Slides and Transcript
Slide 1 of 15
So, we've been talking about the technical principles of Psychodynamic Psychopharmacology. So far, we've covered the first two of the six principles: avoiding a mind-body split and knowing who the patient is. We're going to move on to the next principles. In this section, we're going to begin to look at particularly the issues around ambivalence, in prescribing.
Slide 2 of 15
In terms of ambivalence, it's probably important to recognize that for many and probably most of our patients there is some degree of ambivalence about treatment. I don't want to take medications and most of my patients don't want to take medications, so there's some built-in ambivalence just right there. But more than that, our patients especially, many of whom have had negative early experiences or have been harmed by caregiving, they have a lot of worries.
References:
- Mintz, D. (2022). Psychodynamic Psychopharmacology: Caring for the Treatment-Resistant Patient. American Psychiatric Pub.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
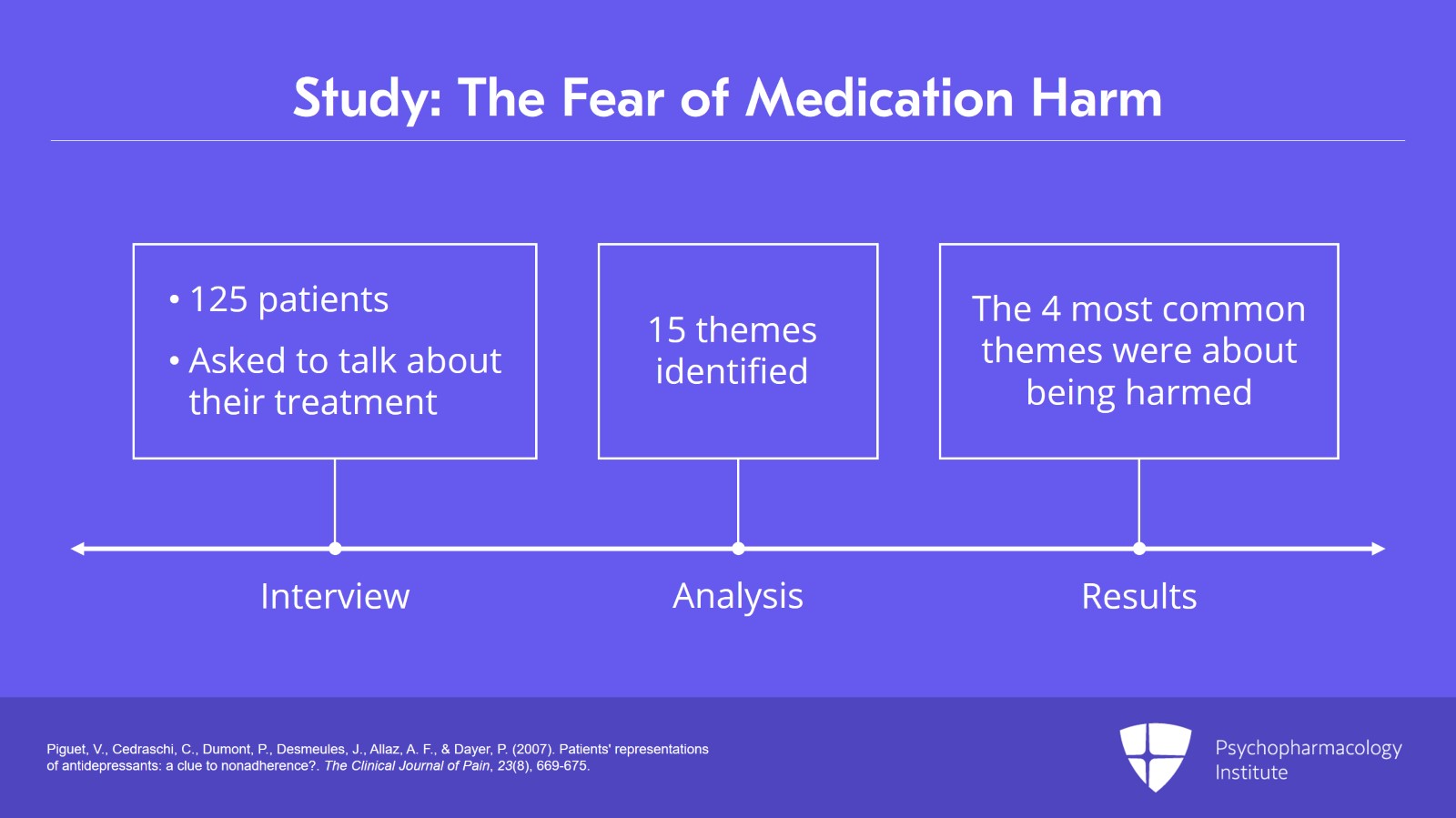
Slide 3 of 15
And interestingly, a study by Piguet, a sociologist who interviewed something like 125 patients with a history of depression who had been prescribed medications, did an open-ended factor analytic study where they just asked patients to talk about their treatment with medications. And then, they collated the 125 or so interviews and identified 15 themes that kind of ran through those interviews. Of those 15 themes, the four most common themes when people discussed their medications were all about being harmed. It took to the fifth theme, the fifth most common theme, to start hearing from patients about ways they felt their treatments benefited them.
