Slides and Transcript
Slide 1 of 21
In section 4, we will discuss assessing adherence including self-report, a variety of standardized rating scales, monitoring medication refills, automated pill taking, frequency monitoring, medication routines, and the duration of a variety of assessments.
So, there are a lot of different ways to assess medication treatment adherence.
Slide 2 of 21
One of the most common and one we typically use in clinical settings is self-reported adherence. So, we ask the patient. Language is important when assessing for medication adherence.
For example, a person has bipolar disorder or has schizophrenia. They are not bipolar or schizophrenic. That kind of robs the person of their individual identity and may actually unintentionally bias reporting such that the person is not candid with their clinician.
References:
- Sajatovic, M., Jenkins, J. H., Cassidy, K. A., & Muzina, D. J. (2009). Medication treatment perceptions, concerns and expectations among depressed individuals with type I bipolar disorder. Journal of Affective Disorders, 115(3), 360-366.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 21
The term adherence is generally preferred over the term compliance as it is more of a partnership language.
And we optimally will normalize asking about missed medication, for example, saying something along the lines of, “Many people forget to take their medications at times. Does that ever happen to you?” And that’s a higher yield way than simply asking, you know, “Do you forget to take your medications?”
References:
- Sajatovic, M., Jenkins, J. H., Cassidy, K. A., & Muzina, D. J. (2009). Medication treatment perceptions, concerns and expectations among depressed individuals with type I bipolar disorder. Journal of Affective Disorders, 115(3), 360-366.
Slide 4 of 21
There is a body of research that addresses the question of: Can physicians identify poorly adherent patients?
So, correlations between electronic medication taking monitoring system such as one called the MEM System which is Medication Events Monitoring.
There are a variety of commercial devices that can assess this. But correlations between MEMS and physician impressions of adherence have been reported to be non-significant or minimal.
And using that standard 80% cutoff that I discussed earlier, physicians were unable to dichotomize or divide people into groups of adherent versus non-adherent groups. So, we think that we can really accurately assess adherence among our patients, but the data does not, in fact, suggest that that is the case.
References:
- Byerly, M., Fisher, R., Whatley, K., Holland, R., Varghese, F., Carmody, T., Magouirk, B., & Rush, A. J. (2005). A comparison of electronic monitoring vs. clinician rating of antipsychotic adherence in outpatients with schizophrenia. Psychiatry Research, 133(2-3), 129-133.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 21
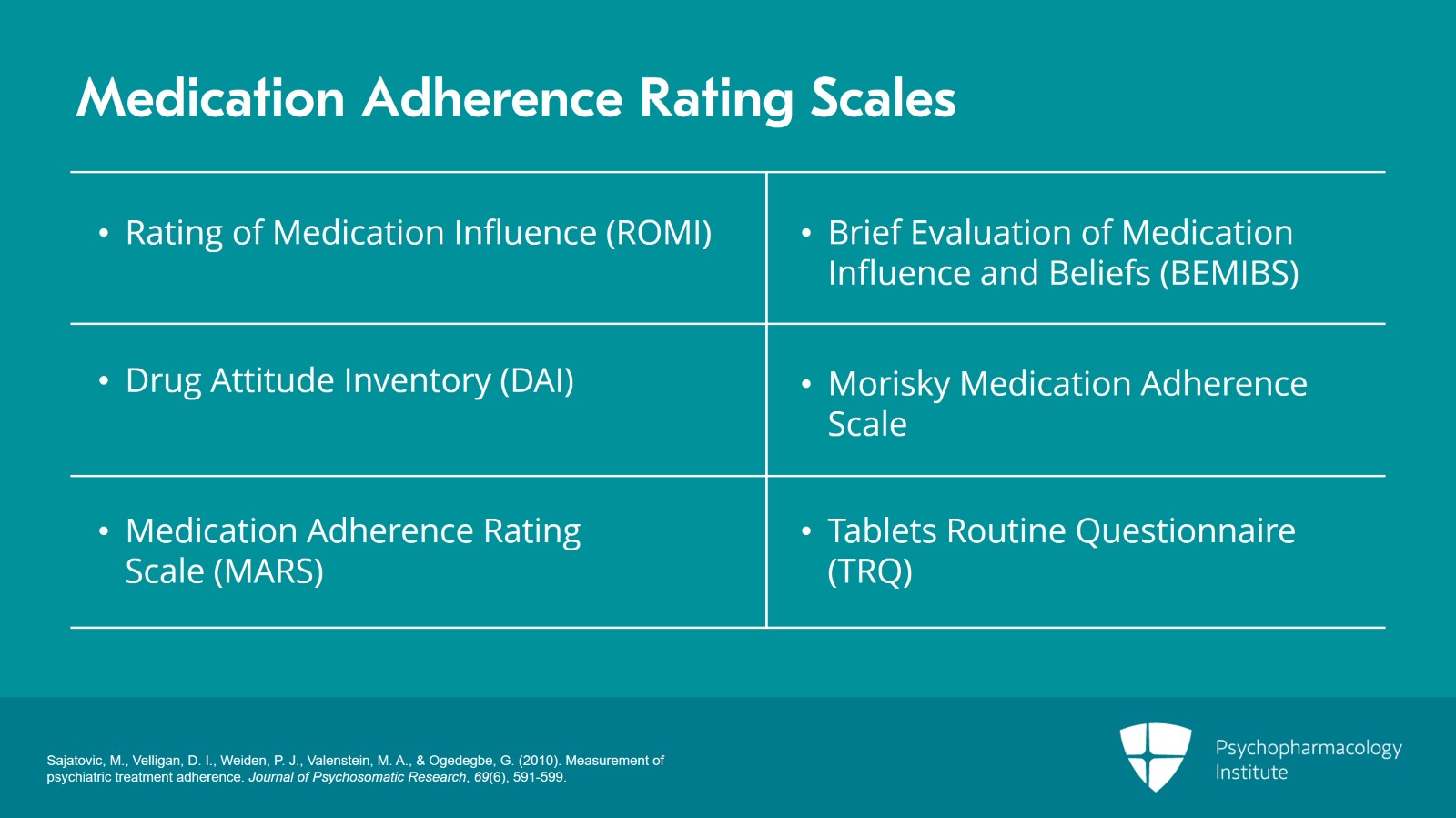
Our next slide shows some examples of medication adherence rating scales, Rating of Medication Influence or ROMI, Drug Attitude Inventory or DAI, the Medication Adherence Rating Scale or MARS.
