Slides and Transcript
Slide 1 of 19
In this third video, I will discuss the appropriate use of benzodiazepines including their indications and optimal selection.
Slide 2 of 19
When considering the first-line indications for prescribing benzodiazepines, there are several.
Benzodiazepines are first line for managing withdrawal from benzodiazepines as well as from alcohol. They are indicated for treating status epilepticus, crisis anxiety without psychotic features, procedure anesthesia.
References:
- Holbrook, A. M., Crowther, R., Lotter, A., Cheng, C., & King, D. (1999). Meta-analysis of benzodiazepine use in the treatment of acute alcohol withdrawal. Canadian Medical Association Journal, 160(5), 649–655.
- Prasad, M., Krishnan, P. R., Sequeira, R., & Al-Roomi, K. (2014). Anticonvulsant therapy for status epilepticus. Cochrane Database of Systematic Reviews, 2014(9).
- Messina, A. G., Wang, M., Ward, M. J., Wilker, C. C., Smith, B. B., Vezina, D. P., & Pace, N. L. (2016). Anaesthetic interventions for prevention of awareness during surgery. Cochrane Database of Systematic Reviews, 2016(10).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 19
They’re first-line treatment in certain acute movement disorders such as stiff person syndrome, specific pain conditions such as burning mouth syndrome, catatonia and status dystonicus.
References:
- Pelzer, A., Van der Heijden, F., & Den Boer, E. (2018). Systematic review of catatonia treatment. Neuropsychiatric Disease and Treatment, 14, 317-326.
- Wright, S. L. (2020). Limited utility for benzodiazepines in chronic pain management: A narrative review. Advances in Therapy, 37(6), 2604-2619.
Slide 4 of 19
They are used for REM sleep behavior disorder as well as an end-of-life palliative care.