References:
- Piguet, V., Cedraschi, C., Dumont, P., Desmeules, J., Allaz, A. F., & Dayer, P. (2007). Patients' representations of antidepressants: a clue to nonadherence?. The Clinical Journal of Pain, 23(8), 669-675.
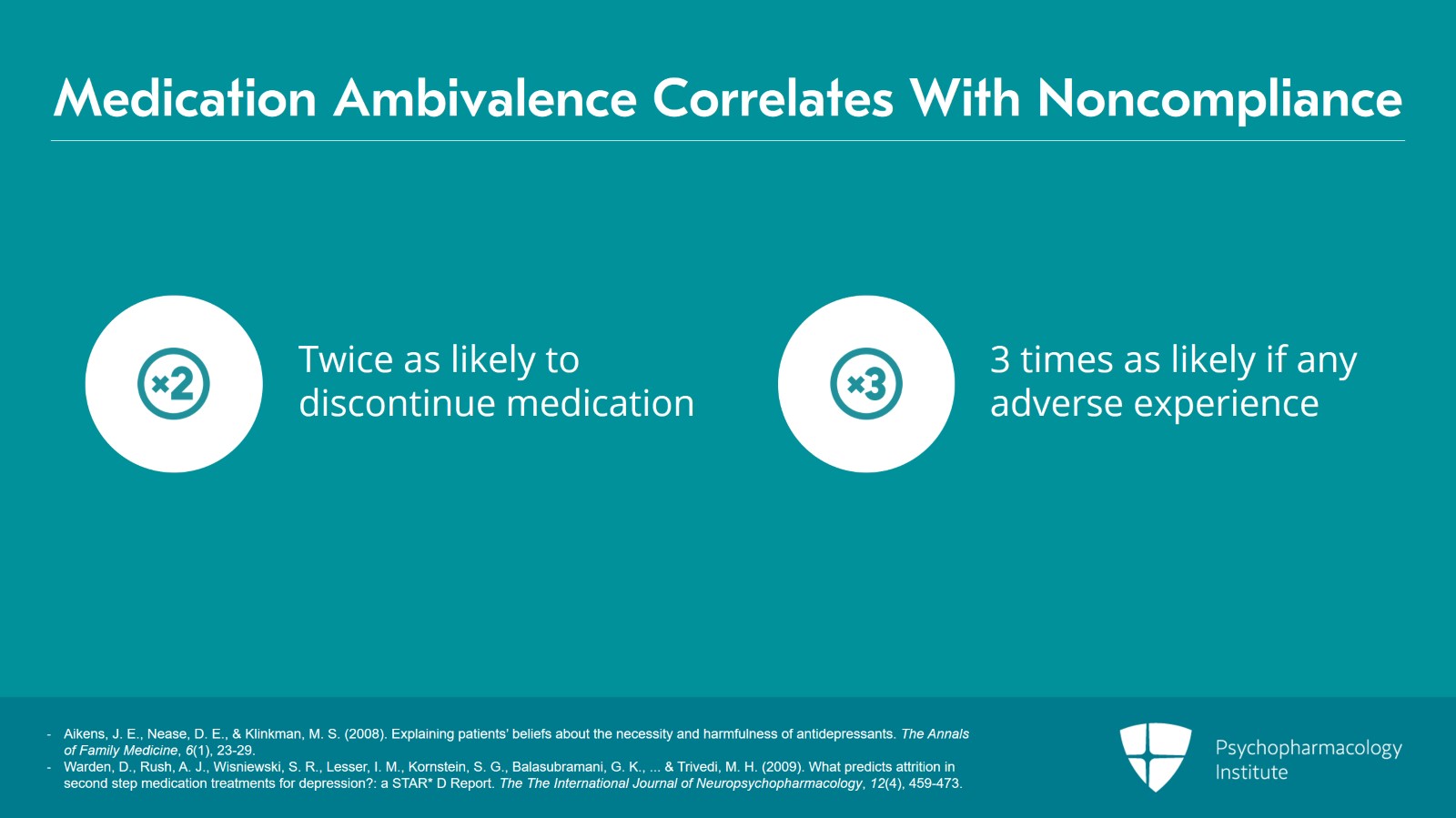
Slide 4 of 15
So, this kind of thing is happening and our patients are bringing in all sorts of complicated anxious feelings about. And we know that the patient's ambivalence is directly corelated with noncompliance, so patients who come in with ambivalence are already from the outset twice as likely to discontinue medications and three times as likely to discontinue medications if they have any kind of adverse experience at all.
References:
- Aikens, J. E., Nease, D. E., & Klinkman, M. S. (2008). Explaining patients’ beliefs about the necessity and harmfulness of antidepressants. The Annals of Family Medicine, 6(1), 23-29.
- Warden, D., Rush, A. J., Wisniewski, S. R., Lesser, I. M., Kornstein, S. G., Balasubramani, G. K., … & Trivedi, M. H. (2009). What predicts attrition in second step medication treatments for depression?: a STAR* D Report. The The International Journal of Neuropsychopharmacology, 12(4), 459-473.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 15
But our patients bring in ambivalences also about illness. When patients are ambivalent about illness, when they do get sick in some way they might discover there are secondary gains. You know, when you get those lemons, you kind of figure out how to make some lemonade from it. And once that happens, those patients who are getting secondary gains from their illness are less likely to recover. And we know that the patient's readiness to change exerts an important influence on whether or not medication treatment is going to work.
