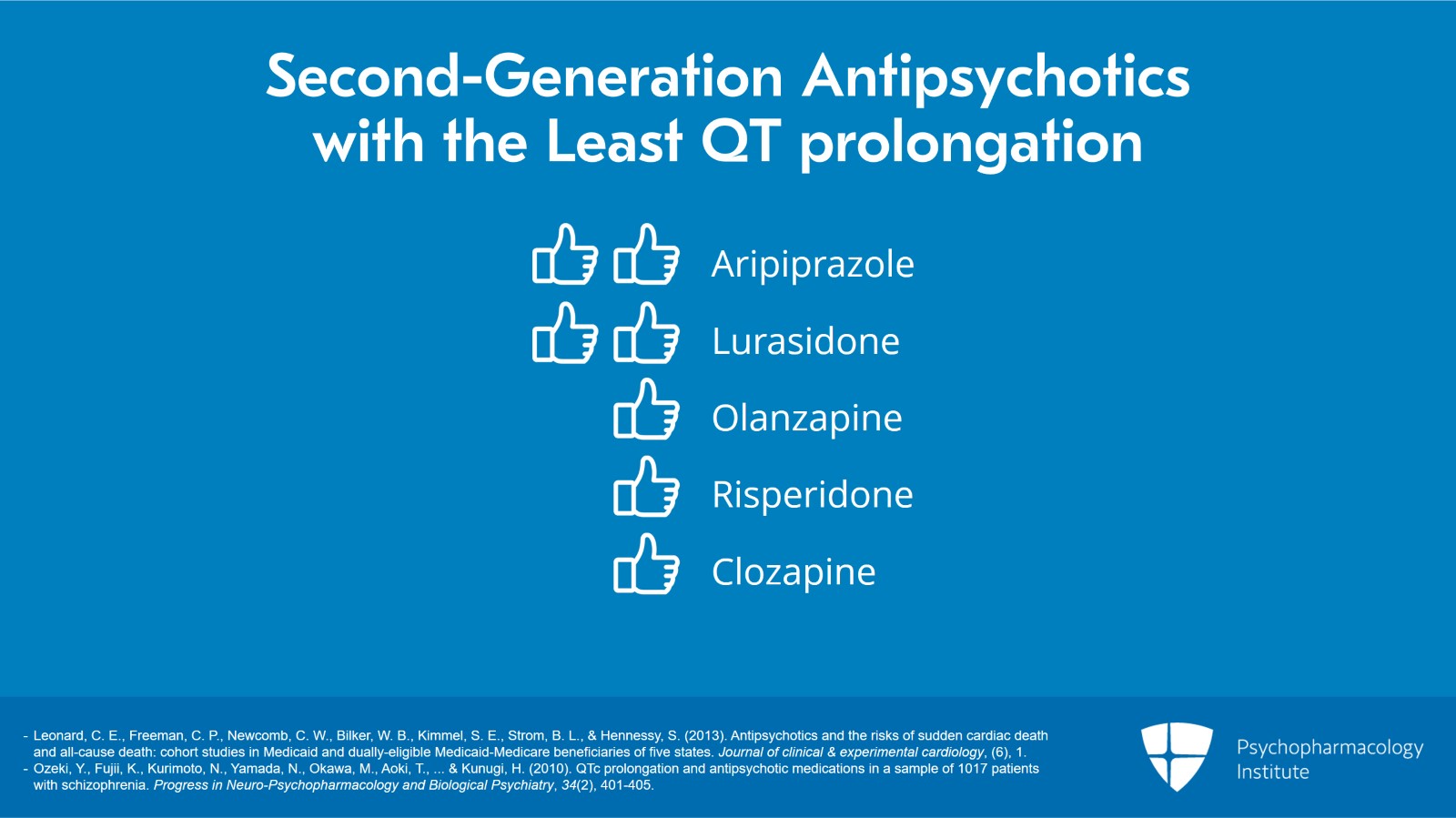
Among the second generation antipsychotics and really among antipsychotics as a whole, the agents that performed best from the standpoint of QT prolongation appeared to be aripiprazole and lurasidone. Most other antipsychotics can’t really be separated out from one another and end up somewhere in the middle of the pack and these include olanzapine, risperidone and clozapine.
