Slides and Transcript
Slide 2 of 30
It is a mu-opioid partial agonist and to a lesser extent a kappa-opioid antagonist. Buprenorphine binds very tightly to the mu-opioid receptor so any opioid will be displaced. Also, the original formulations have been sublingual due to poor oral bioavailability.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 30
To expand more, buprenorphine can satisfy opioid receptors so that withdrawal and cravings are reduced and illicit opioids are no longer pleasurable. Generally, buprenorphine is combined with naloxone to reduce misuse, for example, injecting the medication. Today, we will be primarily the combined buprenorphine/naloxone sublingual to keep the discussion simple.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Slide 4 of 30
However, note for some populations like pregnant people, it is not appropriate to prescribe buprenorphine with naloxone. It must just be buprenorphine.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 30
There are many steps that are involved in office-based treatment with buprenorphine. Note that many of these are common to methadone but outside of OTPs most of us will not be managing methadone. We will generally be prescribing buprenorphine so I will go over the assessment with respect to that but many of the steps can be used for methadone as well.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Slide 6 of 30
First, we need to ensure that there is a need for treatment and that somebody has an opioid use disorder. Next, just as we would do with any medication, we complete a history, lab workup.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 30
And provide a comprehensive treatment plan including counseling. Then we provide education about the medication, withdrawal, how to keep the medication safely.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Slide 8 of 30
It's also important to check the PMP or prescription drug monitoring programs and complete a full substance history to inquire about other substance use. Mostly, we want to ensure that there are no other substances that may interfere with the medication but it's notable that the risk of respiratory depression is also much lower with buprenorphine. A urine drug screen can also help identify other drugs but also ensure that somebody is using the opioids and that they need the treatment to begin with.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 30
It is important to provide naloxone and education around naloxone. We would also want to provide education on overdose risks associated with using other substances.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Slide 10 of 30
