Slides and Transcript
Slide 1 of 22
We're now turning to the section of the talk that's going to be about specific medications and their use during breastfeeding. I'm going to divide this up into sections on different classes of medications and I'll work in some clinical vignettes for most of these types of drugs so that you can see how to apply these principles to your patients.
Slide 2 of 22
Remember that older drugs have more evidence. So, if you're starting from scratch and you want to use a drug for the first time, choose something that's older because it will have more evidence. For the SSRIs, for example, this means that the older SSRIs are drugs for which we've collected a lot of evidence. Those new drugs that have come out in the last few years, we don't know anything about their use in breastfeeding. Chances are they're fine, but we don't actually have any data.
References:
- Begg, E. J., Duffull, S. B., Hackett, L. P., & Ilett, K. F. (2002). Studying drugs in human milk: Time to unify the approach. Journal of Human Lactation, 18(4), 323-332.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 22
We have no evidence also that timing of the drug dose relative to timing of feedings makes any difference. So, I think a lot of doctors will give advice that "well, you should feed the baby and then take your sertraline." But we don't actually have any evidence that that makes a difference so I wouldn't advise women that way.
References:
- Begg, E. J., Duffull, S. B., Hackett, L. P., & Ilett, K. F. (2002). Studying drugs in human milk: Time to unify the approach. Journal of Human Lactation, 18(4), 323-332.
Slide 4 of 22
Fortunately, the SSRI medications all have low passage into the breastmilk, and they're all considered compatible with breastfeeding.
References:
- Begg, E. J., Duffull, S. B., Hackett, L. P., & Ilett, K. F. (2002). Studying drugs in human milk: Time to unify the approach. Journal of Human Lactation, 18(4), 323-332.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 22
One thing to be aware of is poor neonatal adaptation syndrome which may occur in up to 30% of babies who are exposed to SSRIs in utero. This is a behavioral syndrome that usually goes away by about two weeks postpartum, and it's characterized by fussiness, difficulty feeding and other behavioral symptoms in the postpartum.
References:
- Begg, E. J., Duffull, S. B., Hackett, L. P., & Ilett, K. F. (2002). Studying drugs in human milk: Time to unify the approach. Journal of Human Lactation, 18(4), 323-332.
Slide 6 of 22
We don't really know what it is whether it's withdrawal, toxicity or something else because it's also observed in babies whose mothers did not take SSRIs in utero. But there's some evidence that it may be lessened in breastfed babies. So that's actually one advantage to a woman who used the medication in pregnancy staying on that medication in breastfeeding.
References:
- Begg, E. J., Duffull, S. B., Hackett, L. P., & Ilett, K. F. (2002). Studying drugs in human milk: Time to unify the approach. Journal of Human Lactation, 18(4), 323-332.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 22
Sertraline is the drug that's probably best studied in breastfeeding and has the lowest passage into breastmilk. So, it's often a go-to for women who are starting a drug for the first time in the postpartum.
References:
- Drugs and lactation database: (LactMed). (2006). National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK501922/?report=reader
- Begg, E. J., Duffull, S. B., Hackett, L. P., & Ilett, K. F. (2002). Studying drugs in human milk: Time to unify the approach. Journal of Human Lactation, 18(4), 323-332.
Slide 8 of 22
Fluoxetine has a very long half-life which at first led to theoretical concerns about increased adverse effects for infants. And in fact, there are more case reports of sedation and colic for fluoxetine than for other SSRI medications. That may mean that it wouldn't be your first choice for a mother who is SSRI naïve and needs to go on medication for the first tine in the postpartum.
References:
- Drugs and lactation database: (LactMed). (2006). National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK501922/?report=reader
- Begg, E. J., Duffull, S. B., Hackett, L. P., & Ilett, K. F. (2002). Studying drugs in human milk: Time to unify the approach. Journal of Human Lactation, 18(4), 323-332.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 22
It doesn't mean, however, that it should be stopped in mothers who are already using it. We know that certain people respond to certain antidepressants, and we can't figure out why. So, if you have a mother who's has had a good response with fluoxetine in the past, I wouldn't use that theoretical concern about increased effects in the infant as a reason not to use fluoxetine. I'd try it and observe.
References:
- Drugs and lactation database: (LactMed). (2006). National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK501922/?report=reader
- Begg, E. J., Duffull, S. B., Hackett, L. P., & Ilett, K. F. (2002). Studying drugs in human milk: Time to unify the approach. Journal of Human Lactation, 18(4), 323-332.