References:
- Leonard, C. E., Freeman, C. P., Newcomb, C. W., Bilker, W. B., Kimmel, S. E., Strom, B. L., & Hennessy, S. (2013). Antipsychotics and the risks of sudden cardiac death and all-cause death: cohort studies in Medicaid and dually-eligible Medicaid-Medicare beneficiaries of five states. Journal of clinical & experimental cardiology, (6), 1.
- Ozeki, Y., Fujii, K., Kurimoto, N., Yamada, N., Okawa, M., Aoki, T., … & Kunugi, H. (2010). QTc prolongation and antipsychotic medications in a sample of 1017 patients with schizophrenia. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 34(2), 401-405.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 14
Another issue that has generated some inquiry in the recent past is the idea about whether polypharmacy with multiple antipsychotics leads to greater QT prolongation. There are unclear conclusions regarding that but there’s speculation that if that is true it’s probably mediated by the total cumulative dose or the total cumulative relative dose rather than by the fact that the patient is on multiple different agents.
References:
- Leonard, C. E., Freeman, C. P., Newcomb, C. W., Bilker, W. B., Kimmel, S. E., Strom, B. L., & Hennessy, S. (2013). Antipsychotics and the risks of sudden cardiac death and all-cause death: cohort studies in Medicaid and dually-eligible Medicaid-Medicare beneficiaries of five states. Journal of clinical & experimental cardiology, (6), 1.