Brief Evaluation of Medication Influence and Beliefs or BEMIBS, Morisky Adherence, and Tablets Routine Questionnaire or TRQ.
References:
- Sajatovic, M., Velligan, D. I., Weiden, P. J., Valenstein, M. A., & Ogedegbe, G. (2010). Measurement of psychiatric treatment adherence. Journal of Psychosomatic Research, 69(6), 591-599.
Slide 6 of 21
Those vary in number of items, their mode of administration. Most are self-report. They can take up to 15 minutes to administer and they have mixed reliability and validity ratings.
References:
- Sajatovic, M., Velligan, D. I., Weiden, P. J., Valenstein, M. A., & Ogedegbe, G. (2010). Measurement of psychiatric treatment adherence. Journal of Psychosomatic Research, 69(6), 591-599.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 21
These are probably more likely to be used in research although clinicians might use the MARS or the BEMIBS more often.
We do not tend to use the Morisky in our adherence research just because of copyright issues.
And then some of them do require some backend calculations like the Tablets Routine Questionnaire where you ask questions and then you actually calculate a percentage.
References:
- Sajatovic, M., Velligan, D. I., Weiden, P. J., Valenstein, M. A., & Ogedegbe, G. (2010). Measurement of psychiatric treatment adherence. Journal of Psychosomatic Research, 69(6), 591-599.
Slide 8 of 21
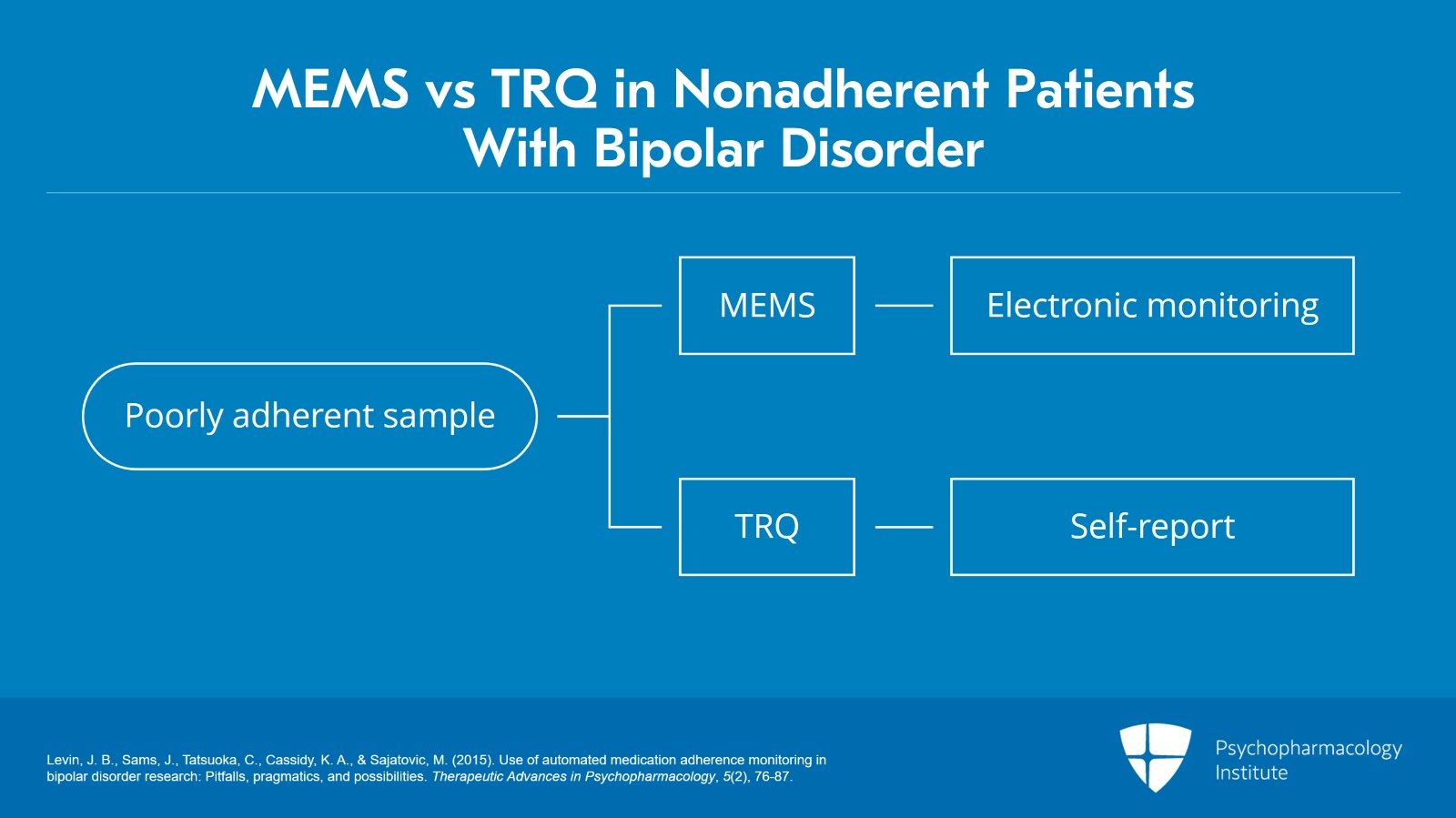