References:
- Van Egmond, J., & Kummeling, I. (2002). A blind spot for secondary gain affecting therapy outcomes. European Psychiatry, 17(1), 46-54.
Slide 6 of 15
And patients can also be ambivalent about caregiving. So, they've had early adverse experiences, and early trauma is correlated with increased treatment resistance. And, as I said in a previous lecture, there are also legacies of systemic oppression. Patients are bringing that legacy in in the form of medical mistrust, that makes the patients perhaps less able to make use of the treatments we have to offer. And, of course, if we're not mindful, we can also end up enacting those aspects of systemic oppression and actually contributing to the problem rather than helping to fix it.
References:
- Williams, D. R., & Collins, C. (2016). Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Reports.
- Sirey, J. A., Bruce, M. L., Alexopoulos, G. S., Perlick, D. A., Friedman, S. J., & Meyers, B. S. (2001). Stigma as a barrier to recovery: Perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatric Services, 52(12), 1615-1620.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 15
So, some of the things that we do around ambivalence is that we want to attend to it, and a simple way to do that early on is: ask the patient what their feelings are about taking medications. And, very often, patients will tell you right away about their ambivalences. And this, again, is not something that should take a lot of time. This can be part of an initial interview and it takes two minutes maybe to get a sense for how patients feel about taking medications.
