.
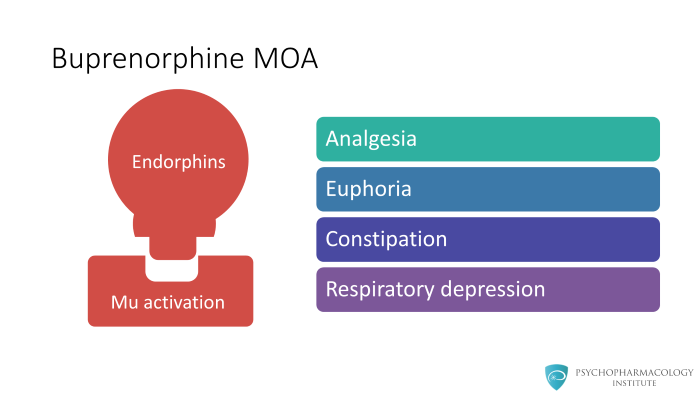
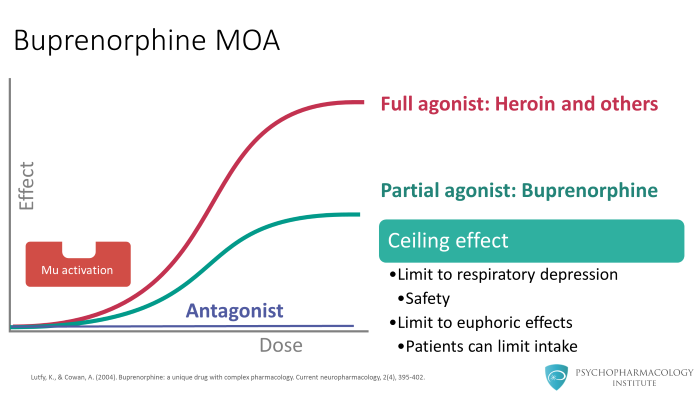
Let me start with the buprenorphine mechanism of action and rationale for therapeutic use. In the brain, naturally produced opioids called endorphins are released in the synapse and activate the opioid receptors producing a classic mu-opioid response. The effects include: analgesia, euphoria, constipation and respiratory depression.
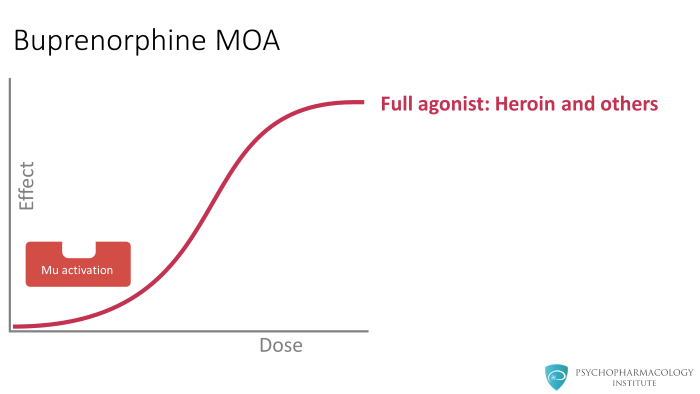
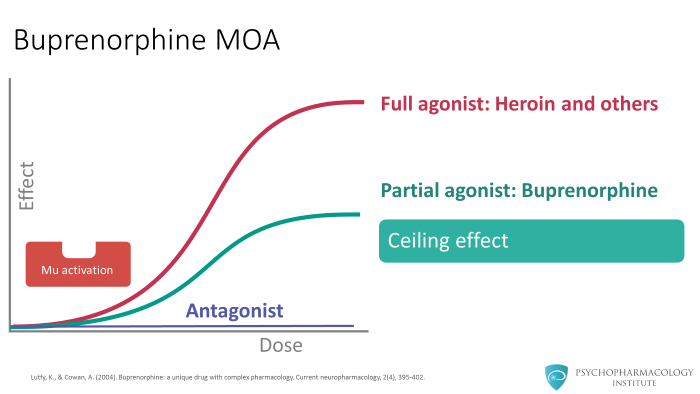
Antagonists attach to receptors but never actually activate the receptors. Therefore, antagonists unlike either partial or full agonist never activate the receptors.