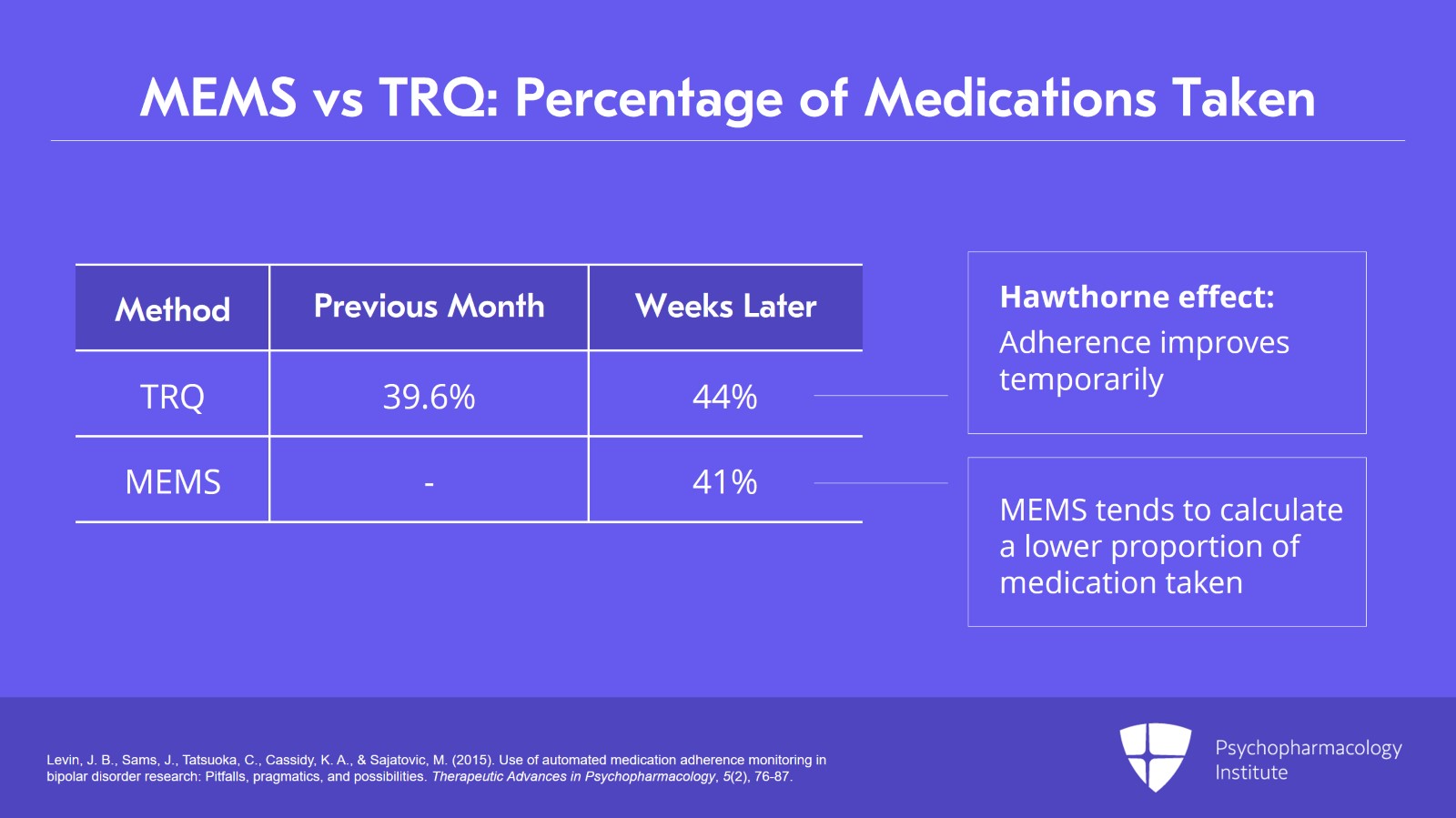
The next slide is some research data from our team. We looked at the automated pill monitoring or MEMS versus the Tablets Routine Questionnaire or TRQ in non-adherent patients with bipolar disorder.
So, this was a deliberately enrolled poorly adherent sample and we basically compared MEMS, which is electronic monitoring versus TRQ, which is self-report.
References:
- Levin, J. B., Sams, J., Tatsuoka, C., Cassidy, K. A., & Sajatovic, M. (2015). Use of automated medication adherence monitoring in bipolar disorder research: Pitfalls, pragmatics, and possibilities. Therapeutic Advances in Psychopharmacology, 5(2), 76-87.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 21
And what I really would like to draw your attention to is this is looking at the percent of medications taken. So, if we look at the TRQ in the past month, for instance, you know, patients talked about taking close to 40% or 39.6%.
Looking at them a couple of weeks later, we see that they’re up to 44%. Something called the Hawthorne effect, and this is when you start to monitor people and ask them about adherence, their adherence will improve usually only temporarily.
And the other take-home message that I would say here is that MEMS tends to calculate a lower proportion of medication taken versus self-report. So, MEMS calculated was 41% versus the TRQ which might be anywhere from 44 to 44.9%. So electronic monitoring tends to have lower findings.