Slide 10 of 22
What about things other than SSRIs? Well, we use them less often in the perinatal period simply because side effects of other classes of antidepressants tend to be higher, but we don't actually have any known contraindications for these medications in breastfeeding.
References:
- Begg, E. J., Duffull, S. B., Hackett, L. P., & Ilett, K. F. (2002). Studying drugs in human milk: Time to unify the approach. Journal of Human Lactation, 18(4), 323-332.
- Drugs and lactation database: (LactMed). (2006). National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK501922/?report=reader
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 22
The tricyclic antidepressants have all been studied and there's no evidence of excess adverse effects with this class. There are, however, more cases of hypotonia, poor suckling and vomiting with doxepin as opposed to some of the other TCAs.
References:
- Begg, E. J., Duffull, S. B., Hackett, L. P., & Ilett, K. F. (2002). Studying drugs in human milk: Time to unify the approach. Journal of Human Lactation, 18(4), 323-332.
- Drugs and lactation database: (LactMed). (2006). National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK501922/?report=reader
Slide 12 of 22
For bupropion which is used frequently in women of childbearing age, there's a theoretical concern that it could lower the seizure threshold when used in high doses. And in fact, we have one published case report of an infant who had a seizure but it's only one published case report. What that leads you to do in the clinical situation is use this drug with caution in a baby who has other reasons for being at risk for seizure but it's not a reason not to use the drug in babies who don't have an excess seizure risk.
References:
- Begg, E. J., Duffull, S. B., Hackett, L. P., & Ilett, K. F. (2002). Studying drugs in human milk: Time to unify the approach. Journal of Human Lactation, 18(4), 323-332.
- Drugs and lactation database: (LactMed). (2006). National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK501922/?report=reader
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 22
