Slides and Transcript
Slide 1 of 11
Video 5. Body Dysmorphic Disorder: Medications, CBT and Exposure Response Prevention Therapy.
Slide 2 of 11
So again, as with all the OCRD, there is an integrated approach to BDD treatment.
Moderate to severe cases usually require both medications and ERP.
With mild cases, using ERP alone can be appropriate.
Just briefly, the exposure and response prevention therapy that is used for BDD is similar to ERP that is used in OCD. It’s different in some ways.
Essentially, what you are doing is getting the person to look at themselves and exposing them to their body in order to get neutral feelings with their body rather than the anxiety feelings that they usually get.
References:
- Fang, A., Matheny, N. L., & Wilhelm, S. (2014). Body dysmorphic disorder. The Psychiatric Clinics of North America, 37(3), 287–300.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 11
Let me talk about some of the medication treatments for BDD.
There was a double-blind crossover of 29 patients, clomipramine versus desipramine. And the clomipramine patients were noted to have improvement. Functional disability improved. And interestingly, patients who would be considered to be delusional or lacking insight completely, they responded the best.
And what DSM-5 considers delusional level of insight, that’s not actually delusional, that’s not actually psychotic. It’s just called delusional insight and it’s confusing terminology, I know. DSM-5 decided not to change that. I just really wanted or I would prefer the term absent insight but these people aren’t actually psychotic. They may look psychotic because of their lack of insight. But interestingly, they improved on clomipramine the most.
There was another trial of fluoxetine versus placebo. And they noted that the active medication improved symptoms and it worked as equally well in people with delusional insight as it did other people with body dysmorphic disorder. It also was noted that fluoxetine had a protective effect on suicidality.
References:
- Phillips, K. A., Albertini, R. S., & Rasmussen, S. A. (2002). A randomized placebo-controlled trial of fluoxetine in body dysmorphic disorder. Archives of General Psychiatry, 59(4), 381.
- Hollander, E., Allen, A., Kwon, J., Aronowitz, B., Schmeidler, J., Wong, C., & Simeon, D. (1999). Clomipramine vs Desipramine crossover trial in body dysmorphic disorder. Archives of General Psychiatry, 56(11), 1033.
Slide 4 of 11
Now, there is no differences in responses to the different SSRIs. So one SSRI seems to be the same as the other. And I think this is going to be the same for most of the obsessive-compulsive and related disorders.
There was data presented earlier that showed that escitalopram and citalopram may not be as effective in hoarding disorder. As I said that may be an artifact of the diagnosis at that time.
We know that for most of the obsessive-compulsive and related disorders there doesn’t seem to be a difference in response to the different SSRIs. I recommend people choose medications based on clinical preference and patient side effects.
References:
- Fang, A., Matheny, N. L., & Wilhelm, S. (2014). Body dysmorphic disorder. The Psychiatric Clinics of North America, 37(3), 287–300.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 11
So augmentation in body dysmorphic disorder.
There have been a number of studies that have looked at augmentation using a high-potency antipsychotic, pimozide. Pimozide was proved to be no more effective than placebo augmentation of fluoxetine even in patients with delusional insight.
However, buspirone augmentation may work at 60 mg a day.
There was one study that showed that 17 patients had some response to levetiracetam but I will tell you that study has significant flaws. That is not a medication that I generally recommend, certainly not based on that study.
References:
- Phillips, K. A. (2005). Placebo-controlled study of Pimozide augmentation of fluoxetine in body dysmorphic disorder. American Journal of Psychiatry, 162(2), 377-379.
- Phillips K. A. (1996). An open study of buspirone augmentation of serotonin-reuptake inhibitors in body dysmorphic disorder. Psychopharmacology Bulletin, 32(1), 175–180.
- Phillips, K. A., & Menard, W. (2009). A prospective pilot study of levetiracetam for body dysmorphic disorder. CNS Spectrums, 14(5), 252–260.
Slide 6 of 11
I think some take-home points with this are that the SSRIs work best when they stand alone. And I recommend SSRIs for body dysmorphic disorder even in patients who are delusional.
And in fact, the patients who are delusional may have the most powerful effects to SSRIs.
If you need augmentation, I would not think of antipsychotics, again even in the delusional patients.
Buspirone is the medication that seems to have the best evidence if used at the 60 mg a day dose.
Clomipramine may be one that can be used as a third line and maybe a little more effective than some of the SSRIs based on some work that is done as shown above.
References:
- Fang, A., Matheny, N. L., & Wilhelm, S. (2014). Body dysmorphic disorder. The Psychiatric Clinics of North America, 37(3), 287–300.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 11
For cognitive behavioral therapy, again psychotherapy is the treatment of choice. It’s done either individually or group. Certainly, depression can improve. And it’s typically weekly for five to six months. And homework is given with appropriate CBT and they are given a daily homework.
References:
- Fang, A., Matheny, N. L., & Wilhelm, S. (2014). Body dysmorphic disorder. The Psychiatric Clinics of North America, 37(3), 287–300.