References:
- Levin, J. B., Sams, J., Tatsuoka, C., Cassidy, K. A., & Sajatovic, M. (2015). Use of automated medication adherence monitoring in bipolar disorder research: Pitfalls, pragmatics, and possibilities. Therapeutic Advances in Psychopharmacology, 5(2), 76-87.
Slide 10 of 21
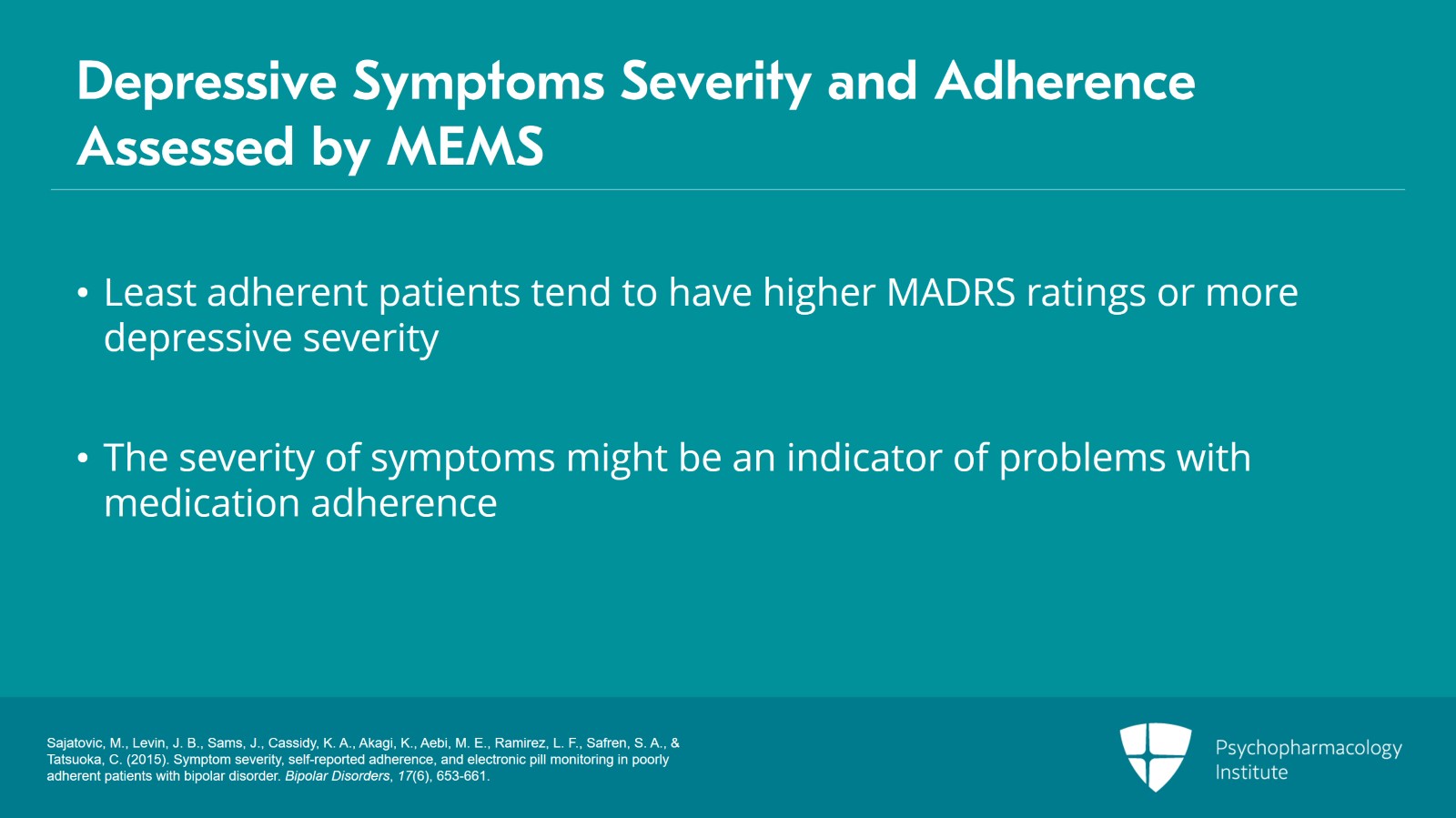
Assessment of depressive symptoms severity as measured by the Montgomery-Asberg Depression Rating Scale associated with adherence as assessed by MEMS.
So least adherent tended to have higher MADRS ratings or more depressive severity.
So, patients who tend to have more severe symptoms may be less adherent. Somebody could still be poorly responsive to a given medication, but it might be one indicator that a clinician can use along with your other data to help you decide if the person is having problems with medication adherence.
References:
- Sajatovic, M., Levin, J. B., Sams, J., Cassidy, K. A., Akagi, K., Aebi, M. E., Ramirez, L. F., Safren, S. A., & Tatsuoka, C. (2015). Symptom severity, self-reported adherence, and electronic pill monitoring in poorly adherent patients with bipolar disorder. Bipolar Disorders, 17(6), 653-661.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 21
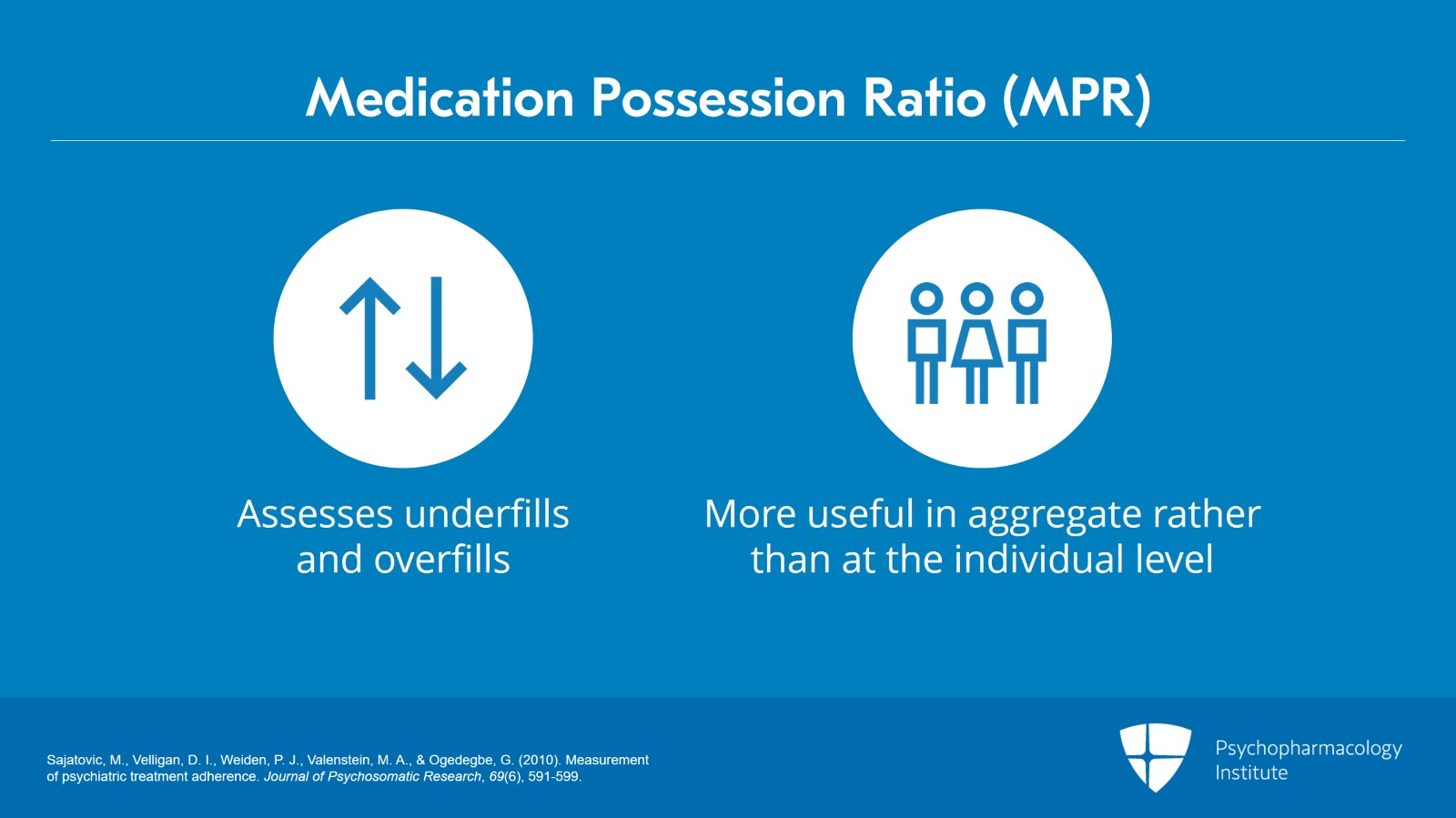
I just do want to mention a couple of things about the Medication Possession Ratio or MPR.