References:
- Mintz, D. (2022). Psychodynamic Psychopharmacology: Caring for the Treatment-Resistant Patient. American Psychiatric Pub.
- Mintz, D., & Belnap, B. (2006). A view from Riggs: Treatment resistance and patient authority—III. What is psychodynamic psychopharmacology? An approach to pharmacologic treatment resistance. Journal of the American Academy of Psychoanalysis and Dynamic Psychiatry, 34(4), 581-601.
Slide 8 of 15
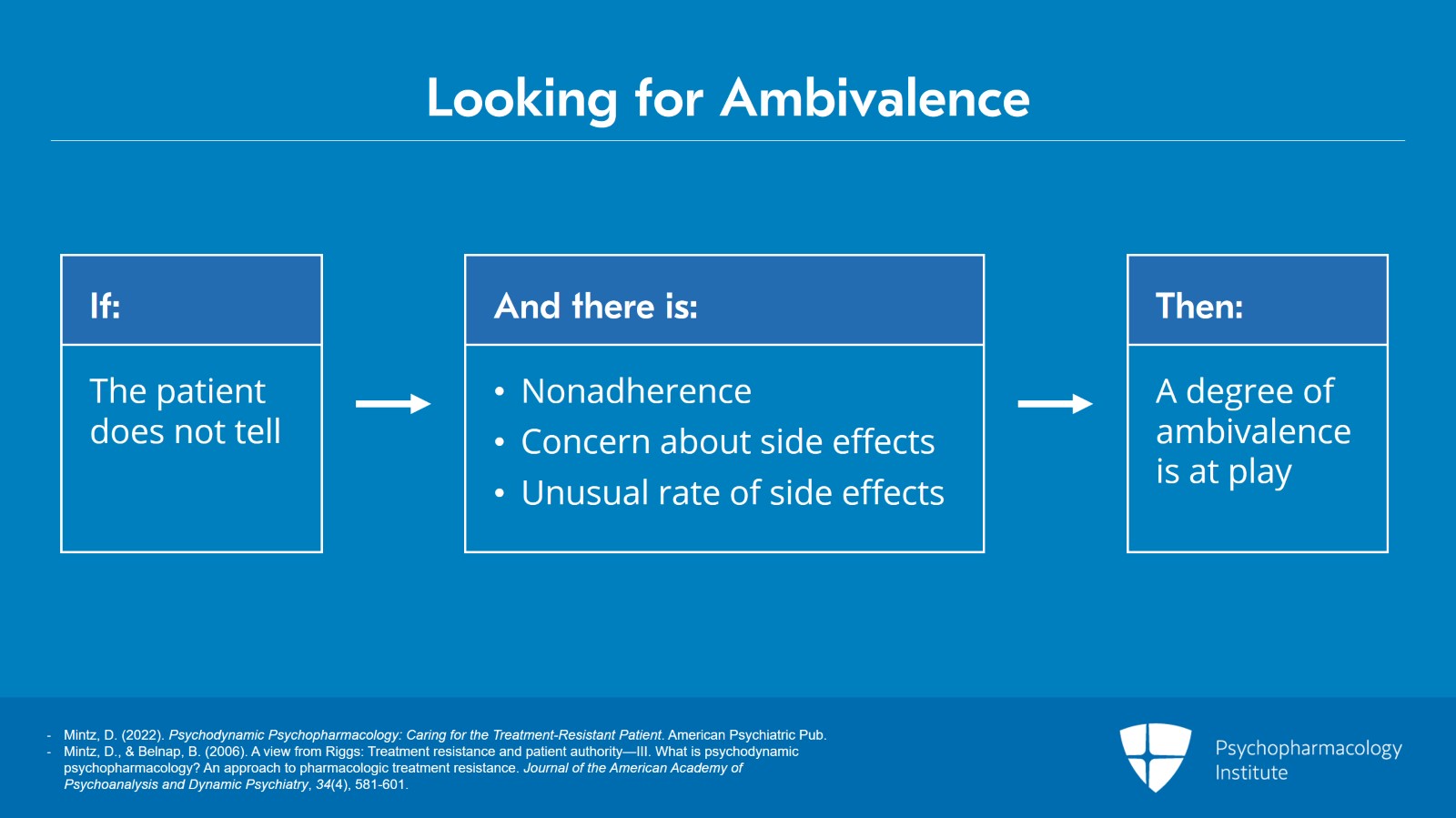
We also want to be on the lookout for evidence of ambivalence if the patient does not tell us about it, if there's nonadherence, or patients are bringing in a lot of concern about side effects, or other aspects of treatment, or they're having side effects at a rate that doesn't necessarily make pharmacologic sense or raises questions for us about whether these are nocebo responses. All of these things should alert us to the possibility that there's a degree of ambivalence at play that's interfering with the patient's ability to make healthy use of medications.