References:
- Durán-Crane, A., Laserna, A., López-Olivo, M. A., Cuenca, J. A., Díaz, D. P., Cardenas, Y. R., Urso, C., O’Connell, K., Azimpoor, K., Fowler, C., Price, K. J., Sprung, C. L., & Nates, J. L. (2019). Clinical practice guidelines and consensus statements about pain management in critically ill end-of-life patients: A systematic review. Critical Care Medicine, 47(11), 1619-1626.
- Howell, M., Avidan, A. Y., Foldvary-Schaefer, N., Malkani, R. G., During, E. H., Roland, J. P., McCarter, S. J., Zak, R. S., Carandang, G., Kazmi, U., & Ramar, K. (2023). Management of REM sleep behavior disorder: An American Academy of Sleep Medicine systematic review, meta-analysis, and GRADE assessment. Journal of Clinical Sleep Medicine, 19(4), 769-810.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 19
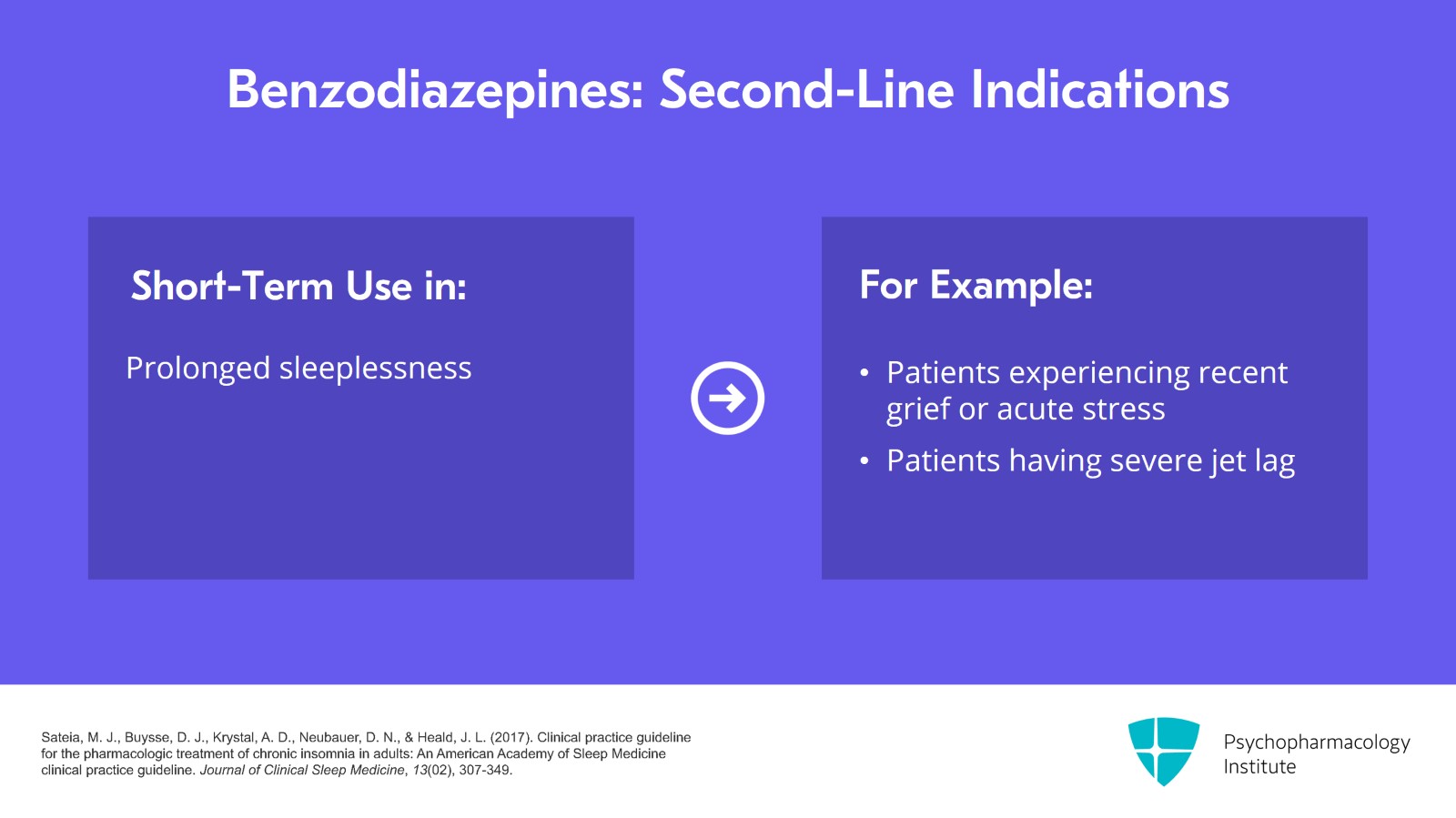
While those are the first-line indications for benzodiazepines, they are more often prescribed for some of their second-line usages.
So they are appropriate for short-term use which can be thought of as being around one to three days for prolonged sleeplessness which is not due to circadian rhythm or chronic sleep problem. Some examples of this would be if a patient has experienced recent grief or acute stress or is having severe jet lag, it’d be appropriate to prescribe a benzodiazepine to be used for a few days.
References:
- Sateia, M. J., Buysse, D. J., Krystal, A. D., Neubauer, D. N., & Heald, J. L. (2017). Clinical practice guideline for the pharmacologic treatment of chronic insomnia in adults: An American Academy of Sleep Medicine clinical practice guideline. Journal of Clinical Sleep Medicine, 13(02), 307-349.