We did cover those in an earlier slide, but this is important because you’ll see this in the literature. The MPR assesses underfills as well so prescriptions not refilled frequently enough as well as overfills. So, it can look at both categories.
It is probably more useful in aggregate rather than in individual level. So, if you’ll look at, you know, say, all the patients in a given clinic, you could help identify when they are most vulnerable to poor adherence.
References:
- Sajatovic, M., Velligan, D. I., Weiden, P. J., Valenstein, M. A., & Ogedegbe, G. (2010). Measurement of psychiatric treatment adherence. Journal of Psychosomatic Research, 69(6), 591-599.
Slide 12 of 21
As I’ve mentioned before, there’s no guarantee that drug is ingested just because somebody goes to the pharmacy or picks up a medication. And in some systems, they’re automatically mailed out so people could have, you know, a storage room full of medication bottles.
The MPR is also an opportunity for the pharmacist to get involved and intervene, so for instance, if somebody does not fill their medication on time.
References:
- Sajatovic, M., Velligan, D. I., Weiden, P. J., Valenstein, M. A., & Ogedegbe, G. (2010). Measurement of psychiatric treatment adherence. Journal of Psychosomatic Research, 69(6), 591-599.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 21
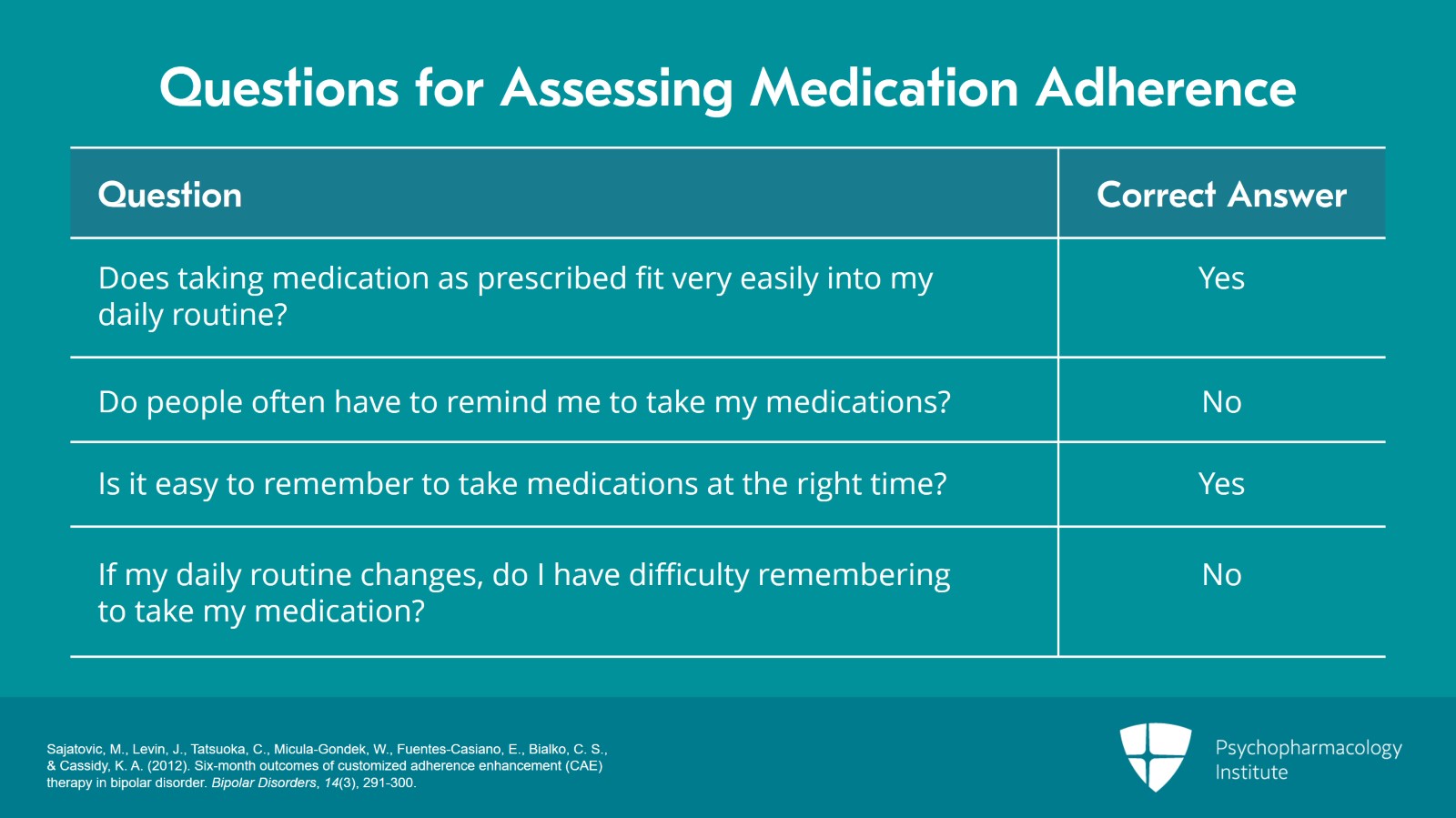
I want to give you some sample questions that you can use in assessing medication adherence.
So, what we use in some of our assessments with the medication routines question is number one, taking medication as prescribed fits in very easily with my daily routine. So, ask them if they agree with this, yes or no. The correct answer would be yes.
Second question, people often have to remind me to take my medications. You know, does this happen to you? The correct answer is no.
Is it easy to remember to take medications at the right time? The correct answerer is yes.
And, if my daily routine changes, do I have difficulty remembering to take my medication? So correct answer is no.
And in our research, we actually give people these questions and ask them to respond to them.
References:
- Sajatovic, M., Levin, J., Tatsuoka, C., Micula-Gondek, W., Fuentes-Casiano, E., Bialko, C. S., & Cassidy, K. A. (2012). Six-month outcomes of customized adherence enhancement (CAE) therapy in bipolar disorder. Bipolar Disorders, 14(3), 291-300.
