Slides and Transcript
Slide 1 of 17
So video 4. Body Dysmorphic Disorder: The DSM-5 Criteria and Clinical Features. BDD, one of the more severe psychiatric disorders and especially as far as its morbidity and mortality.
Slide 2 of 17
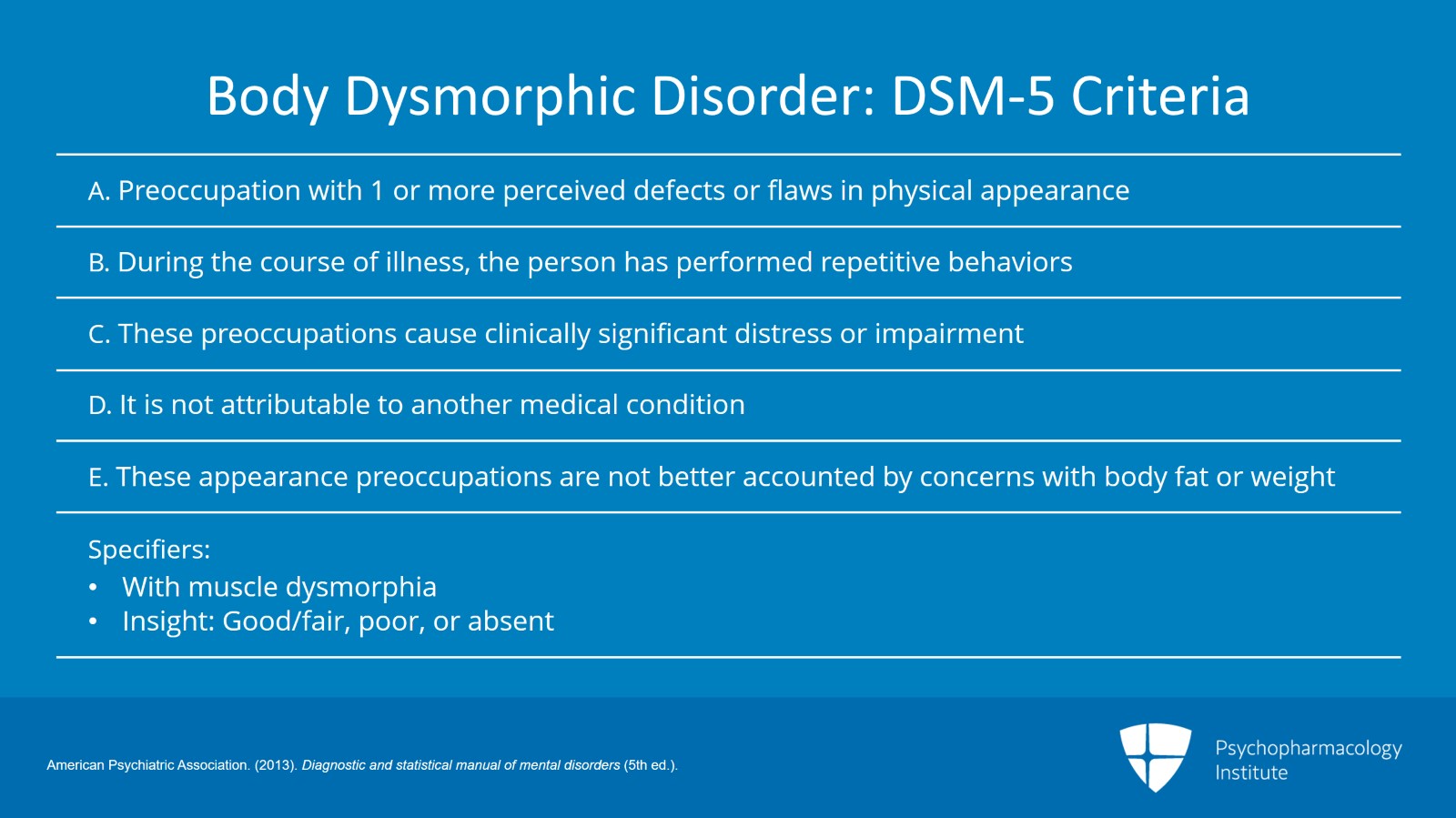
So the DSM-5 criteria, preoccupation with one or more perceived defects or flaws in physical appearance that are either not observable or really appears slight to other people. At some point during the course of the disorder, the person has performed repetitive behaviors. So mirror checking, excessive grooming, skin picking, reassurance seeking or performing mental acts such as comparing their appearance with that of others in response to the appearance concerns. These preoccupations cause clinically significant distress or impairment in social, occupational or other important areas of functioning. This is not attributable to another medical condition. And importantly, this appearance preoccupations are not better accounted for by concerns with body fat or weight. If a person is concerned about how much they weigh or how much body fat they have, typically an eating disorder would be a more appropriate diagnosis. There are two specifiers. Muscle dysmorphia is a specifier. This is often seen in men and these are men who have concerns that their muscles are too small and will spend excessive amounts of time exercising trying to build up their muscles and may also abuse steroids, anabolic steroids as a result. Insight is listed as good/fair, poor or absent.