Slide 6 of 19
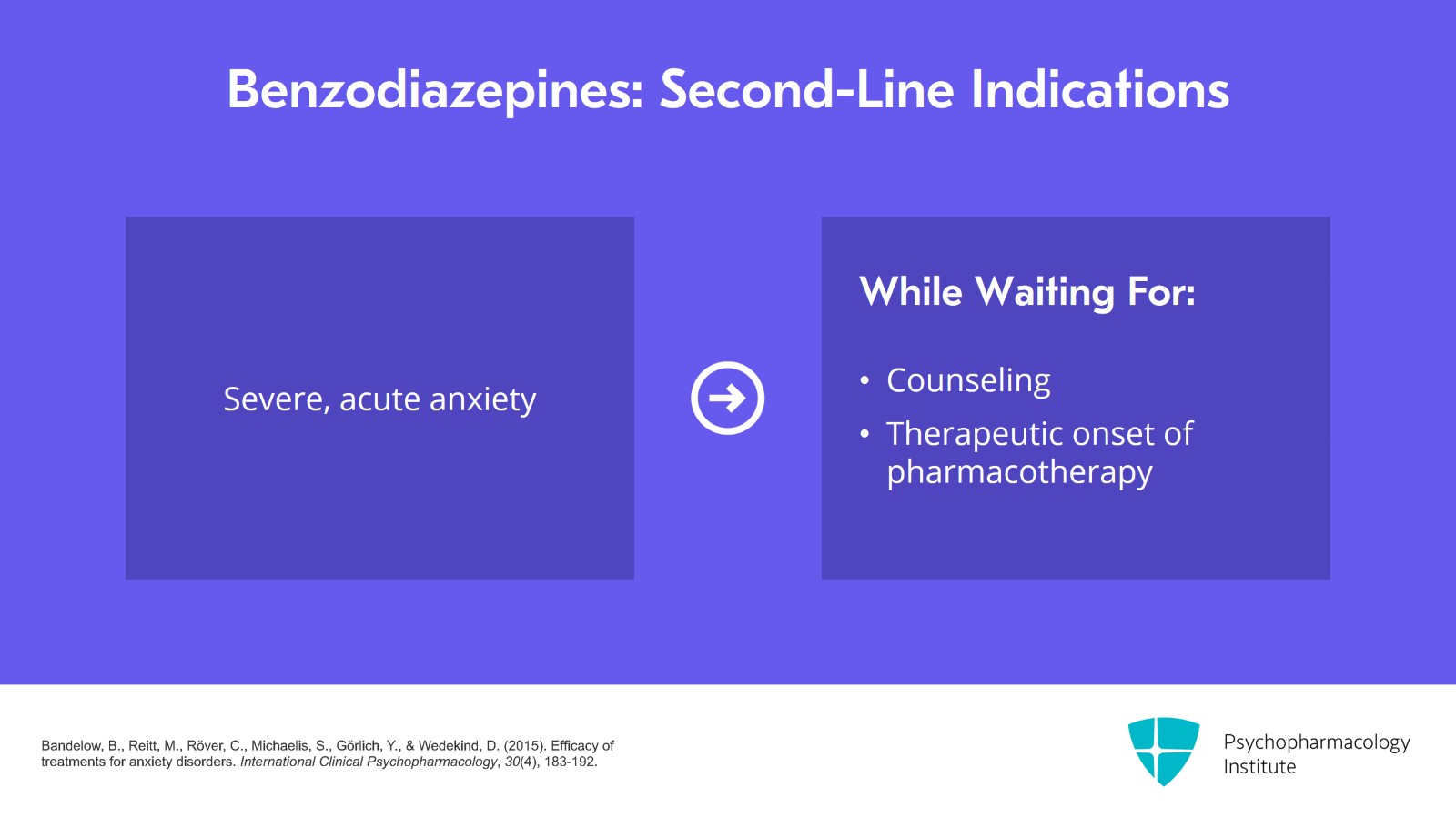
They’re also appropriate in the setting of severe and acute anxiety where no other appropriate support is immediately available while waiting for counseling or therapy support to be arranged as well as while waiting for therapeutic onset of other first-line pharmacotherapy for anxiety such as our antidepressants.