Slide 14 of 21
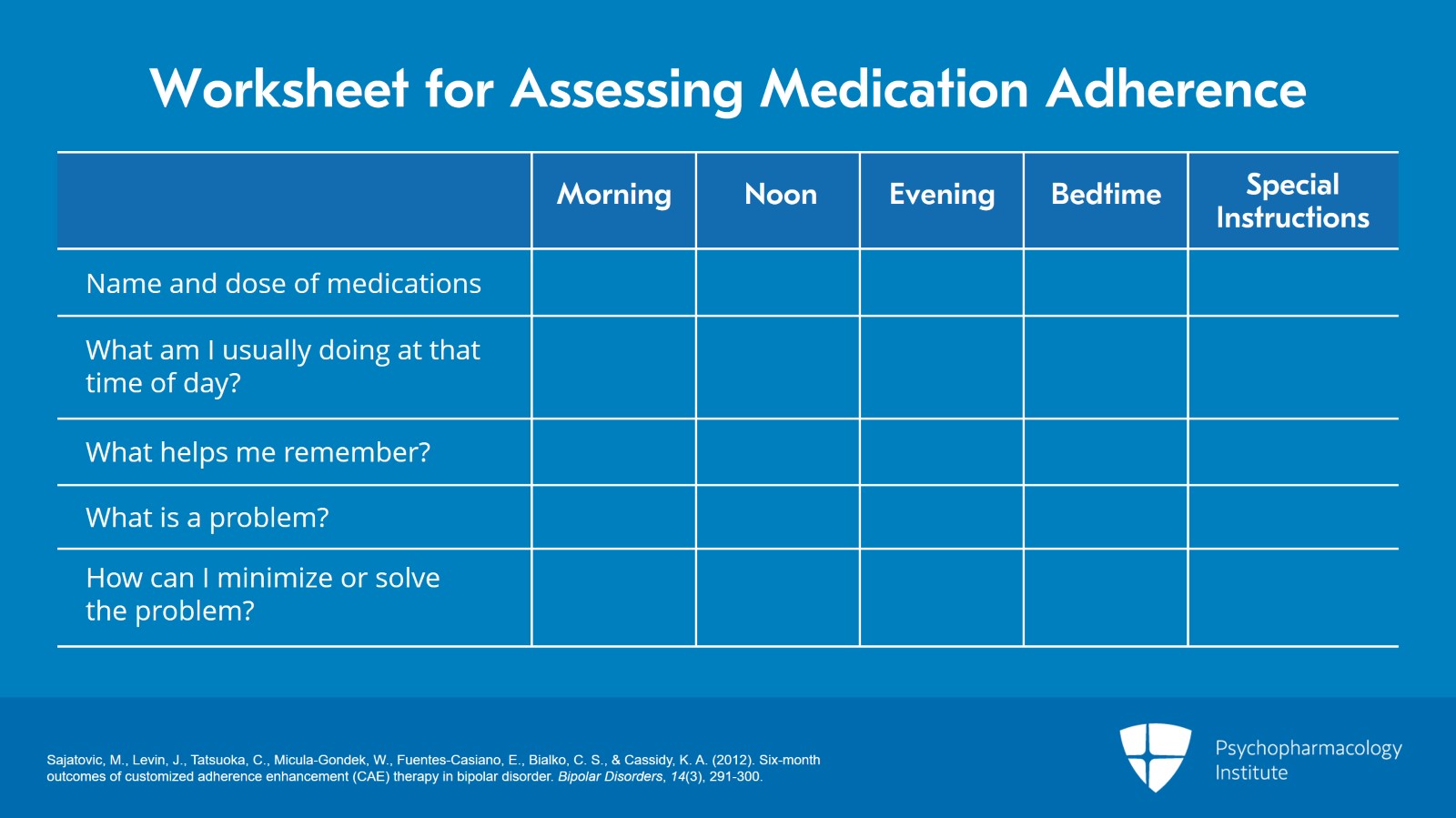
The next slide shows a worksheet that we use in our research settings.
So, we have people identify their name and dose of medications, what they’re doing at that time of day, what helps me remember and what is the problem and then their own problem solving and how they can minimize or solve the problem.
So, you know, looking at all the medications and one by one evaluating whether there are lifestyle or medication routine barriers.
So, clinicians can use a checklist like this, or they can just ask. You know, what are you usually doing when you’re, you know, when you need to take your medication? And is there a way to link it into a routine that you have in your life?
References:
- Sajatovic, M., Levin, J., Tatsuoka, C., Micula-Gondek, W., Fuentes-Casiano, E., Bialko, C. S., & Cassidy, K. A. (2012). Six-month outcomes of customized adherence enhancement (CAE) therapy in bipolar disorder. Bipolar Disorders, 14(3), 291-300.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 21
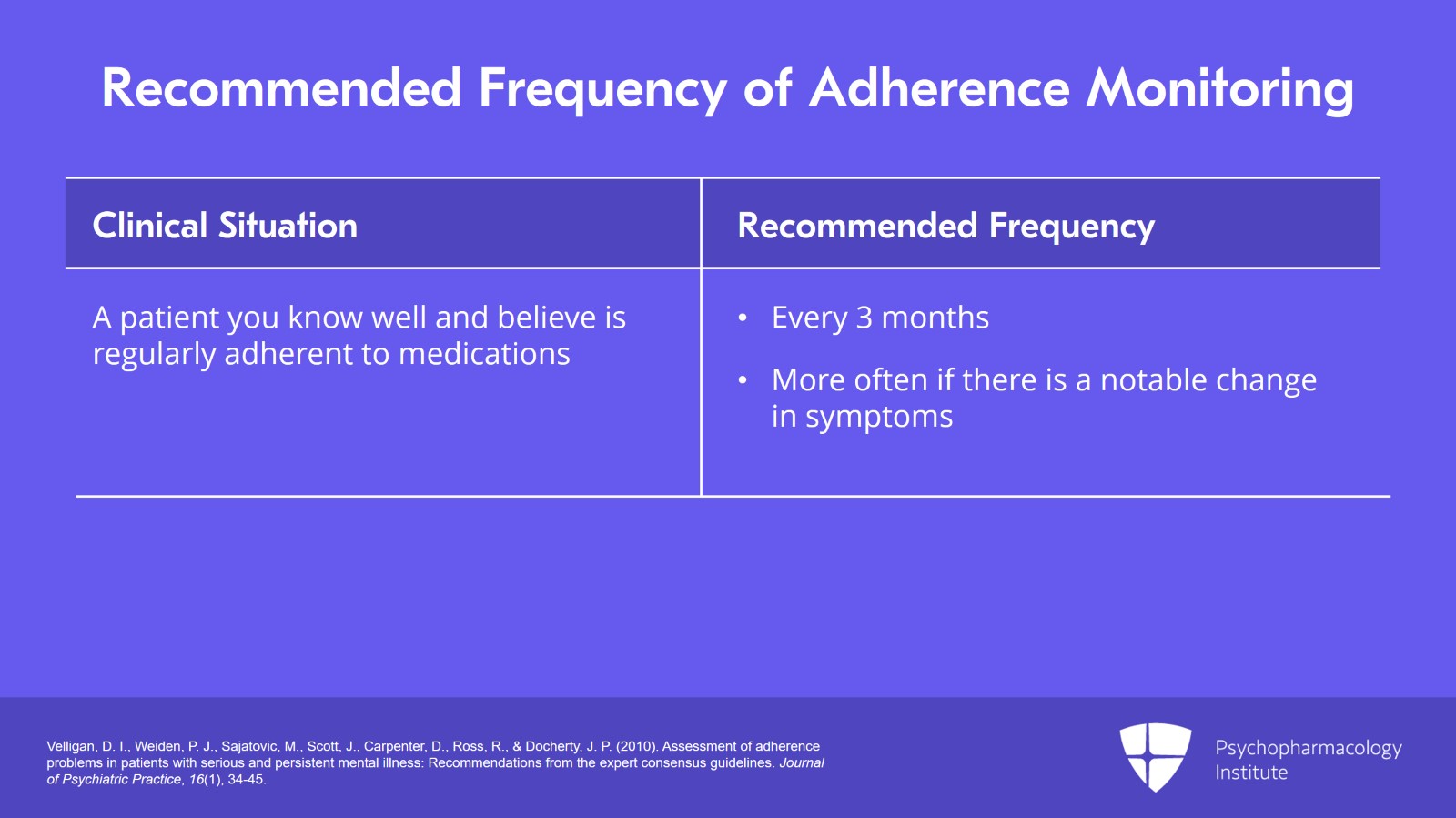