- Ozeki, Y., Fujii, K., Kurimoto, N., Yamada, N., Okawa, M., Aoki, T., … & Kunugi, H. (2010). QTc prolongation and antipsychotic medications in a sample of 1017 patients with schizophrenia. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 34(2), 401-405.
Slide 10 of 14
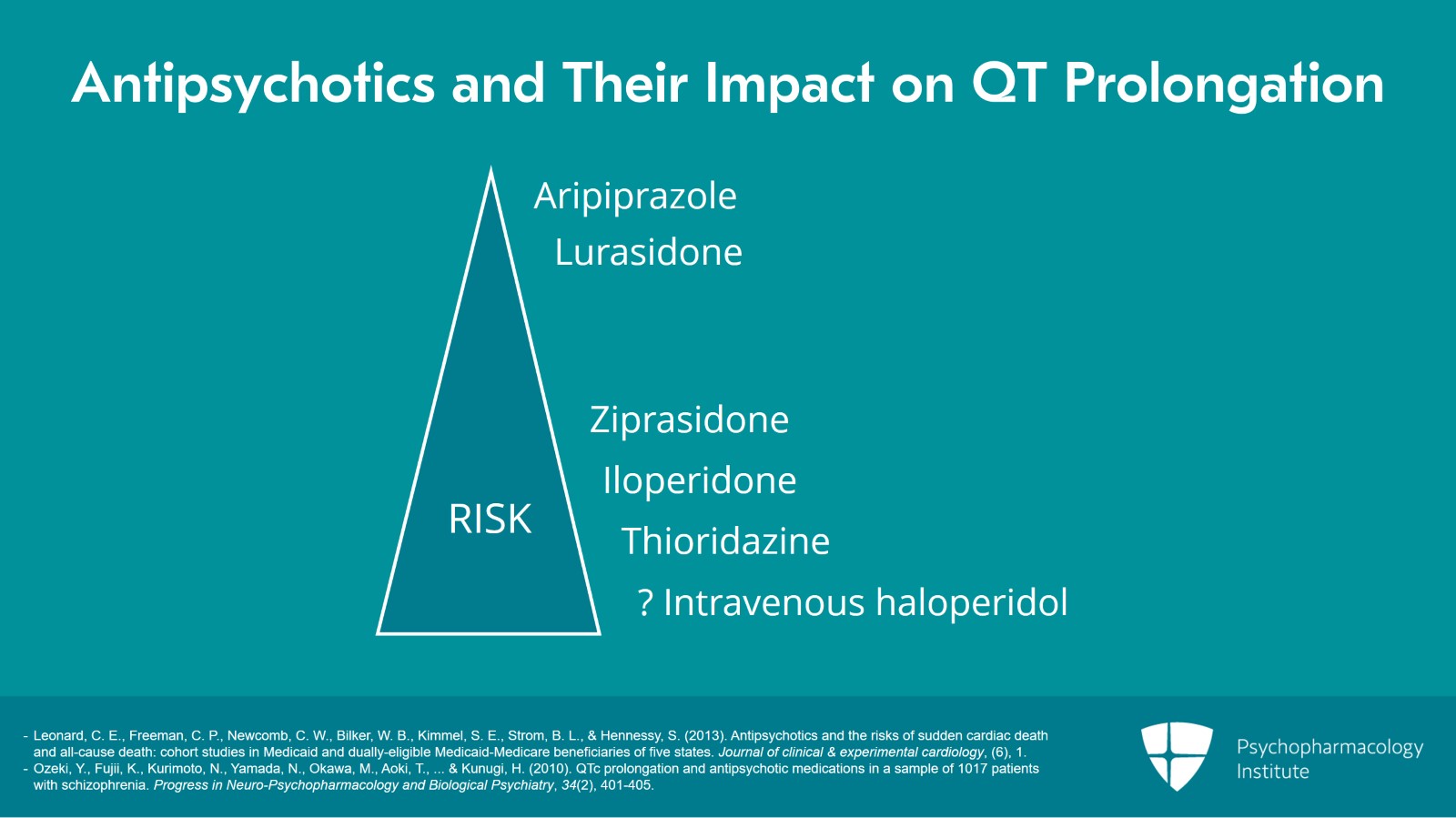
So when we’re thinking about antipsychotics as a whole and their impact on QT prolongation, we can do a little bit of risk stratifying with regard to specific agents though it’s pretty challenging. We think that agents that convey a minimal risk include aripiprazole and lurasidone and we think that agents that convey a higher risk include ziprasidone, iloperidone, thioridazine and possibly intravenous haloperidol.
References:
- Leonard, C. E., Freeman, C. P., Newcomb, C. W., Bilker, W. B., Kimmel, S. E., Strom, B. L., & Hennessy, S. (2013). Antipsychotics and the risks of sudden cardiac death and all-cause death: cohort studies in Medicaid and dually-eligible Medicaid-Medicare beneficiaries of five states. Journal of clinical & experimental cardiology, (6), 1.
- Ozeki, Y., Fujii, K., Kurimoto, N., Yamada, N., Okawa, M., Aoki, T., … & Kunugi, H. (2010). QTc prolongation and antipsychotic medications in a sample of 1017 patients with schizophrenia. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 34(2), 401-405.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 14
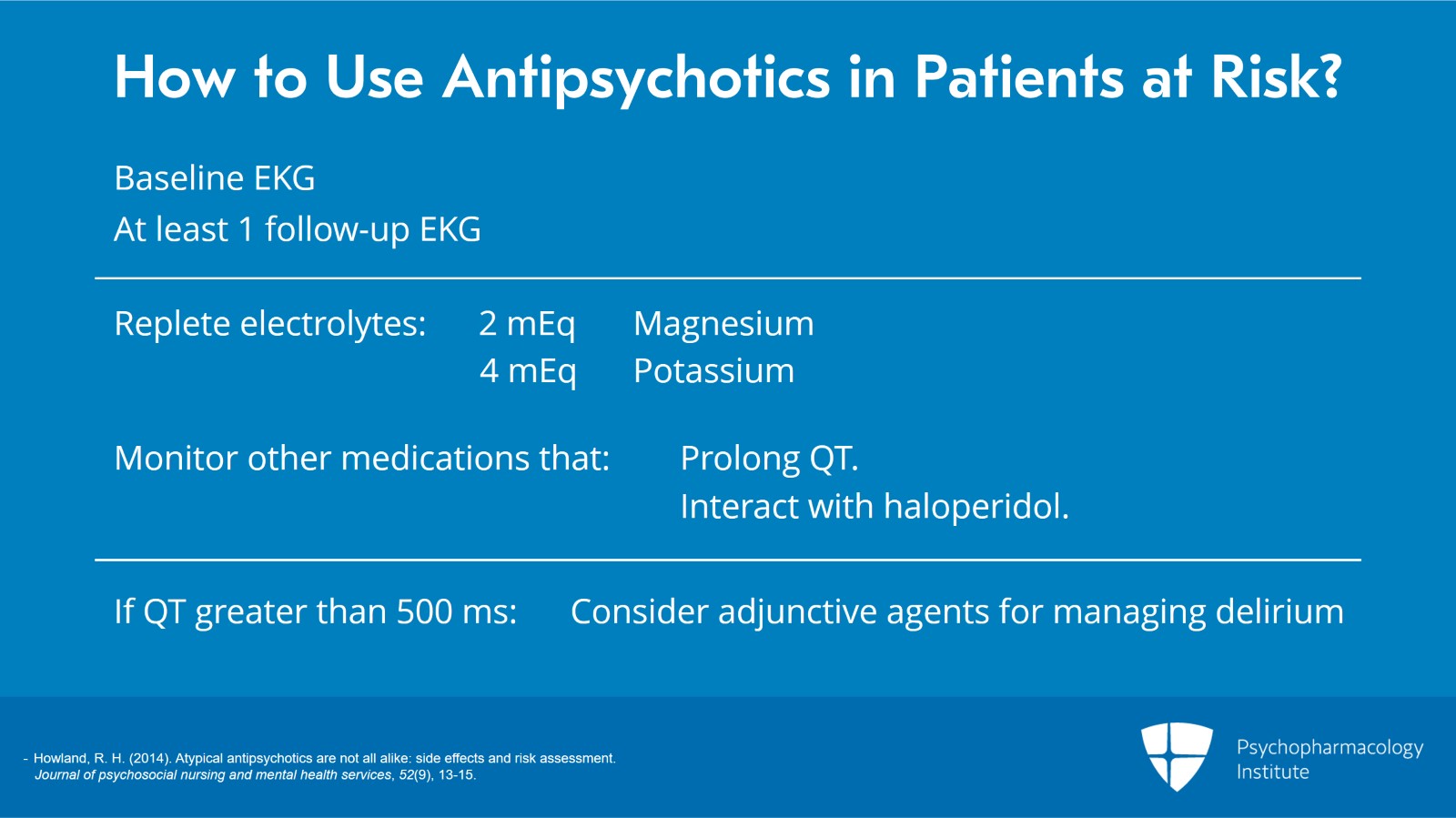
Practically speaking, how do we think about using antipsychotics in patients who may be at risk? Well, for intravenous haloperidol in particular in the inpatient setting, it’s generally recommended that prescribers check a baseline EKG and at least one followup EKG. It is important though to minimize other risk factors for QT prolongation in that setting and that includes repleting electrolytes, specifically magnesium and potassium should be repleted to 2 and 4, respectively, on a daily basis, and minimizing other risk factors which may include looking at other medications that the patient is taking which might either independently increase the risk for QT prolongation or interact with haloperidol in such a way to convey a greater risk and seeing whether there’s room to minimize or mitigate those other risk factors. In patients who have a QT greater than 500 ms, you might want to consider adjunctive agents for managing the delirium in the hospital.
References:
- Howland, R. H. (2014). Atypical antipsychotics are not all alike: side effects and risk assessment. Journal of psychosocial nursing and mental health services, 52(9), 13-15.
Slide 12 of 14
When we think about using antipsychotics in the outpatient setting, we generally don’t recommend monitoring for patients without risk factors unless they’re being prescribed one of the high risk agents such as thioridazine, ziprasidone or iloperidone. There’s really not evidence to monitor patients who are being started on a different antipsychotic who don’t have significant risk factors. On the other hand, for patients who may have multiple risk factors for QT prolongation, it might be worthwhile to obtain an EKG at baseline and intermittently after the initiation of an antipsychotic just to mitigate against the risk.