And also provide education on restarting illicit use after being on treatment. Tolerance reduces and so the same dose of a drug that somebody was using prior to treatment may be too much and that's why increase, there's increased risk of overdose.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 30
Of course, we always want to treat co-occurring disorders such as depression, anxiety and other substance use disorders. Finally, we want to create a customized and patient-centered treatment plan for the medications and more. If someone does need a higher level of care, it is important to refer.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Slide 12 of 30
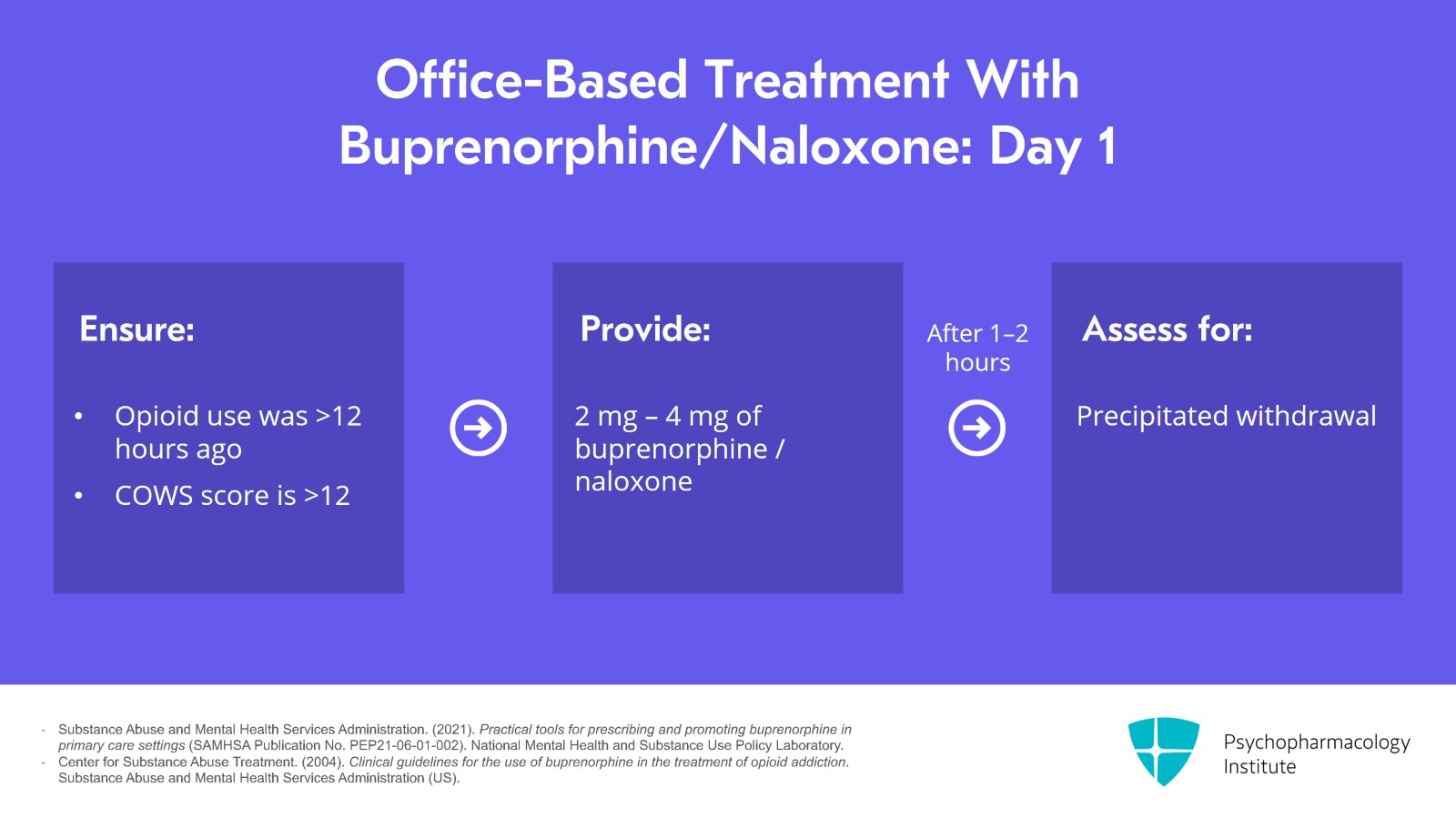
On day 1, we ensure that opioid use was more than 12 hours ago, 36 to 72 hours if they've been on long-acting opioids. A COWS score should be over 12. We provide 2 to 4 mg of the medication and after an hour or two assess for precipitated withdrawal.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 30
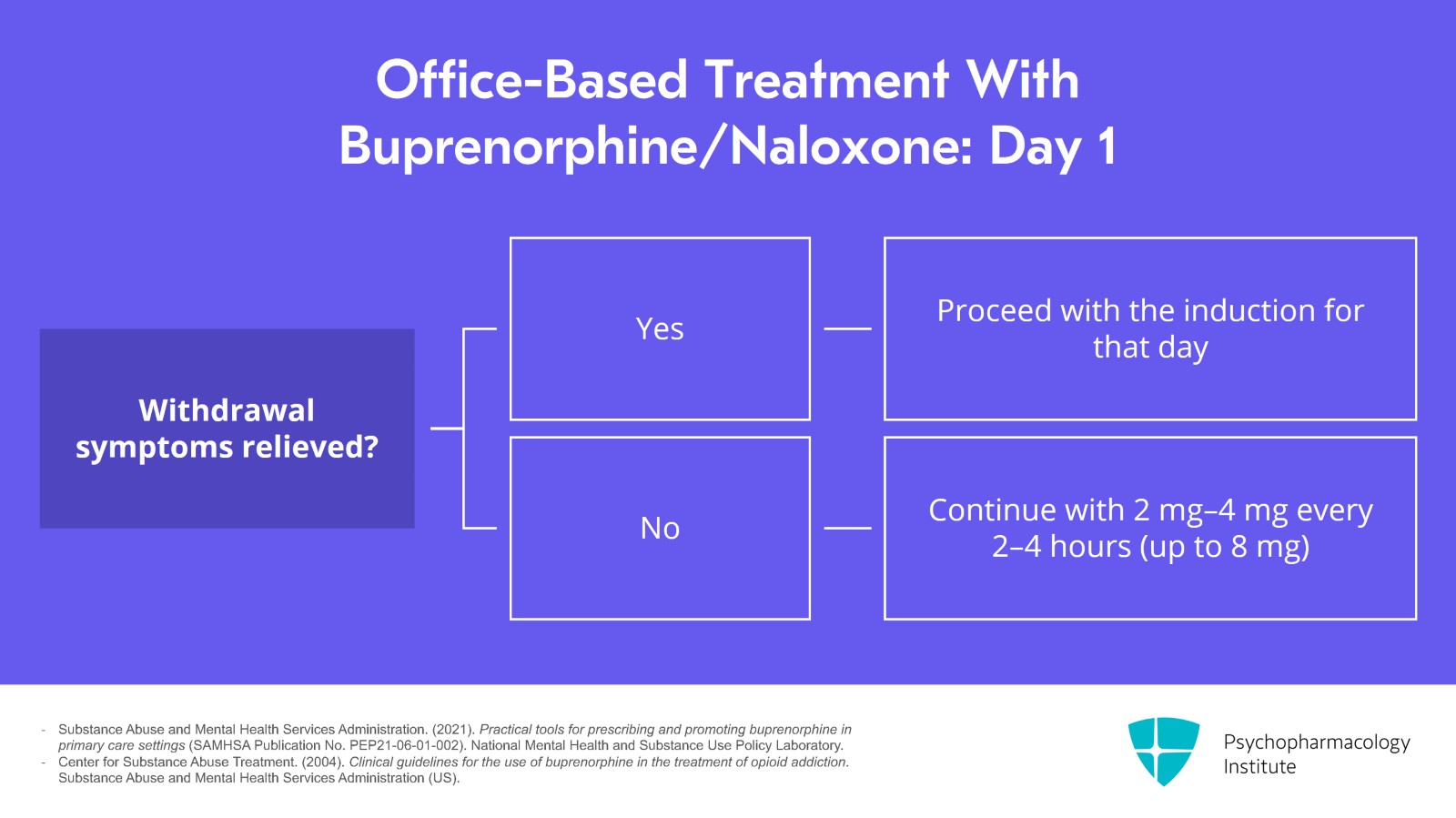
If in precipitated withdrawal, we should proceed with the induction for that day. Otherwise, we can continue with two more doses of 2 to 4 mg every two to four hours. The goal is to get to around 8 mg and resolve withdrawal.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Slide 14 of 30
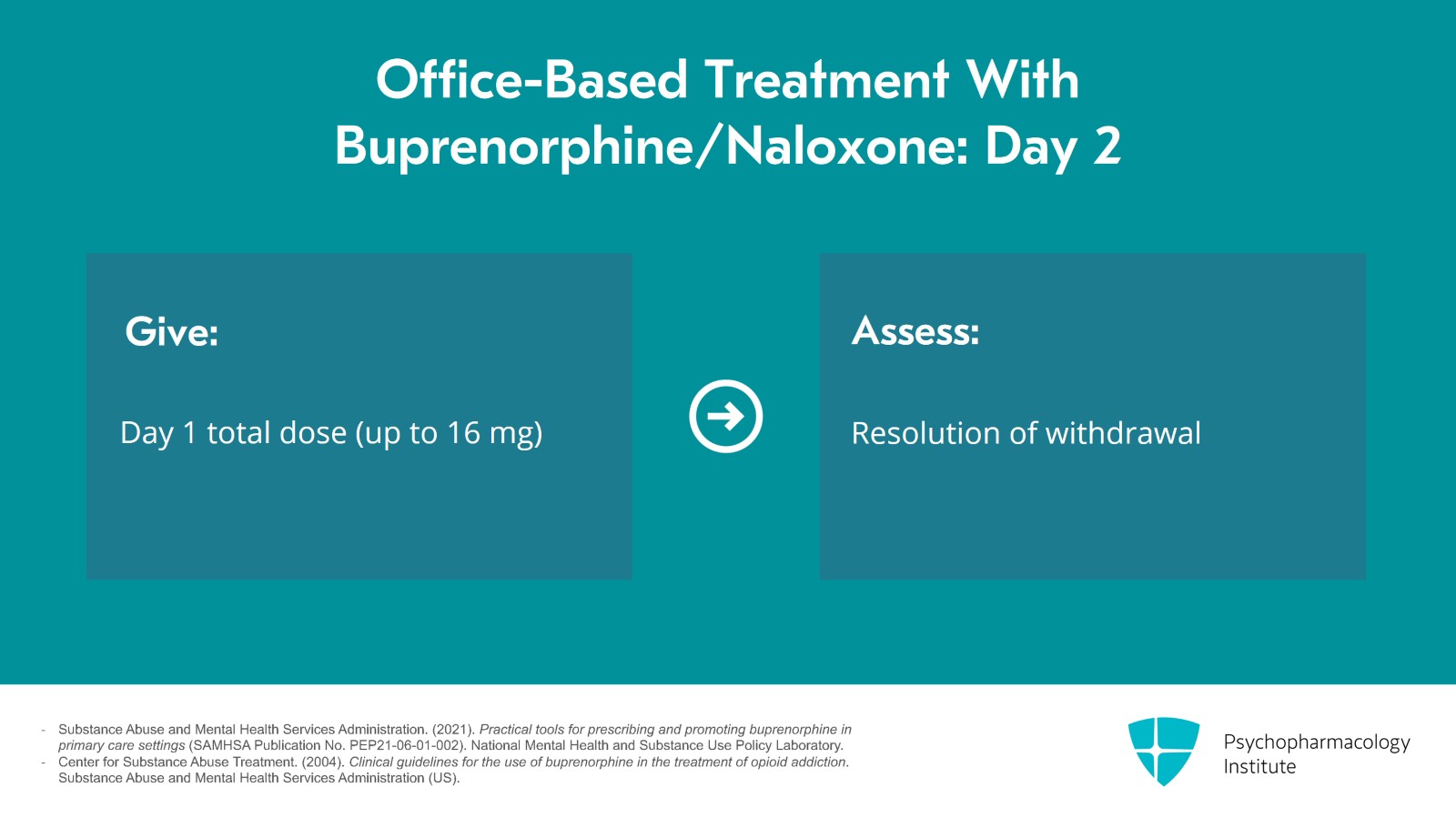
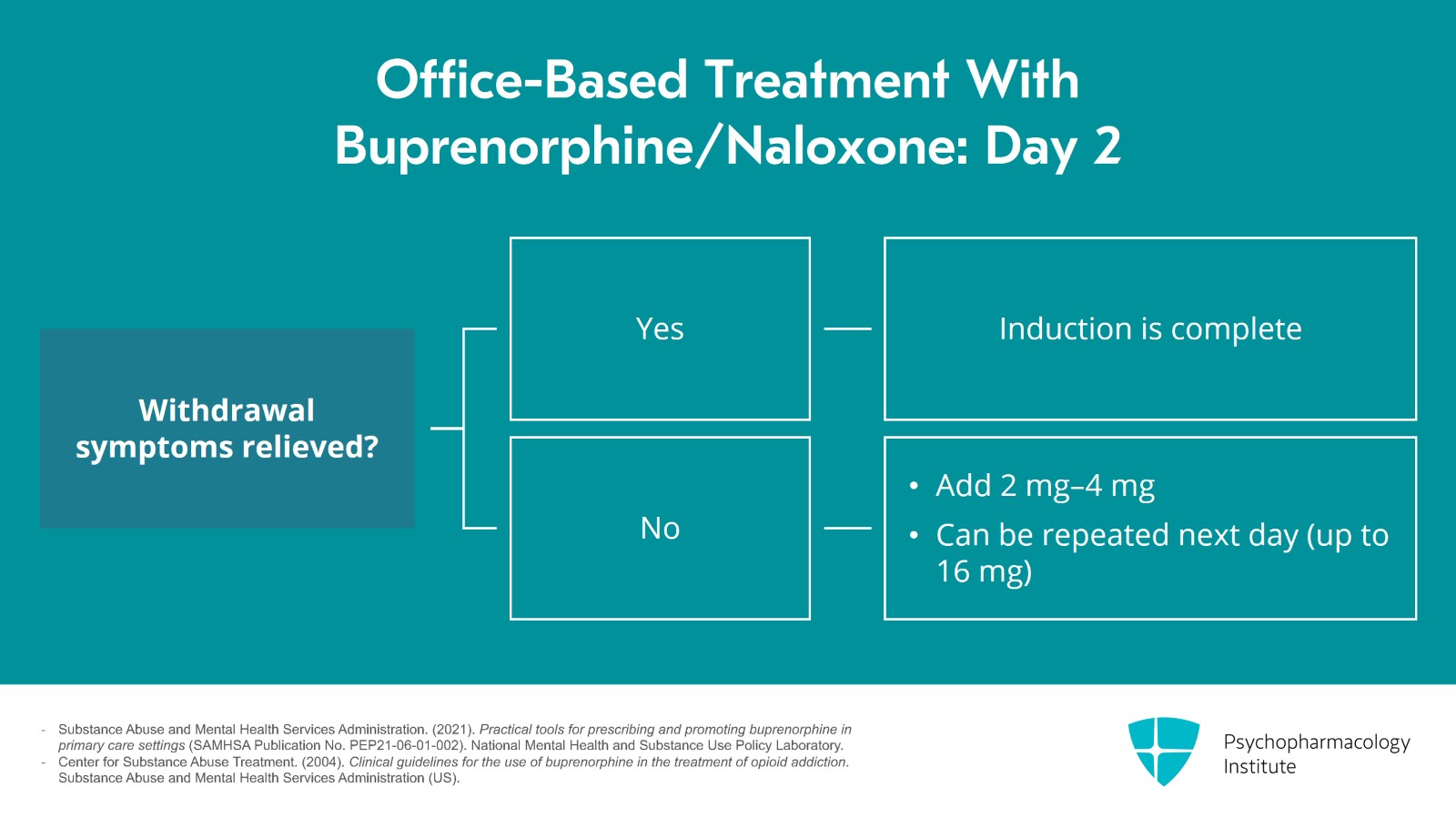