References:
- Mintz, D. (2022). Psychodynamic Psychopharmacology: Caring for the Treatment-Resistant Patient. American Psychiatric Pub.
- Mintz, D., & Belnap, B. (2006). A view from Riggs: Treatment resistance and patient authority—III. What is psychodynamic psychopharmacology? An approach to pharmacologic treatment resistance. Journal of the American Academy of Psychoanalysis and Dynamic Psychiatry, 34(4), 581-601.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 15
Once we start to suspect that it may be there, we're looking for whether there may be secondary gains, all the kinds of things that interfere with other more primary rewards from the world. We may want to start wondering whether symptoms are serving defensive functions for the patient or helping to manage intolerable affects.
References:
- Mintz, D. (2022). Psychodynamic Psychopharmacology: Caring for the Treatment-Resistant Patient. American Psychiatric Pub.
Slide 10 of 15
Or, wonder whether symptoms are serving as communications, or some kind of currency in a doctor-patient relationship. You can imagine a patient who is reluctant to get better because when they come to you, as a doctor you're the one person, the one time in their month where somebody just is interested and concerned and caring. And so, the patient may be reluctant to give up their symptoms because that's their way of saying "I need your care“.
References:
- Mintz, D. (2022). Psychodynamic Psychopharmacology: Caring for the Treatment-Resistant Patient. American Psychiatric Pub.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 15
Or, conversely, the patient has a lot of early adverse experiences and a real chip on their shoulder about caregiving, and so they're invested in showing how you can't trust caregivers, you can't turn to caregivers, nobody really helps you, you're on your own. And so, that patient may also use their symptoms to try to communicate something about their anger, about the ineffectiveness of caregiving that you can get in the world including from you, their doctor.
References:
- Mintz, D. (2022). Psychodynamic Psychopharmacology: Caring for the Treatment-Resistant Patient. American Psychiatric Pub.
- Mintz, D. L., & Flynn, D. F. (2012). How (not what) to prescribe: nonpharmacologic aspects of psychopharmacology. Psychiatric Clinics, 35(1), 143-163.
Slide 12 of 15
Another way to get at ambivalence is simply to inquire. What does the patient stand to lose if treatment works? Now, on this one in particular, I think it is crucial if you're going to ask this question that you ask it in the first session, or maybe second session, before any transferences emerge, before you've gotten frustrated by their nonresponse or they've gotten frustrated by their nonresponse, because then, if you ask the question, what do you stand to lose if treatment works, they hear it defensively and probably rightly so, because it starts to have some blame to it.
References:
- Mintz, D. L., & Flynn, D. F. (2012). How (not what) to prescribe: nonpharmacologic aspects of psychopharmacology. Psychiatric Clinics, 35(1), 143-163.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 15
So, key points from this lecture: From a psychodynamic perspective, patients like all people have conflicts that may complicate many aspects of their lives including their use of psychiatric care. Ambivalence about medications, doctors, care, or even health itself contributes to treatment refractoriness.
Slide 14 of 15
So some of the things that we do around ambivalence is that we want to attend to it. A simple way to do that early on is ask the patient what their feelings are about taking medications. Also, be on the lookout for evidence of ambivalence if the patient does not tell us about it.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.