References:
- Bandelow, B., Reitt, M., Röver, C., Michaelis, S., Görlich, Y., & Wedekind, D. (2015). Efficacy of treatments for anxiety disorders. International Clinical Psychopharmacology, 30(4), 183-192.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 19
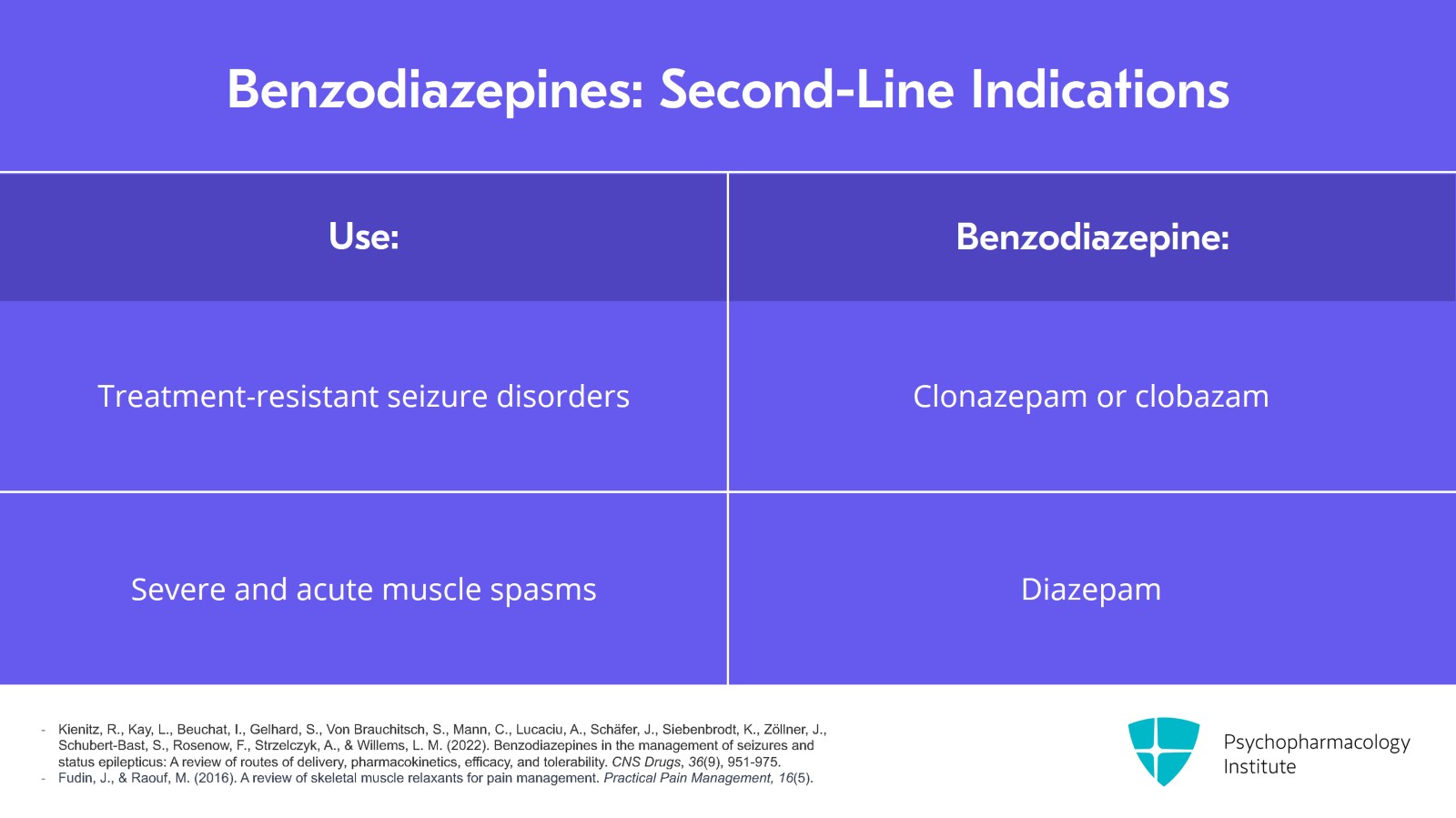
They can be used in certain treatment-resistant intractable seizure disorders and in this case, what is approved is clonazepam or clobazam.