On day 2, we give the day 1 total dose which can be up to 16 mg and then see if withdrawal is completely resolved.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 30
If so, induction is complete. If not, we can add 2 to 4 mg more. We can repeat this for another day and add to 2 to 4 mg, again up to 16 mg usually.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Slide 16 of 30
Another thing to consider is at-home inductions that are possible and safe. Patients can be instructed about precipitated withdrawal and withdrawal symptoms. By allowing them to undergo the induction process in the comfort of their home, the likelihood of them actually starting treatment may increase.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 30
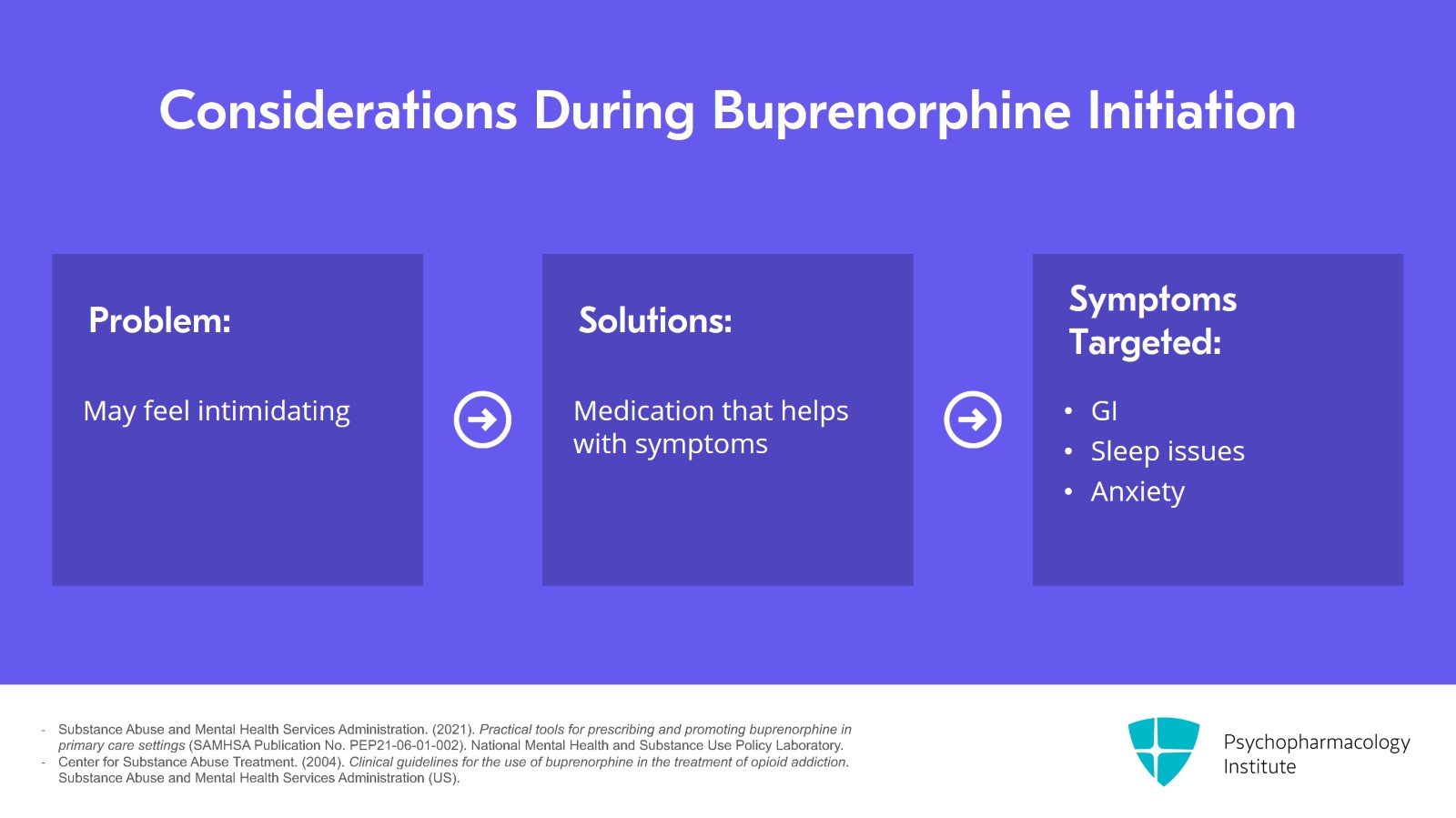
Getting people to start on buprenorphine may feel intimidating since they need to be in withdrawal. There are a number of options to help symptoms. Over-the-counter and some prescription medications can help with GI symptoms, sleep issues and anxiety.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Slide 18 of 30
If clonidine is used, very low doses are indicated and it is important to warn them about the side effects of clonidine such as low blood pressure. It is also important for people to undergo withdrawal on a day that works well for them and to hydrate. For example, undergoing withdrawal during a busy work shift is not ideal.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 30