References:
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 17
Clinical features This can occur in all age groups. It does usually begin in early adolescence. While OCD has an even male to female ratio, there's a slight female predominance in this illness at a 3:2 ratio, female to male. Now, the symptoms of BDD are similar in both genders with the exception of muscle dysmorphia which again is typically seen in men.
References:
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
Slide 4 of 17
BDD usually is seen with obsessions and preoccupations with appearance. Typically, it involves the face, head or hairline but it can occur with any body part and most patients with BDD will have obsessions or preoccupations with multiple body parts. The insight for BDD tends to be on the lower end of the scale, usually poor or absent. They have worries about being mocked and they will talk to you about being paranoid, worries that others are looking at them, others are talking about them. Their complaints can almost sound psychotic and they will often use the term paranoia to describe it. Three to eight hours a day of preoccupations that are difficult to resist. They spend a great amount of time during the day on this preoccupation.
References:
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
- Phillips, K.A. (2011). Body Dysmorphic Disorder. In Hudak, R. & Dougherty, D. D. (Eds.) Clinical obsessive-compulsive disorders in adults and children (pp. 122–137). Cambridge University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 17
Melancholia is a common comorbidity. So one of the more severe types of major depressive disorder is a very common comorbidity in people with BDD. And there are markedly poor outcomes in quality of life ratings with this disorder.
References:
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
- Phillips, K.A. (2011). Body Dysmorphic Disorder. In Hudak, R. & Dougherty, D. D. (Eds.) Clinical obsessive-compulsive disorders in adults and children (pp. 122–137). Cambridge University Press.
Slide 6 of 17
Now, most patients with BDD will perform the compulsive behaviors that I talked about above. Usually, this involves checking, hiding or fixing perceived deficits. They may have favorite clothes that they wear. They may check in mirrors for hours and hours. I would certainly be concerned with any male taking steroids if there wasn't a legitimate indication for steroids, even if it was something such as trying to bulk up to play sports even if that's illegal. That would be something that would be an indication that is non-psychiatric. But men who are doing that just simply to bulk up, I would be very concerned about the possibility of BDD. Many of these compulsions that they do can involve excessive grooming, styling, plucking, shaving that can occur for hours a day. Touching affected areas. Asking for reassurance is one that can commonly happen. Note that 25% of BDD people will compulsively tan in order to hide skin defects. And of course, there are multiple medical morbidities associated with this including things like melanoma. Skin picking can also occur.
References:
- Phillips, K.A. (2011). Body Dysmorphic Disorder. In Hudak, R. & Dougherty, D. D. (Eds.) Clinical obsessive-compulsive disorders in adults and children (pp. 122–137). Cambridge University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 17
Now, BDD usually begins in early adolescence. Their preoccupations are similar. Note that 20% of people with BDD drop out of school because of their illness and 44% will report a suicide attempt. And it's important to note this because out of all the psychiatric disorders, you may be surprised to find out that BDD has the highest suicide rate of any other psychiatric disorders. The treatment is the same in children as adolescents although I think most clinicians may be more conservative about prescribing medications and want to give therapy a chance to work as a stand-alone treatment.
References:
- Phillips, K.A. (2011). Body Dysmorphic Disorder. In Hudak, R. & Dougherty, D. D. (Eds.) Clinical obsessive-compulsive disorders in adults and children (pp. 122–137). Cambridge University Press.
Slide 8 of 17
So again, a little more about suicidality. Eighty percent of people will have suicidal ideations and 25% of people with BDD will attempt suicide at some point. Dermatological patients who commit suicide have been found to have either acne or body dysmorphic disorder. The annual suicide rate for body dysmorphic disorder is 0.3% which is the highest among all psychiatric disorders. So know that when you're seeing with someone with BDD there's the real potential for lethality there.
References:
- Phillips, K.A. (2011). Body Dysmorphic Disorder. In Hudak, R. & Dougherty, D. D. (Eds.) Clinical obsessive-compulsive disorders in adults and children (pp. 122–137). Cambridge University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 17
The vast majority of patients with BDD will frequently seek surgery or dermatologic treatment. This can also include dental treatment for people who have BDD preoccupations concerning their mouth or teeth. This does not work. Obsessions will continue or focus on new areas. So plastic surgery or cosmetic treatments are not appropriate in people with body dysmorphic disorder. And to note, the reason for this is that 40% of surgeons have been threatened by BDD patients in the past. What will happen is someone with BDD will get very angry because their surgery didn't fix their problem. Because no surgery like this can fix a psychiatric issue, they become angry and can potentially become violent. I think as a result it's important to work with cosmetic surgeons and dental departments who frequently see these patients. I work with these departments in my university to make sure that these medical and surgical doctors are aware of this disorder. They need to be aware of this and they need to be aware of the extreme danger that they're in and that their patients are in if they perform inappropriate surgeries on them. I have some tips below.