The next slide shows some clinical situations with recommended frequency of adherence monitoring.
So, if you have a clinical situation where a patient you know well and believe is regularly adherent to medications, the recommendation is that can be potentially built into a routine of maybe every three months if they’re seen monthly, maybe more often if there’s a notable change in symptoms. This should be something that, you know, might be a briefer portion of the med check or visit, five minutes or less.
References:
- Velligan, D. I., Weiden, P. J., Sajatovic, M., Scott, J., Carpenter, D., Ross, R., & Docherty, J. P. (2010). Assessment of adherence problems in patients with serious and persistent mental illness: Recommendations from the expert consensus guidelines. Journal of Psychiatric Practice, 16(1), 34-45.
Slide 16 of 21
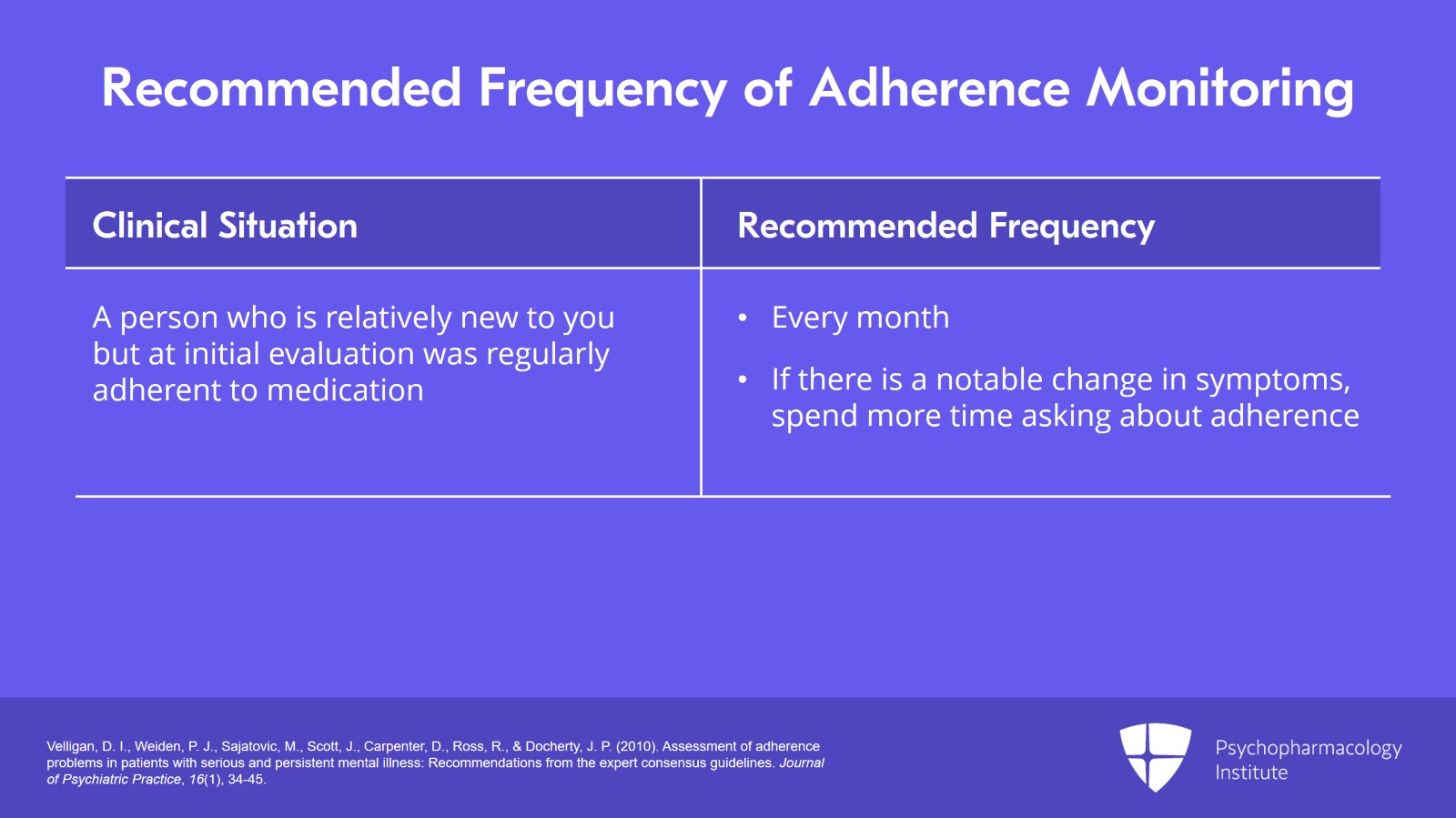
Or a person who’s relatively new to you but at initial evaluation was regularly adherent to medication, maybe a month later. Or if there’s a notable change in symptoms, you might spend a little more time asking about adherence.