Over time, people are usually maintained on 4 to 24 mg with most doing well at 16 mg. The maximum recommended dose is 32 mg.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Slide 20 of 30
If somebody is still using other opioids or running out of medications early, for example, if they're on 12 mg, it is usually an indication that they need a more sufficient dose.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 21 of 30
It is good to encourage treatment and recovery such as groups, counseling and treatment of other psychiatric diagnoses.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Slide 22 of 30
Moving along, the goal of treatment is to eliminate withdrawal, to reduce cravings and to eliminate other opioid use. I feel most satisfied in working with patients on this medication when they tell me they feel normal again and they're able to engage in their regular activities without opioids being something that they're worried about.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 23 of 30
It's useful to continue the medication for as long as needed since treatment usually leads to better outcomes.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
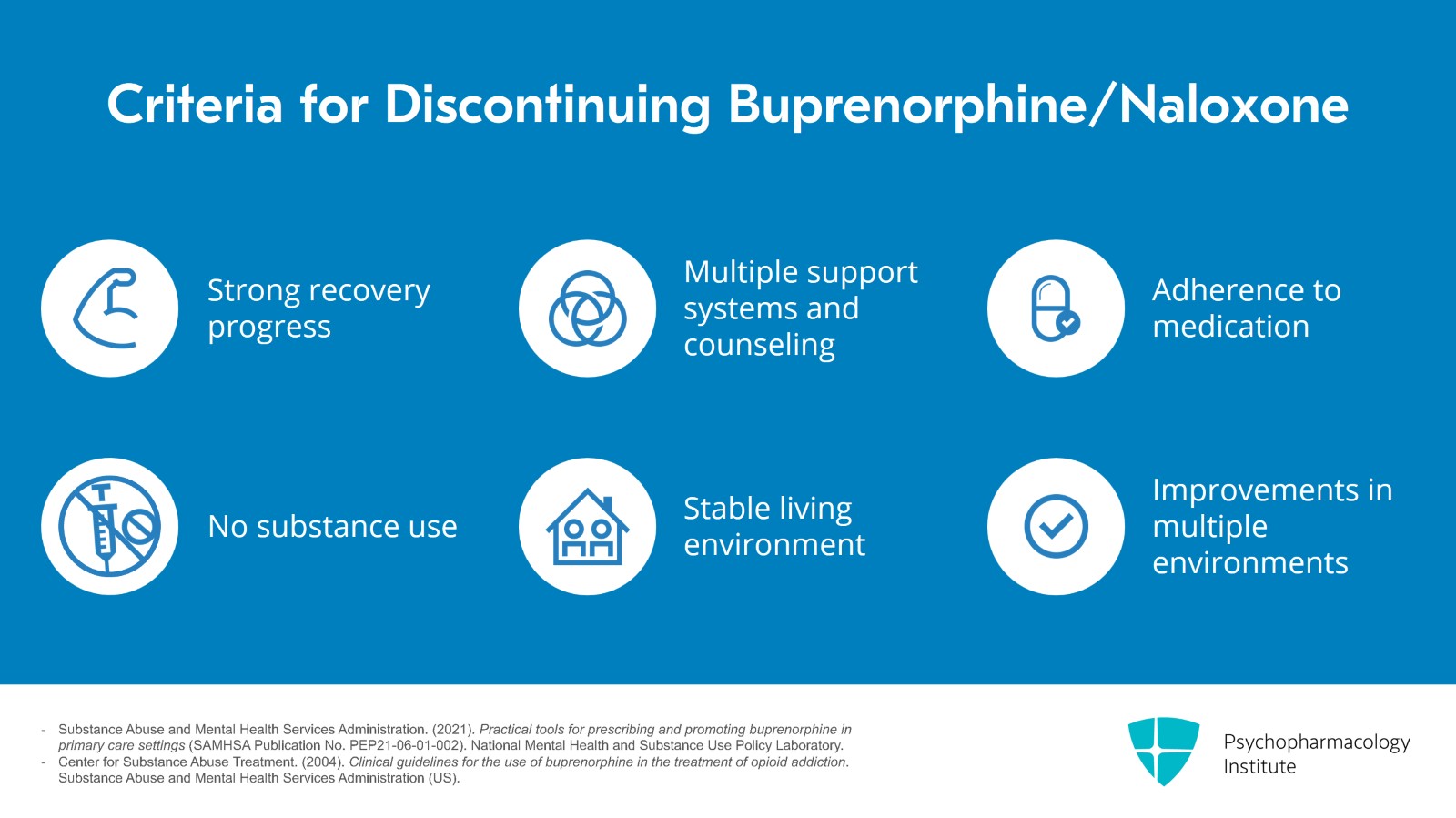
Slide 24 of 30