References:
- Phillips, K. A., Wilhelm, S., Koran, L. M., Didie, E. R., Fallon, B. A., Feusner, J., & Stein, D. J. (2010). Body dysmorphic disorder: Some key issues for DSM-V. Depression and Anxiety, 27(6), 573-591.
Slide 10 of 17
Self-surgery. People with BDD will often perform self-surgery and this may be an exception to the rule that BDD patients look normal. If they perform self-surgery because of their severe obsessions, they may look scarred. Skin picking is one form of self-surgery but people have used pins, needles, razor blades, knives or any kind of implement possible.
References:
- Phillips, K. A., Wilhelm, S., Koran, L. M., Didie, E. R., Fallon, B. A., Feusner, J., & Stein, D. J. (2010). Body dysmorphic disorder: Some key issues for DSM-V. Depression and Anxiety, 27(6), 573-591.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 17
So some diagnostic questions. So there are some diagnostic questions that you can ask for your patients. Clinicians do not ask, "are you worried about an imagined defect in appearance?" by reading the criteria. That's a way to get someone to absolutely not want to engage with you. Ask instead, are you unhappy with how you look? Ask about all of the other areas of their body. Ask, does this concern preoccupy you? How much distress does these concerns cause you? Ask about common compulsions. Ask, do they tan, weightlift, conceal, touch themselves?
References:
- Phillips, K. A., Wilhelm, S., Koran, L. M., Didie, E. R., Fallon, B. A., Feusner, J., & Stein, D. J. (2010). Body dysmorphic disorder: Some key issues for DSM-V. Depression and Anxiety, 27(6), 573-591.
Slide 12 of 17
Obviously, you need to rule out eating disorders. And screen of course for OCD, major depression, social anxiety disorder, substance use. While there is some self-harm in these BDD patients, you can very easily most of the time distinguish between this and borderline personality disorder. The self-harm in borderline personality disorder tends to reduce anxiety. With BDD, however, the self-harm only makes the anxiety increase more. Like the compulsion is, it doesn't cause relief.
References:
- Phillips, K. A., Wilhelm, S., Koran, L. M., Didie, E. R., Fallon, B. A., Feusner, J., & Stein, D. J. (2010). Body dysmorphic disorder: Some key issues for DSM-V. Depression and Anxiety, 27(6), 573-591.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 17
There are no rating scales or lab testing in common use at this time for BDD. You need to establish an alliance with these patients. Take their concerns seriously. Don't dismiss them. Explain what BDD is and how it applies to them. Tell them that the focus is to decrease their excessive preoccupation. So what you want to do is get their focus away from their bodies so that they're not upset all the time. And I tend to tread pretty lightly with them.
References:
- Phillips, K. A., Wilhelm, S., Koran, L. M., Didie, E. R., Fallon, B. A., Feusner, J., & Stein, D. J. (2010). Body dysmorphic disorder: Some key issues for DSM-V. Depression and Anxiety, 27(6), 573-591.
Slide 14 of 17
I'll give them the formal diagnosis. I will let them know that they can feel better and emphasize feeling better rather than emphasizing appearance. I usually ask them to get a copy of a book, a famous book called the Broken Mirror by Katharine Phillips as an educational tool in teaching them. I always recommend against surgery. And if they don't want to hear that, I ask them to please at least delay surgery until after treatment. I give them treating recommendations and I explain that there are effective interventions. I let them know that the interventions for this disorder indeed can work and can help them feel better.
References:
- Phillips, K. A., Wilhelm, S., Koran, L. M., Didie, E. R., Fallon, B. A., Feusner, J., & Stein, D. J. (2010). Body dysmorphic disorder: Some key issues for DSM-V. Depression and Anxiety, 27(6), 573-591.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 17
Key points. Body dysmorphic disorder is a serious illness in which the patients are overly concerned about their appearance and have rituals that cover up how they look. There are serious medical comorbidities involved including inappropriate surgeries. The suicide rate for BDD may be the highest of all psychiatric disorders.
Slide 16 of 17
Forty percent of surgeons report having received threats from body dysmorphic disorder patients making them a homicide risk as well. Screening and diagnostic questions have to be framed in a way not to offend or anger the patient. Cosmetic treatments should always be discouraged even in the presence of actual physical deficits until treatment has been completed. Thank you.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.