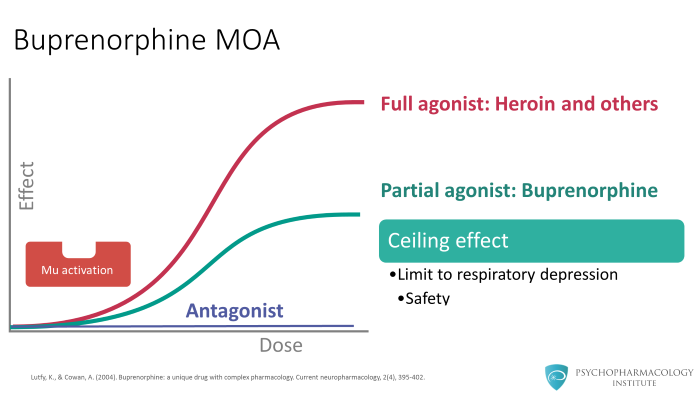
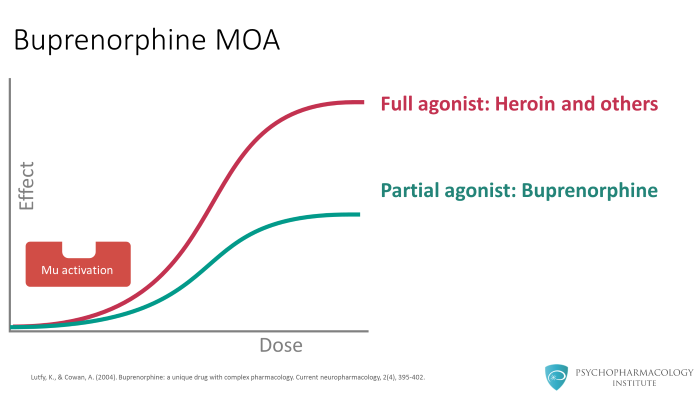
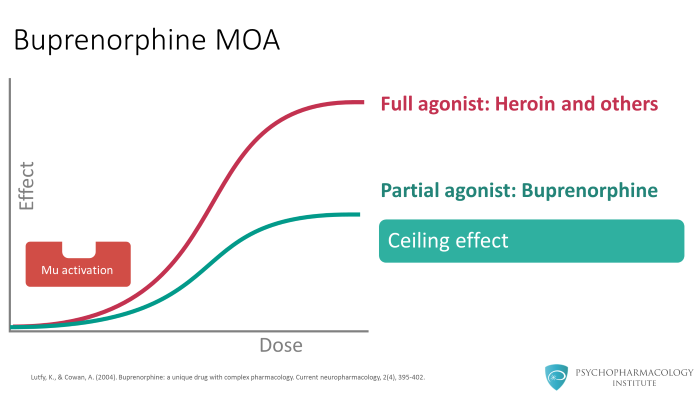
The ceiling effect of buprenorphine means that there is a limit on the respiratory depression. This is one of the reasons why this medication can be safely prescribed.
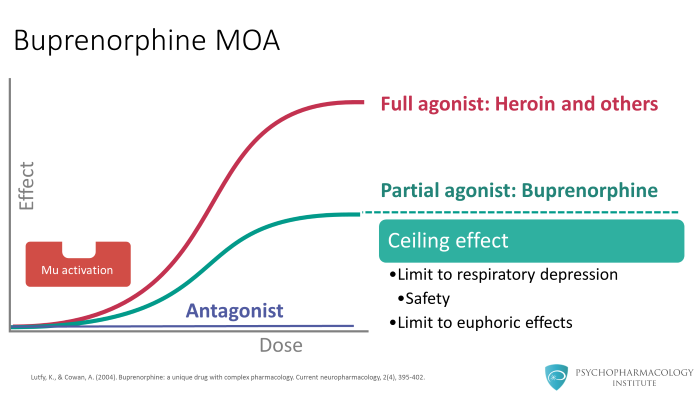
What this also means is that taking more buprenorphine does not lead to additional euphoric effects. This is very different from other full agonist opioids (oxycodone, heroin or morphine) where taking additional doses generally means you get additional euphoria. This is exactly why patients can be trusted to take one or two tablets a day and refrain from taking additional tablets.