References:
- Velligan, D. I., Weiden, P. J., Sajatovic, M., Scott, J., Carpenter, D., Ross, R., & Docherty, J. P. (2010). Assessment of adherence problems in patients with serious and persistent mental illness: Recommendations from the expert consensus guidelines. Journal of Psychiatric Practice, 16(1), 34-45.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 21
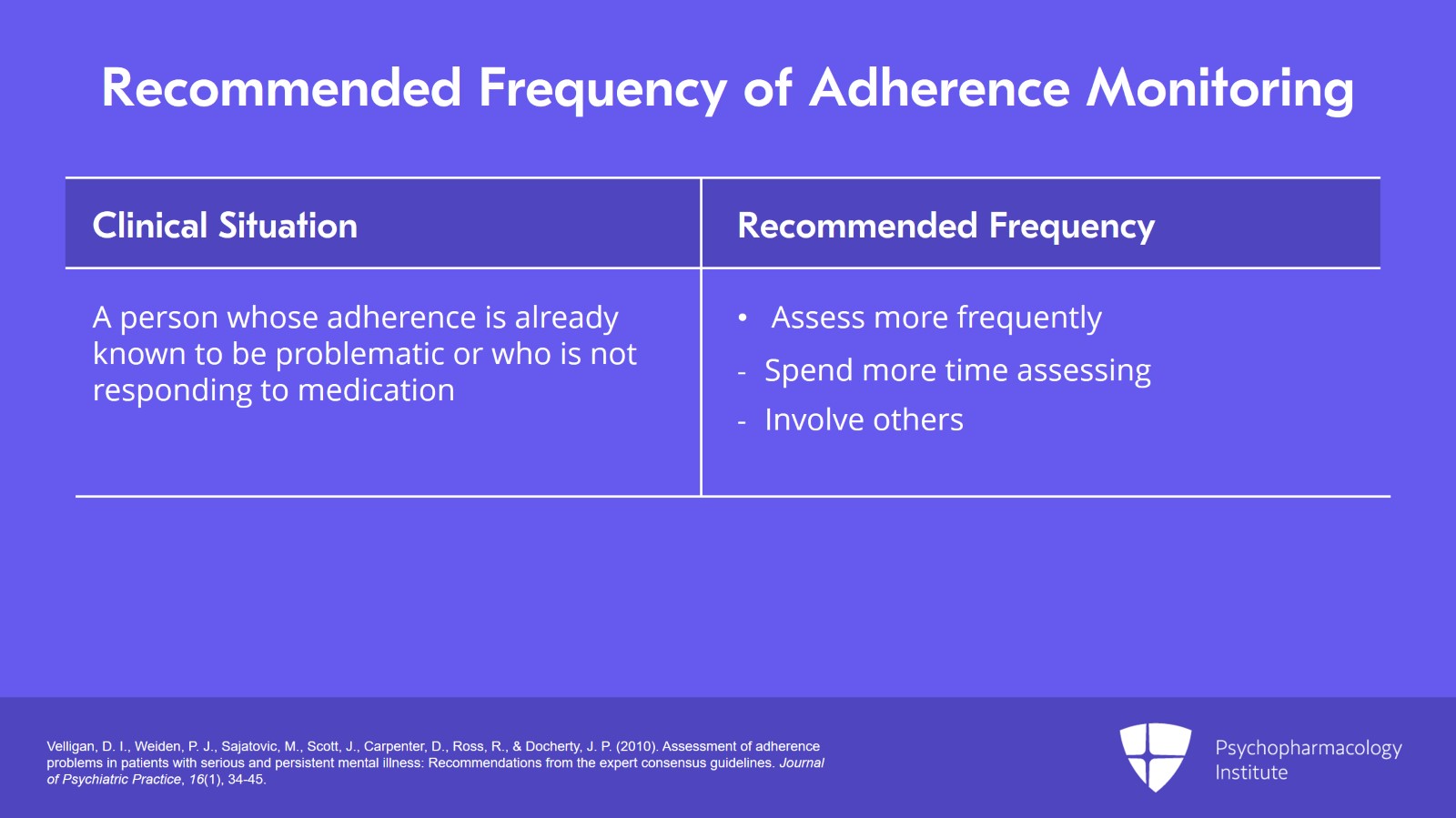
And then the last two categories, a person whose adherence is already known to be problematic or a person who is not responding to medication, you might want to assess more frequently, spend more time, you know, maybe, you know, more than 10 minutes.
You might want to involve others or maybe even do daily checks depending if the person is in a program like a PACT program, Program of Assertive Community Treatment.
References:
- Velligan, D. I., Weiden, P. J., Sajatovic, M., Scott, J., Carpenter, D., Ross, R., & Docherty, J. P. (2010). Assessment of adherence problems in patients with serious and persistent mental illness: Recommendations from the expert consensus guidelines. Journal of Psychiatric Practice, 16(1), 34-45.
Slide 18 of 21
So, adherence assessment should ideally be linked to what is going on with your patient at that particular time.
References:
- Velligan, D. I., Weiden, P. J., Sajatovic, M., Scott, J., Carpenter, D., Ross, R., & Docherty, J. P. (2010). Assessment of adherence problems in patients with serious and persistent mental illness: Recommendations from the expert consensus guidelines. Journal of Psychiatric Practice, 16(1), 34-45.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 21
The key point here is that there is no single perfect method to assess treatment adherence.
Sometimes, combined assessments, you know, self-report and other measures can be used.
Self-report is easiest but needs to be done using approaches that are collaborative and nonjudgmental.
Slide 20 of 21
So how you ask the question and how you talk to the patient are important. Assessments need to be done repeatedly. And symptom flareup may be an indicator to reassess adherence.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.