References:
- Howland, R. H. (2014). Atypical antipsychotics are not all alike: side effects and risk assessment. Journal of psychosocial nursing and mental health services, 52(9), 13-15.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 14
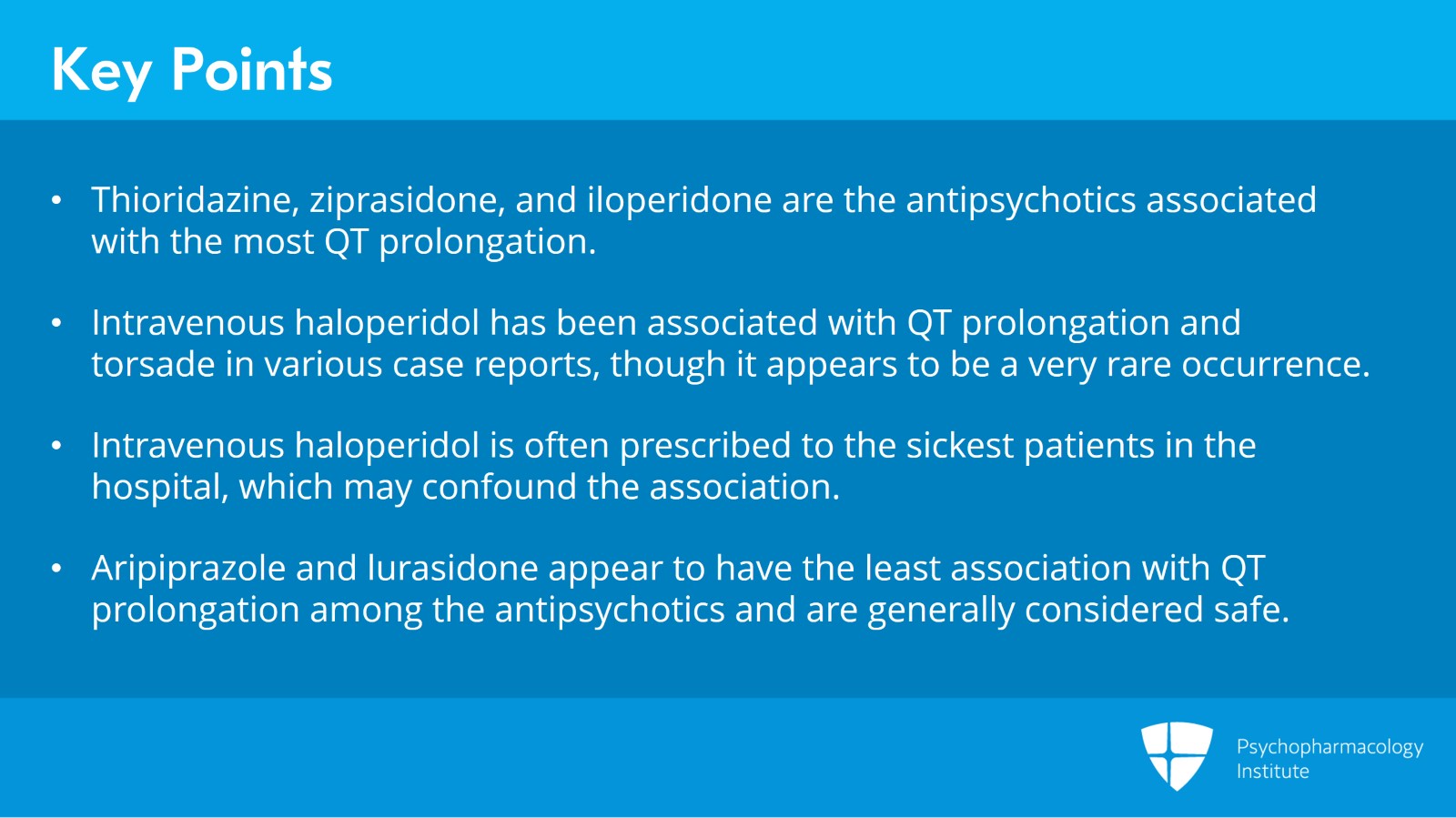
So to summarize some key points from this section, thioridazine, ziprasidone and iloperidone are the antipsychotics associated with the most QT prolongation. Intravenous haloperidol has been associated with QT prolongation and torsade in various case reports though it appears to be a very rare occurrence and it’s important to remember that intravenous haloperidol is often prescribed to the sickest patients in the hospital which may confound the association. Aripiprazole and lurasidone appear to have the least association with QT prolongation among the antipsychotics and are generally considered safe in this regard.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.