Slide 8 of 11
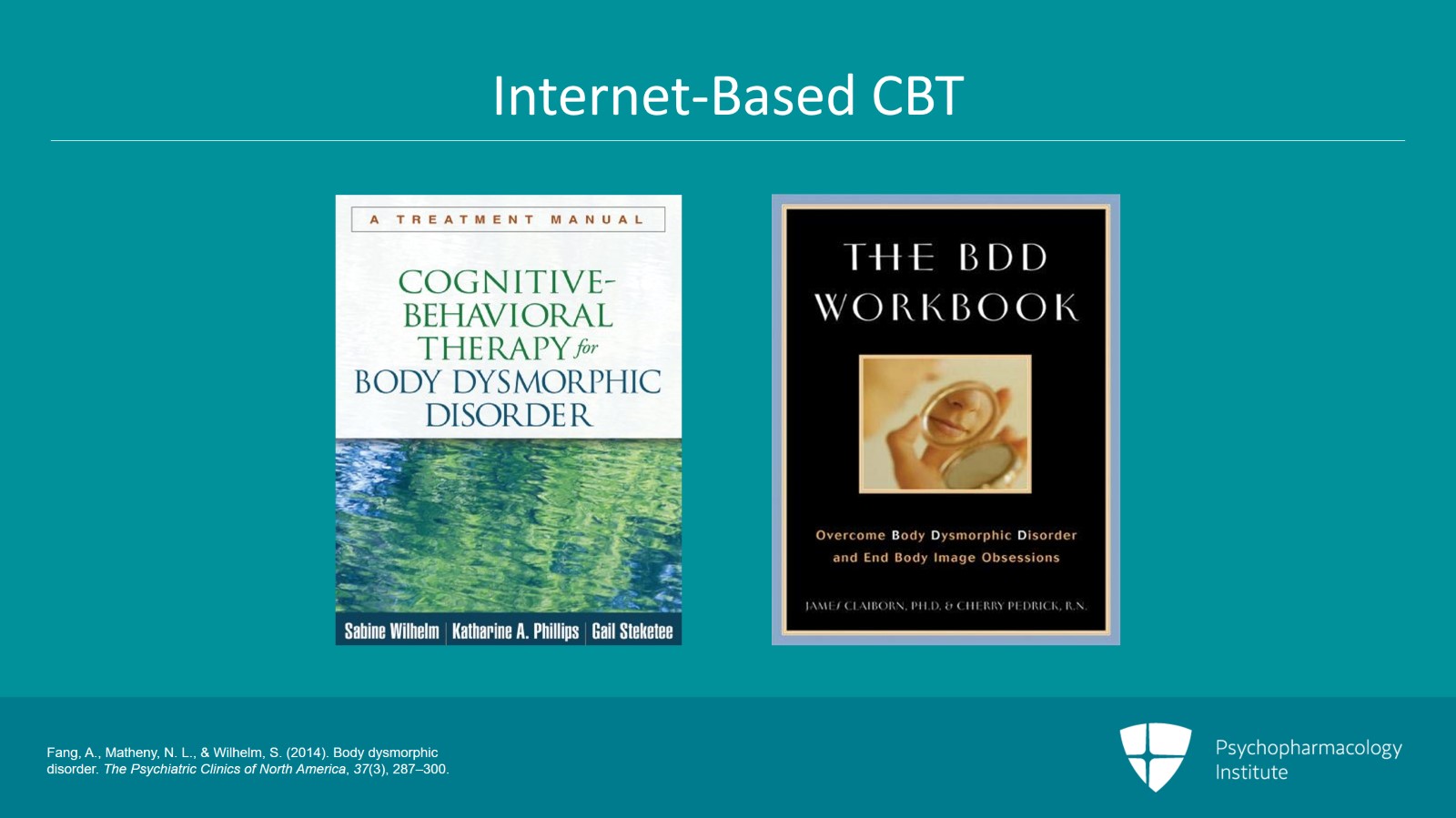
For people who want some CBT, there isn’t any good internet-based CBT but there are manuals for therapists. I recommend the Cognitive Behavioral Therapy for Body Dysmorphic Disorder by Wilhelm, Phillips and Steketee.
And as a self-help manual for patients, I recommend the BDD Workbook: Overcoming Body Dysmorphic Disorder and End Body Image Obsessions by Claiborn and Pedrick. And that’s a self-help workbook.
References:
- Fang, A., Matheny, N. L., & Wilhelm, S. (2014). Body dysmorphic disorder. The Psychiatric Clinics of North America, 37(3), 287–300.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 11
Key points for this lecture. SSRIs are the first-line medication treatment choice for BDD and like all the OCRD, OCD doses should be used. Refer back to the other lecture for OCD dosing of medications.
Antipsychotics have not been shown to be helpful with body dysmorphic disorder even in patients with so-called delusional insight. The SSRIs or clomipramine seems to be the most powerful medications in this delusional cohort.
Slide 10 of 11
Clomipramine can be used if a patient fails an SSRI. Buspirone has some evidence as an SSRI augmentation therapy in these patients and is my recommended augmentation strategy for BDD.
Thank you.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.