Slides and Transcript
Slide 2 of 13
Psychodynamic Psychopharmacology is an approach developed at the Austen Riggs Center for working with patients that have demonstrated a degree of treatment resistance and, in line with what we've already been talking about, it's an approach that explicitly acknowledges and addresses the central role of meaning and interpersonal factors in pharmacotherapy. It recognizes that medications bear potent meanings and that these should be explored in the treatment of treatment-resistant patients, not just by therapists but also by their pharmacotherapists.
References:
- Mintz, D. (2022). Psychodynamic Psychopharmacology: Caring for the Treatment-Resistant Patient. American Psychiatric Pub.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 13
Psychodynamic psychopharmacology doesn't replace, it complements a traditional objective–descriptive approach to psychopharmacology. So, a traditional objective–descriptive approach typically is based in population-level studies that try to figure out how people are similar and to identify which group of people would respond, for example, to a certain medication but, of course, so many of our patients don't respond the way the studies show they should.
References:
- Mintz, D. (2022). Psychodynamic Psychopharmacology: Caring for the Treatment-Resistant Patient. American Psychiatric Pub.
Slide 4 of 13
And so, psychodynamic psychopharmacology, complimenting that traditional objective–descriptive focus, makes an effort to consider what is unique about this patient. What is it about this patient and their psychology that makes the medications not work the way we expect them to or hope them to? And in that sense, the psychodynamic psychopharmacology gives us guidance not about what to prescribe, which is what comes from that other evidence base, but gives us guidance about how to prescribe to help the patient get the most out of the treatments that we're giving them. Psychodynamic psychopharmacology also is a way of using everyday psychodynamic techniques to explore the meaning of medication and explore resistances to the healthy use of medications in ways that promote better outcomes.
References:
- Mintz, D. (2022). Psychodynamic Psychopharmacology: Caring for the Treatment-Resistant Patient. American Psychiatric Pub.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 13
But also, I think there are probably many of us that have gone into psychiatry because we're interested in people, we're interested in the human mind, we're interested in what makes people tick. And then, we end up operating in a world where there's tremendous need and great pressures for us to work in a primarily pharmacologic mode. But I think that psychodynamic psychopharmacology offers a potential to integrate psychotherapeutic understandings and skills into our everyday work in ways that make the doctor-patient engagement not just more meaningful for our patients, but also more meaningful for ourselves and contribute as a kind of an antidote to the burnout that we can face in our work.