We have limited information on mirtazapine. So, it's a newer drug that we don't have as much as information on but the information we have gives no evidence of adverse effects. And as I mentioned before, among the SSRIs, those newer drugs, we just simply don't have any evidence so I would stick to the older drugs when possible.
References:
- Begg, E. J., Duffull, S. B., Hackett, L. P., & Ilett, K. F. (2002). Studying drugs in human milk: Time to unify the approach. Journal of Human Lactation, 18(4), 323-332.
- Drugs and lactation database: (LactMed). (2006). National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK501922/?report=reader
Slide 14 of 22
Let's talk about how to apply this to a particular patient. Our patient today is Mary Jones. She's 34 years old and she is three weeks postpartum with her first child.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 22
She was referred by her obstetrician for two weeks of difficulty sleeping, worries about the baby and her health, poor appetite and concentration. She feels her baby might be better off without her.
Slide 16 of 22
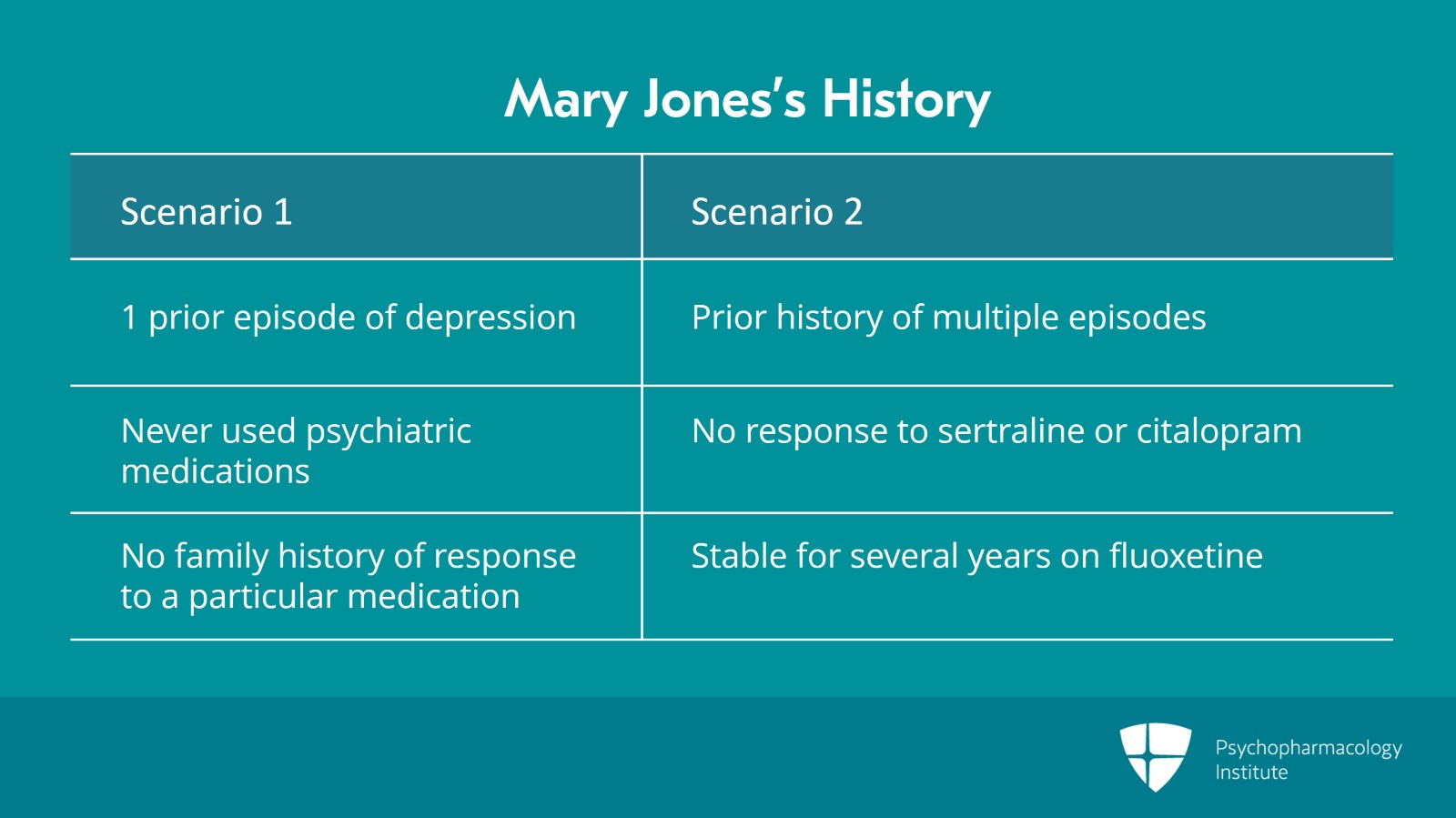
Prior history, let's imagine two different scenarios because they're going to affect what drug we choose. First scenario, this patient has had one prior episode of depression that resolved without treatment. She's never used psychiatric medication. She's got no family history of medication response to a particular medication. Scenario number 2, we're going to give her a prior history of multiple episodes with severe symptoms. She is not responding to sertraline or citalopram in the past, but she was stable for several years on fluoxetine.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 22
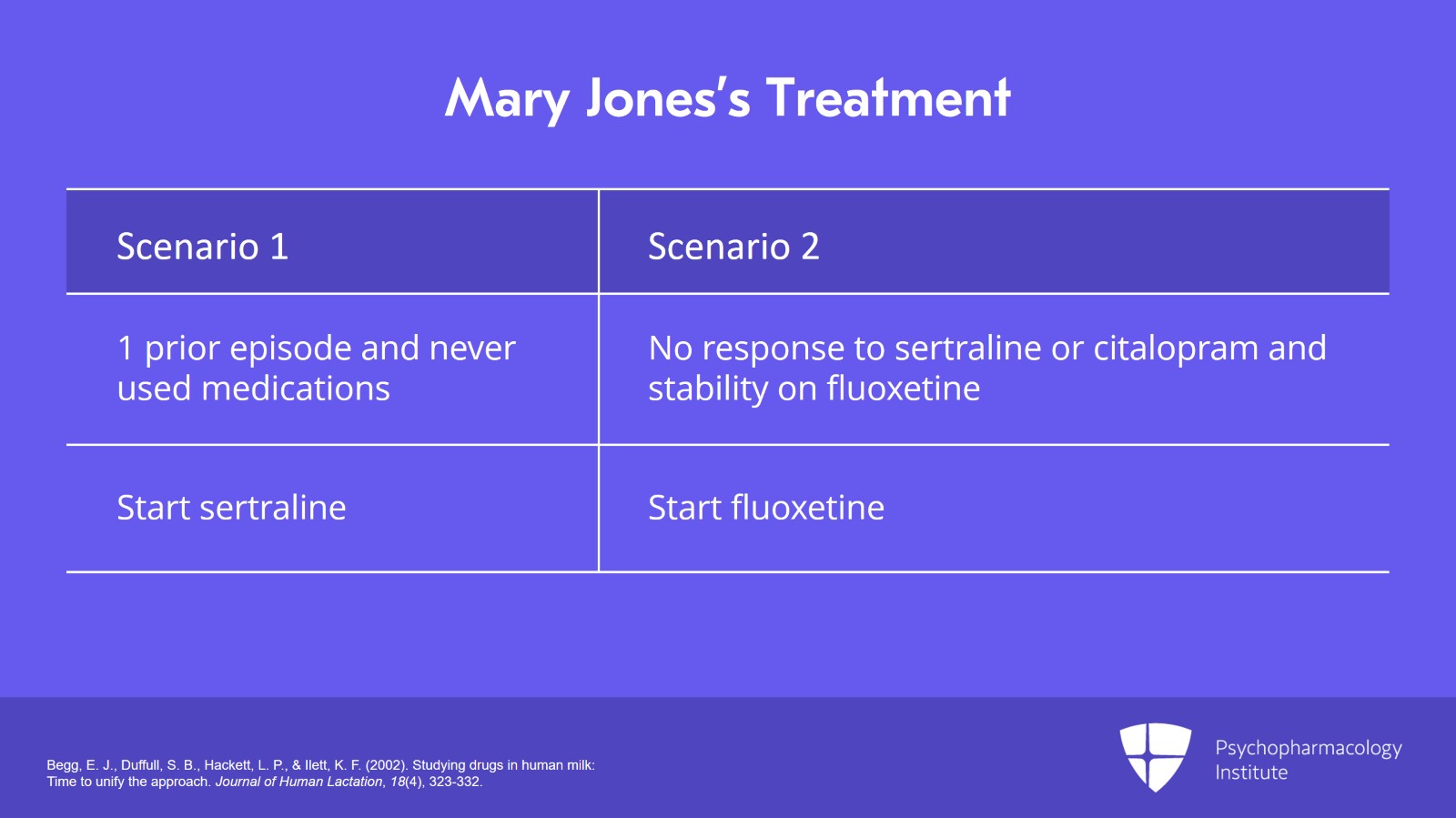
So, let's say for either of these two scenarios, Mary's baby was born full term, healthy weight with no complications and no medical comorbidities. There's no reason to calculate the relative infant dose here. We're looking at commonly used drugs with a lot of published literature about the milk-to-plasma ratio and nothing about the baby that makes me think this is an unusual situation. Symptoms are straightforward.