And diazepam can be used for severe and acute muscle spasms that haven’t responded to the first-line treatments.
References:
- Kienitz, R., Kay, L., Beuchat, I., Gelhard, S., Von Brauchitsch, S., Mann, C., Lucaciu, A., Schäfer, J., Siebenbrodt, K., Zöllner, J., Schubert-Bast, S., Rosenow, F., Strzelczyk, A., & Willems, L. M. (2022). Benzodiazepines in the management of seizures and status epilepticus: A review of routes of delivery, pharmacokinetics, efficacy, and tolerability. CNS Drugs, 36(9), 951-975.
- Fudin, J., & Raouf, M. (2016). A review of skeletal muscle relaxants for pain management. Practical Pain Management, 16(5).
Slide 8 of 19
Of note, there is only very low quality evidence about using them in the setting of tardive dyskinesia and a 2018 Cochrane review determined that there were only a few small and poorly reported trials on the effect of benzodiazepines as an adjunctive treatment for antipsychotic-induced tardive dyskinesia.
They found that overall these inconclusive results meant routine clinical use is not indicated and that treatment using benzodiazepines for tardive dyskinesia remains experimental.
References:
- Bergman, H., Bhoopathi, P. S., & Soares-Weiser, K. (2018). Benzodiazepines for antipsychotic-induced tardive dyskinesia. Cochrane Database of Systematic Reviews, 2018(1).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 19
When thinking about selecting benzodiazepines, I would urge you to consider trying to avoid the use of alprazolam.
As we’ve learned more about its unique pharmacology, we know that it’s the shortest acting with a half-life of 6 to 12 hours. It’s very potent; 0.5 mg is equal to 5 to 10 mg of diazepam depending on an individual’s cross-tolerance.
References:
- Mamtani, H., & Chaturvedi, S. K. (2023). Alprazolam: Good for some, not good for all!. Journal of Clinical Psychopharmacology, 43(3), 204–208.
- Ait-Daoud, N., Hamby, A. S., Sharma, S., & Blevins, D. (2018). A review of Alprazolam use, misuse, and withdrawal. Journal of Addiction Medicine, 12(1), 4-10.
Slide 10 of 19
There’s also increased risk of tolerance and interdose withdrawal and rebound symptoms because of how short acting alprazolam is and it is more toxic in overdose especially when combined with other substances such as opioids. It is also more reinforcing and therefore has a higher risk of misuse and addiction than the other benzodiazepines.
References:
- Mamtani, H., & Chaturvedi, S. K. (2023). Alprazolam: Good for some, not good for all! Journal of Clinical Psychopharmacology, 43(3), 204–208.
- Ait-Daoud, N., Hamby, A. S., Sharma, S., & Blevins, D. (2018). A review of alprazolam use, misuse, and withdrawal. Journal of Addiction Medicine, 12(1), 4-10.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 19
The reason that alprazolam is more reinforcing and therefore has a greater risk of misuse and addiction is because it causes a significant increase in extracellular dopamine in the striatum and this is, therefore, more reinforcing and more likely to lead to misuse and addiction.
This increase in the extracellular dopamine is not seen with lorazepam. When I need to use a shorter-acting benzodiazepine, I will preferentially choose lorazepam over alprazolam for the above reasons.
References:
- Mamtani, H., & Chaturvedi, S. K. (2023). Alprazolam: Good for some, not good for all! Journal of Clinical Psychopharmacology, 43(3), 204–208.
- Ait-Daoud, N., Hamby, A. S., Sharma, S., & Blevins, D. (2018). A review of Alprazolam use, misuse, and withdrawal. Journal of Addiction Medicine, 12(1), 4-10.
Slide 12 of 19
I would also urge caution with the use of clonazepam.