When considering discontinuing the medication, somebody should be at a very strong point in their recovery, have multiple supports and be in counseling. They should be adherent to the medication, not using other substances, have a stable environment and have good improvements in home, work and school.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 25 of 30
You can develop a tapering plan and it is useful to stay in close contact with the patient during this phase. It's also very important to counsel them about the risks of return to use and the increased risk of overdose. Again, I'll emphasize that continuing on this medication for years is advisable until there is very strong stability.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Slide 26 of 30
I've talked a lot about the advantages of buprenorphine but I will list a few disadvantages. For some of our patients, having more structure is helpful. Therefore, less monitoring isn't always desirable. Another major issue is that somebody needs to be in opioid withdrawal to start which can be really hard for many of our patients. Buprenorphine is also a blocker of opioid pain medications. So if somebody needs to be on them down the line, they must get off of buprenorphine. Finally, when it comes to pain, a lot of people find some relief from buprenorphine but not complete. For those, methadone may be preferred.
References:
- Substance Abuse and Mental Health Services Administration. (2021). Practical tools for prescribing and promoting buprenorphine in primary care settings (SAMHSA Publication No. PEP21-06-01-002). National Mental Health and Substance Use Policy Laboratory.
- Center for Substance Abuse Treatment. (2004). Clinical guidelines for the use of buprenorphine in the treatment of opioid addiction. Substance Abuse and Mental Health Services Administration (US).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 27 of 30
To summarize key points, buprenorphine is an extremely effective medication for opioid use disorder. As an opioid receptor partial agonist, it satisfies the receptors without contributing to euphoria as well as the risk of respiratory depression compared to methadone.
Slide 28 of 30
In order to start the medication, we should do a thorough history and physical assessment, treat all conditions, do urine drug testing and ensure that somebody is in withdrawal. They must be in withdrawal so that we do not very aggressively precipitate withdrawal.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 29 of 30
The medication induction process is usually done over one to three days and can be done at home. Visit frequencies can space out from daily to weeks to months and patients should remain on the medication for better outcomes.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.