References:
- Mintz, D. (2022). Psychodynamic Psychopharmacology: Caring for the Treatment-Resistant Patient. American Psychiatric Pub.
Slide 6 of 13
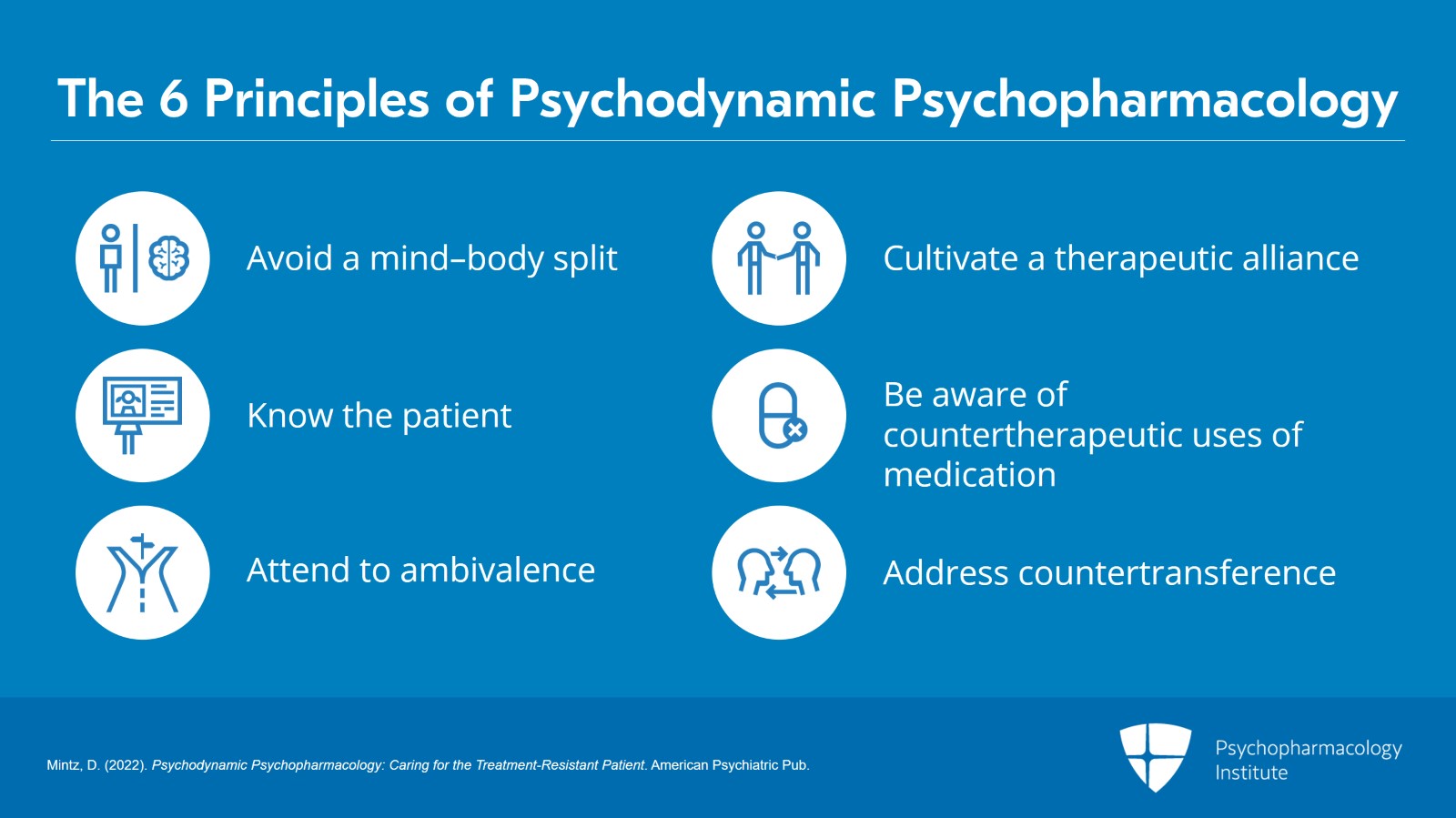
Psychodynamic psychopharmacology has six technical principles that I want to mention. These are: avoiding a mind–body split in the ways we work with our patients, knowing who the patient is, attending to the patient's ambivalence about symptoms, cultivating a therapeutic alliance and addressing negative transference, being aware of counter-therapeutic uses of medications or treat resistance from medications, and addressing countertransference issues and countertransference and enactments in prescribing.
References:
- Mintz, D. (2022). Psychodynamic Psychopharmacology: Caring for the Treatment-Resistant Patient. American Psychiatric Pub.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 13
So, in a sense, it's a way of recognizing that psychodynamics are absolutely an aspect of pharmacotherapy. This includes the recognition: that there's an unconscious that affects how patients use medications; that our patients are in conflict, they're ambivalent about medications, about caregiving, in ways that interfere with the ways they use medications; that they bring transferences into the work. Those transferences stir up counter-transferences in us so that there's a level of irrationality that's always at play in the pharmacotherapeutic relationship.
References:
- Jensen, K. B., Kaptchuk, T. J., Kirsch, I., Raicek, J., Lindstrom, K. M., Berna, C., Gollub, R. L., Ingvar, M., & Kong, J. (2012). Nonconscious activation of placebo and nocebo pain responses. Proceedings of the National Academy of Sciences, 109(39), 15959-15964.
Slide 8 of 13
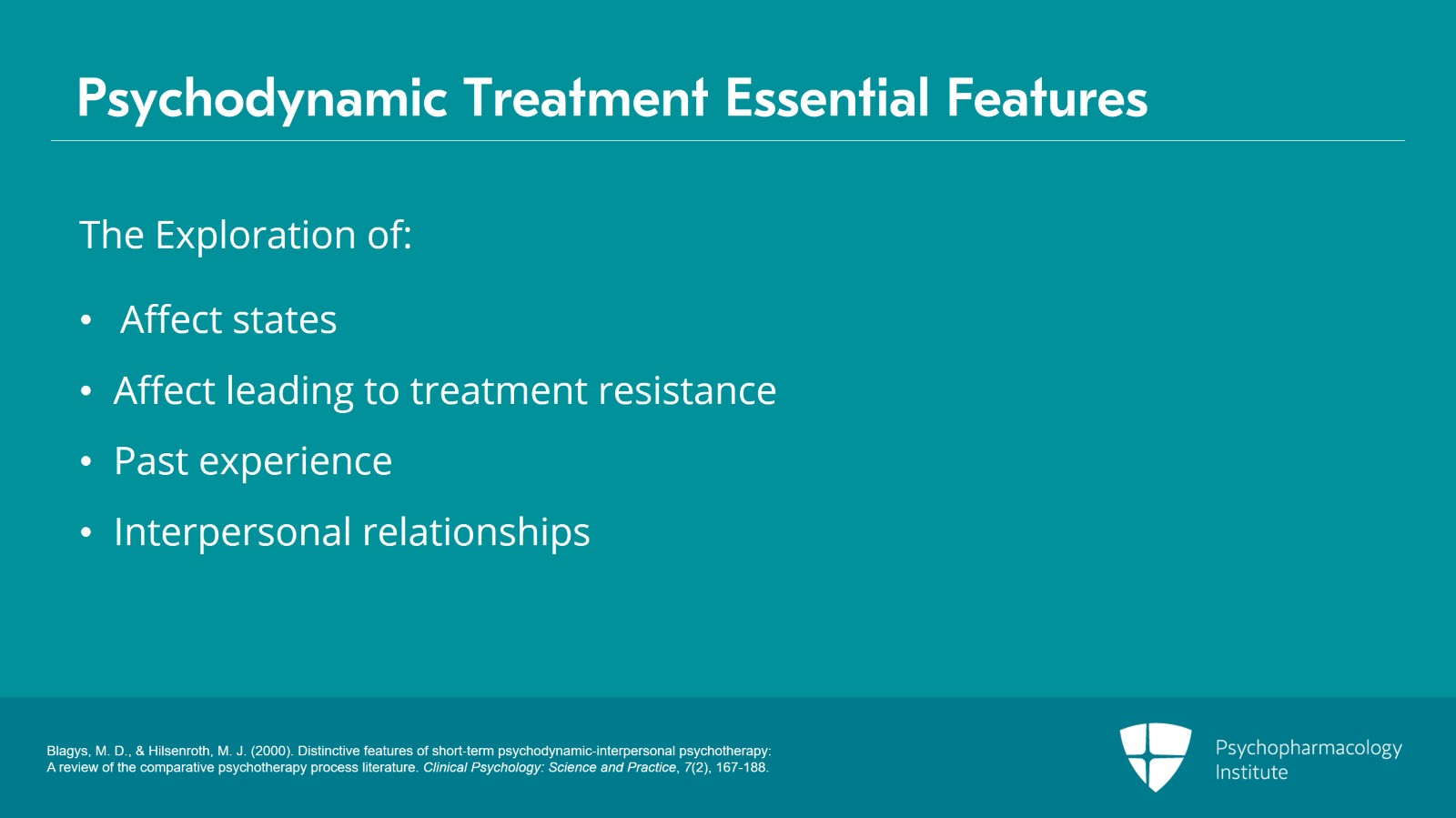
As I said in the last lecture, we integrate the kinds of things that Blagys and Hilsenroth and their evidence-based study of psychodynamic treatment identified as essential features of psychodynamic treatment. So: a focus on affect states and emotional expression, exploration and avoidance of affect leading to treatment resistance, identification of patterns and thoughts, feelings, and relationships on an emphasis on past experience, and ways that inform how the patient's going to use treatment in the here and now, focus on interpersonal relationships, and in this case, we can think of a very personal relationship oftentimes to medications.
References:
- Blagys, M. D., & Hilsenroth, M. J. (2000). Distinctive features of short‐term psychodynamic‐interpersonal psychotherapy: A review of the comparative psychotherapy process literature. Clinical Psychology: Science and Practice, 7(2), 167-188.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 13
And so, that's one of the things we want to understand: is the patient's relationship to medication itself an emphasis on the current doctor-patient relationship? And how we're working together, and an exploration of meaning in terms of patient's wishes and fantasies as pertains to pharmacotherapy. And all of these types of interventions, as I said, can be adapted and used in routine pharmacotherapy in ways that do not encroach on the psychotherapist and which form the backbone of psychodynamic psychopharmacology.