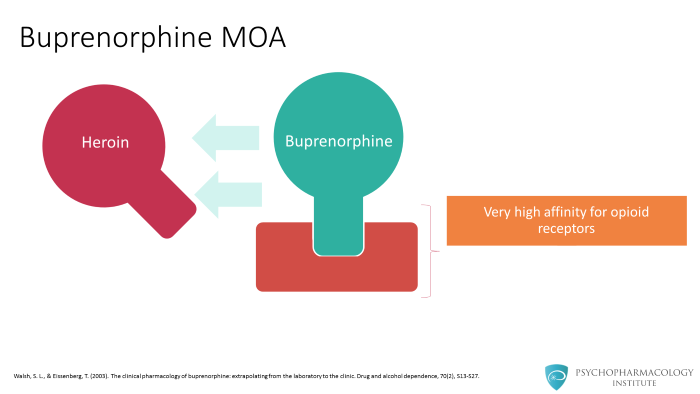
The second issue about buprenorphine is that it has a very high affinity for the opioid receptor, which means that it binds very tightly to the receptors. If buprenorphine is attached to the receptor, other full agonists typically used such as heroin, oxycodone, morphine will not displace buprenorphine.
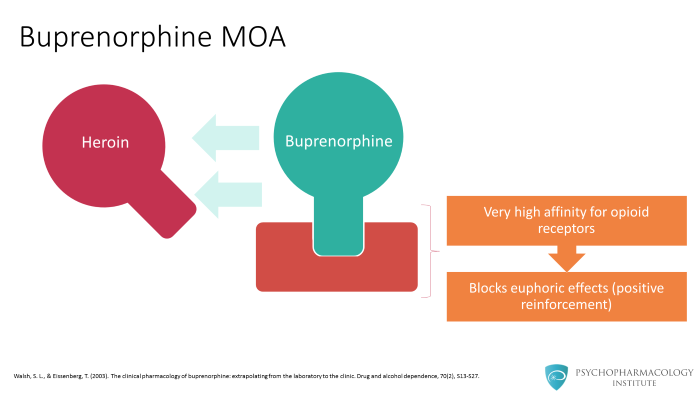
This is a critical benefit to patients because while the patient is taking buprenorphine, even if they use heroin, they will not experience any euphoria.
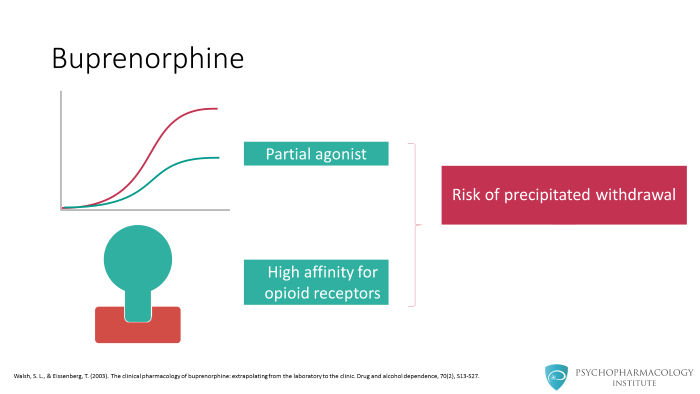
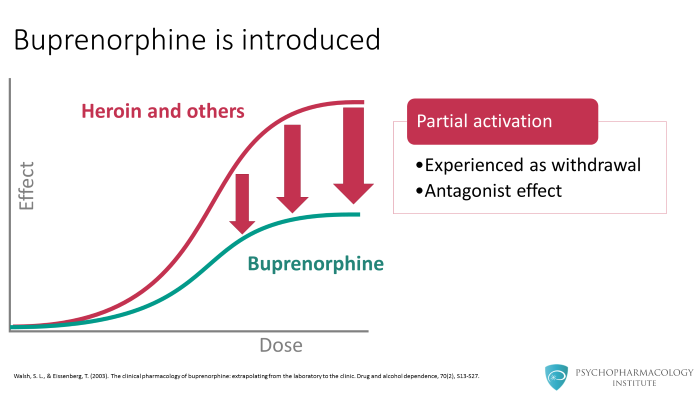
When you combine these two concepts of buprenorphine that A, it is a partial agonist and B, it has a high affinity at the opioid receptors, there is now a possibility for precipitated withdrawal.
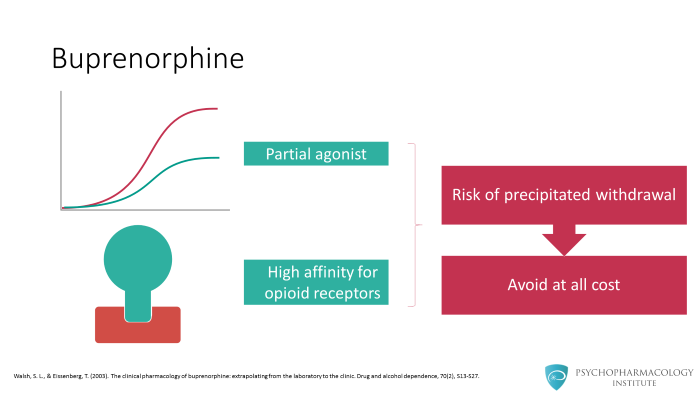
During buprenorphine treatment, this is the one most concerning adverse event that has to be avoided at all cost.