Similar to alprazolam, it is more potent and 0.5 mg is equivalent to approximately 5 to 10 mg of diazepam. One of the bigger limitations I come up against is when someone has been on clonazepam chronically and we’re tapering, your taper becomes limited by the dosages that it is available in unless you start to use other methods or compounding pharmacy.
So the smallest dose that the regular-sized tab comes in is 0.5 mg in the US and it does come in a 0.25 mg and 0.125 mg oral disintegrating tab. However, it’s variable whether insurance covers this and it can be difficult to cut it in much more than half because it becomes crumbly.
References:
- Ashton, C. H. (2002). Benzodiazepines: How They Work and How to Withdraw (The Ashton Manual). Retrieved January 5, 2024, from http://www.benzo.org.uk/manual/
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 19
We’ve also seen that for many withdrawal from these more higher potency benzodiazepines is more difficult.
The higher potency benzodiazepines are also the ones most commonly prescribed – alprazolam, clonazepam and lorazepam.
References:
- Mamtani, H., & Chaturvedi, S. K. (2023). Alprazolam: Good for some, not good for all!. Journal of Clinical Psychopharmacology, 43(3), 204–208.
- Ait-Daoud, N., Hamby, A. S., Sharma, S., & Blevins, D. (2018). A review of Alprazolam use, misuse, and withdrawal. Journal of Addiction Medicine, 12(1), 4-10.
Slide 14 of 19
When thinking about the efficacy of benzodiazepines, for anxiety disorders, benzodiazepines were superior to placebo in reducing short-term anxiety symptoms which is certainly not a surprise to most of us. However, we should keep in mind that less than two-thirds of patients experience full remission of their symptoms with this treatment. And so, like many of our other treatments, it requires a multimodal approach. Additionally, anxiety often returns when treatment is discontinued and sometimes is worse because of withdrawal or between-dose withdrawal.
References:
- Ashton, C. H. (2002). Benzodiazepines: How They Work and How to Withdraw (The Ashton Manual). Retrieved January 5, 2024, from http://www.benzo.org.uk/manual/
- Barlow, D. H. (2002). Anxiety and its disorders: The nature and treatment of anxiety and panic (2nd ed.). The Guilford Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 19
For insomnia, it’s been found that benzodiazepines can help induce sleep in about 50% of patients; however, this therapeutic benefit is often short lived, about one to two weeks. After that time, it may be hard to tell whether a patient is getting the benefit of sleep from the medication or whether if they don’t take the medication and can’t sleep it’s because they’re experiencing rebound from withdrawing the medication.
References:
- Ashton, C. H. (2002). Benzodiazepines: How They Work and How to Withdraw (The Ashton Manual). Retrieved January 5, 2024, from http://www.benzo.org.uk/manual/
- Barlow, D. H. (2002). Anxiety and its disorders: The nature and treatment of anxiety and panic (2nd ed.). The Guilford Press.
Slide 16 of 19
Additionally, it’s important that we and our patients understand that benzodiazepines reduce the amount of time that is spent in restorative stage 3 and 4 sleep and also reduce REM sleep. This is similar to the effects of alcohol on sleep.
References:
- Ashton, C. H. (2002). Benzodiazepines: How They Work and How to Withdraw (The Ashton Manual). Retrieved January 5, 2024, from http://www.benzo.org.uk/manual/
- Barlow, D. H. (2002). Anxiety and its disorders: The nature and treatment of anxiety and panic (2nd ed.). The Guilford Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 19
So to review the key points for this video, benzodiazepines have several first-line indications for use including the treatment of alcohol and benzodiazepine withdrawal, acute crisis anxiety without psychosis, acute movement disorders including catatonia, REM sleep behavior disorder, status epilepticus and procedural anesthesia.
Second-line indications include acute insomnia as well as severe and acute anxiety.
Slide 18 of 19
Finally, it’s important we always use the lowest effective dose for the shortest duration and that we educate patients that over time, if they take this on a regular basis, they will likely experience decreased efficacy as they develop tolerance to many of the common effects.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.