References:
- Blagys, M. D., & Hilsenroth, M. J. (2000). Distinctive features of short‐term psychodynamic‐interpersonal psychotherapy: A review of the comparative psychotherapy process literature. Clinical Psychology: Science and Practice, 7(2), 167-188.
Slide 10 of 13
Treatment resistance may develop when patients take normally effective medications and use them in ways that actually interfere with their development or healthy adaptive capacities and, for example, when they use medications and ways to bolster unhealthy defenses or interfere with healthy development. We, as prescribers, may also inadvertently contribute to the phenomenon of treatment resistance in the ways that we talk about medications or prescribe the medications or miss important resistances that are at play and, based on all these understandings, we're going to describe some specific techniques for addressing those dynamics in order to promote better outcomes.
References:
- Jensen, K. B., Kaptchuk, T. J., Kirsch, I., Raicek, J., Lindstrom, K. M., Berna, C., Gollub, R. L., Ingvar, M., & Kong, J. (2012). Nonconscious activation of placebo and nocebo pain responses. Proceedings of the National Academy of Sciences, 109(39), 15959-15964.
- Mintz, D. L., & Flynn, D. F. (2012). How (not what) to prescribe: nonpharmacologic aspects of psychopharmacology. Psychiatric Clinics, 35(1), 143-163.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 13
Psychological and psychosocial factors in many cases make all the difference between pharmacologic treatments that work and those that don’t. Common dynamic mechanisms contribute to patients’ active though perhaps unconscious resistance against pharmacologic treatment. This includes those patients who are ambivalent about getting well, as well as those patients who mistrust, either consciously or unconsciously, treatment or treaters in ways that keep them from getting better.
References:
- Mintz, D. L., & Flynn, D. F. (2012). How (not what) to prescribe: nonpharmacologic aspects of psychopharmacology. Psychiatric Clinics, 35(1), 143-163.
Slide 12 of 13
So, the key points are: Psychodynamic psychopharmacology is an approach to pharmacologic treatment resistance that recognizes that psychological and interpersonal factors can be key to positive pharmacologic outcomes in treatment-resistant patients. The psychodynamic factors such as the unconscious and many others are all operating in pharmacotherapy as much as they're operating in psychotherapy and influencing how well the patient is able to use treatment. And basic psychodynamic techniques can be readily applied in pharmacotherapy, and I think it can be done without significant use of our time, just a slight shift in our focus.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.