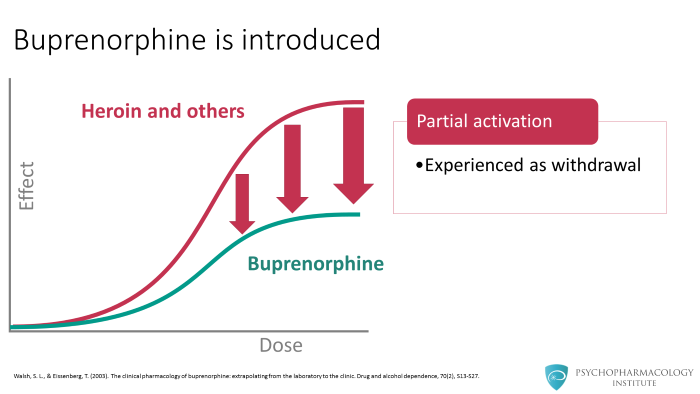
On the other hand, if heroin is already on the receptor and then buprenorphine is introduced, because buprenorphine has a high affinity for the receptor, buprenorphine will displace the heroin. Once this happens, this displacement will cause a sudden drop in the receptor activation going from a full activation to partial activation. This sudden drop in activation is experienced as withdrawal.
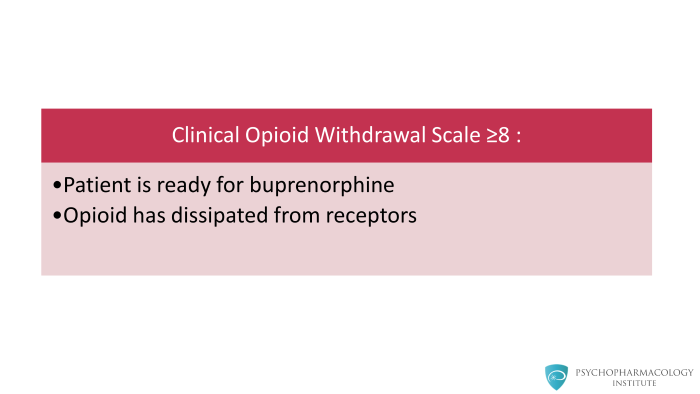
The way we gauge this is by using a scale called the Clinical Opioid Withdrawal Scale or COW Scale. If the COWS score is 8 or greater, generally we think that the patient is sufficiently ready for the introduction of buprenorphine, meaning sufficient amounts of heroin or other opioids have dissipated from the receptors such that introduction of buprenorphine will not cause antagonist effects or withdrawal effects. Instead what happens is an increase in receptor activation which is experienced as agonist effects.
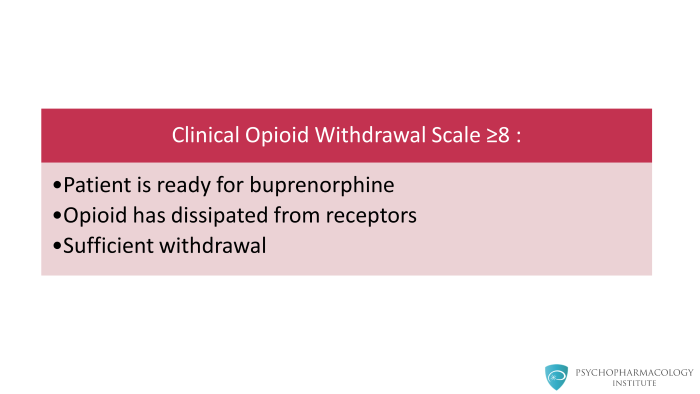
Therefore, it is critical for patients starting on buprenorphine to first be in sufficient amount of withdrawal (from heroin, morphine or oxycodone) before buprenorphine is introduced. If the patient is not, then introduction of buprenorphine will cause even worse withdrawal.
References
- Lutfy, K., & Cowan, A. (2004). Buprenorphine: a unique drug with complex pharmacology . Current neuropharmacology, 2(4), 395-402.
- Walsh, S. L., & Eissenberg, T. (2003). The clinical pharmacology of buprenorphine: extrapolating from the laboratory to the clinic . Drug and alcohol dependence, 70(2), S13-S27.