Slide 18 of 22
In scenario number 1 where she had one prior episode and never used medications, we'll choose to start the patient on sertraline. It has the best evidence of the lowest passage into the breastmilk, and we'll titrate it up to the therapeutic dose. In scenario number 2, however, where the patient had previously not responded to sertraline or citalopram but had several years of stability on fluoxetine, we would instead start the patient on fluoxetine. Remember there's a theoretical risk of increased adverse reactions due to long half-life but a good history that this works well for the patient.
References:
- Begg, E. J., Duffull, S. B., Hackett, L. P., & Ilett, K. F. (2002). Studying drugs in human milk: Time to unify the approach. Journal of Human Lactation, 18(4), 323-332.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 22
So, we'd try fluoxetine. We'd advise her to monitor the patient for drowsiness. We'd contact the pediatrician to explain our reasoning and we'd watch carefully. We can always switch to something else if there's an adverse reaction, but we know this medication will work best for the mother.
References:
- Begg, E. J., Duffull, S. B., Hackett, L. P., & Ilett, K. F. (2002). Studying drugs in human milk: Time to unify the approach. Journal of Human Lactation, 18(4), 323-332.
Slide 20 of 22
So, what are the key points of this section? SSRI medications in general have low passage into the breastmilk and all of them are considered compatible with breastfeeding. Fluoxetine has a longer half-life which led to early anecdotal concern about increased half-life and increased case reports early on about adverse reactions but that doesn't mean there's reason to stop it for breastfeeding if it's the medication that works well for the patient. Remember that older drugs have more data.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 21 of 22
Sertraline has evidence of the lowest passage into the breastmilk but again choose the drug that works for the patient. And other classes of antidepressants are also considered compatible with breastfeeding.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.