Slides and Transcript
Slide 1 of 18
As far as the management of delirium in patients with cancer, we have to have an individual approach to each patient and each patient's needs.
Slide 2 of 18
Ideally, we would maximize our preventive efforts to minimize any patient's risk for developing delirium. About 50% of delirium episodes in patients with advanced cancer can still be reversible.
References:
- Lawlor, P. G., & Bush, S. H. (2015). Delirium in patients with cancer: assessment, impact, mechanisms and management. Nature Reviews Clinical Oncology, 12(2), 77-92.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 18
We want to distinguish between cases where the delirium is part of the terminal stage, where the goal is to control symptoms, for example, pain or shortness of breath. In those cases, the delirium may not actually be reversible and may be part of the course of dying.
References:
- Trzepacz, P., Breitbart, W., Franklin, J., Levenson, J., Martini, D. R., & Wang, P. (2010). Treatment of patients with delirium. Practice Guideline for The Treatment of Patients With Delirium. Trzepacz PT, cheir. American Psychiatric Association, APA Press.
Slide 4 of 18
However, if we have a patient who is not in the process of dying, they're not terminally ill, then certainly it makes sense to search for possible causes and reverse the etiology of a delirium if we can, because the first-line intervention and treatment is to identify and treat reversible precipitants, so those causes that led to the development of delirium.
References:
- Trzepacz, P., Breitbart, W., Franklin, J., Levenson, J., Martini, D. R., & Wang, P. (2010). Treatment of patients with delirium. Practice Guideline for The Treatment of Patients With Delirium. Trzepacz PT, cheir. American Psychiatric Association, APA Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 18
We want to be mindful of the interference of delirium with the assessment and management of pain. Patients who are confused, agitated, delirious, may not be able to tell us how much pain they're experiencing and we may have to look for other signs of patients being in pain. On the other hand, we also don't want to assume that patients are in pain and overtreat them with opiates that may worsen the patient's mental status.
References:
- Lawlor, P. G., & Bush, S. H. (2015). Delirium in patients with cancer: assessment, impact, mechanisms and management. Nature Reviews Clinical Oncology, 12(2), 77-92.
Slide 6 of 18
Non-pharmacological intervention is very, very important in preventing and managing delirium, such as making sure that the patient has appropriate oxygen delivery, that they're hydrated, that we correct the electrolytes, that their bowel and bladder function is appropriately attended to.
References:
- Lawlor, P. G., & Bush, S. H. (2015). Delirium in patients with cancer: assessment, impact, mechanisms and management. Nature Reviews Clinical Oncology, 12(2), 77-92.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 18
That they have their visual and hearing aids, that we reorient them frequently, that we modify their environment as much as we can, so we keep the room well lit during the day and we minimize the nighttime interruptions as much as we can, and also involving physical therapy and occupational therapy to mobilize the patient. So, sitting up in bed or chair is better than just constantly lying down. Whatever we can get the patient to do is important to do so.
References:
- Lawlor, P. G., & Bush, S. H. (2015). Delirium in patients with cancer: assessment, impact, mechanisms and management. Nature Reviews Clinical Oncology, 12(2), 77-92.
Slide 8 of 18
Our pharmacy colleagues can help us identify and eliminate any drugs that could be contributing to delirium, for example opioids, benzodiazepines, anticholinergic agents or some other drugs that may be the culprit. Patients can be individually sensitive to some of these drugs.
References:
- Overshott, R., Karim, S., & Burns, A. (2008). Cholinesterase inhibitors for delirium. Cochrane Database of Systematic Reviews, (1).
- Lawlor et al.: Occurrence, causes, and outcome of delirium in patients with advanced cancer: a prospective study. Arch Intern Med. March, 2000; 160(6):786-794
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 18
Whenever possible, we want to taper off or discontinue drugs that we think could be contributing to delirium. For example, benzodiazepines, that are sometimes used for management of agitation can worsen the presentation of delirium. If we suspect that the patient's delirium could be caused by opioids, it makes sense to rotate or switch opioid agents.
References:
- Lawlor, P. G., Gagnon, B., Mancini, I. L., Pereira, J. L., Hanson, J., Suarez-Almazor, M. E., & Bruera, E. D. (2000). Occurrence, causes, and outcome of delirium in patients with advanced cancer: a prospective study. Archives of Internal Medicine, 160(6), 786-794.
Slide 10 of 18
As far as pharmacological treatment, there are no FDA-approved medications specifically for treatment of delirium but we quite often use antipsychotic medications. The goal of using the medications is to help the patients be awake, alert, calm, comfortable, and still be able to communicate with family and staff.
References:
- Kamholz, B. (2010). Update on delirium: diagnosis, management, and pathophysiology. Psychiatric Annals, 40(1), 52-62.
- Overshott, R., Karim, S., & Burns, A. (2008). Cholinesterase inhibitors for delirium. Cochrane Database of Systematic Reviews, (1).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 18
Of course, there are cases of patients who are so extremely agitated and so confused that even the workup, like getting the patient through the brain MRI, or even head CT, or doing an LP if that's needed, is impossible because of their agitation. For those patients it may help to use more sedating agents to calm them down and allow this workup to be done.
References:
- Kamholz, B. (2010). Update on delirium: diagnosis, management, and pathophysiology. Psychiatric Annals, 40(1), 52-62.
Slide 12 of 18
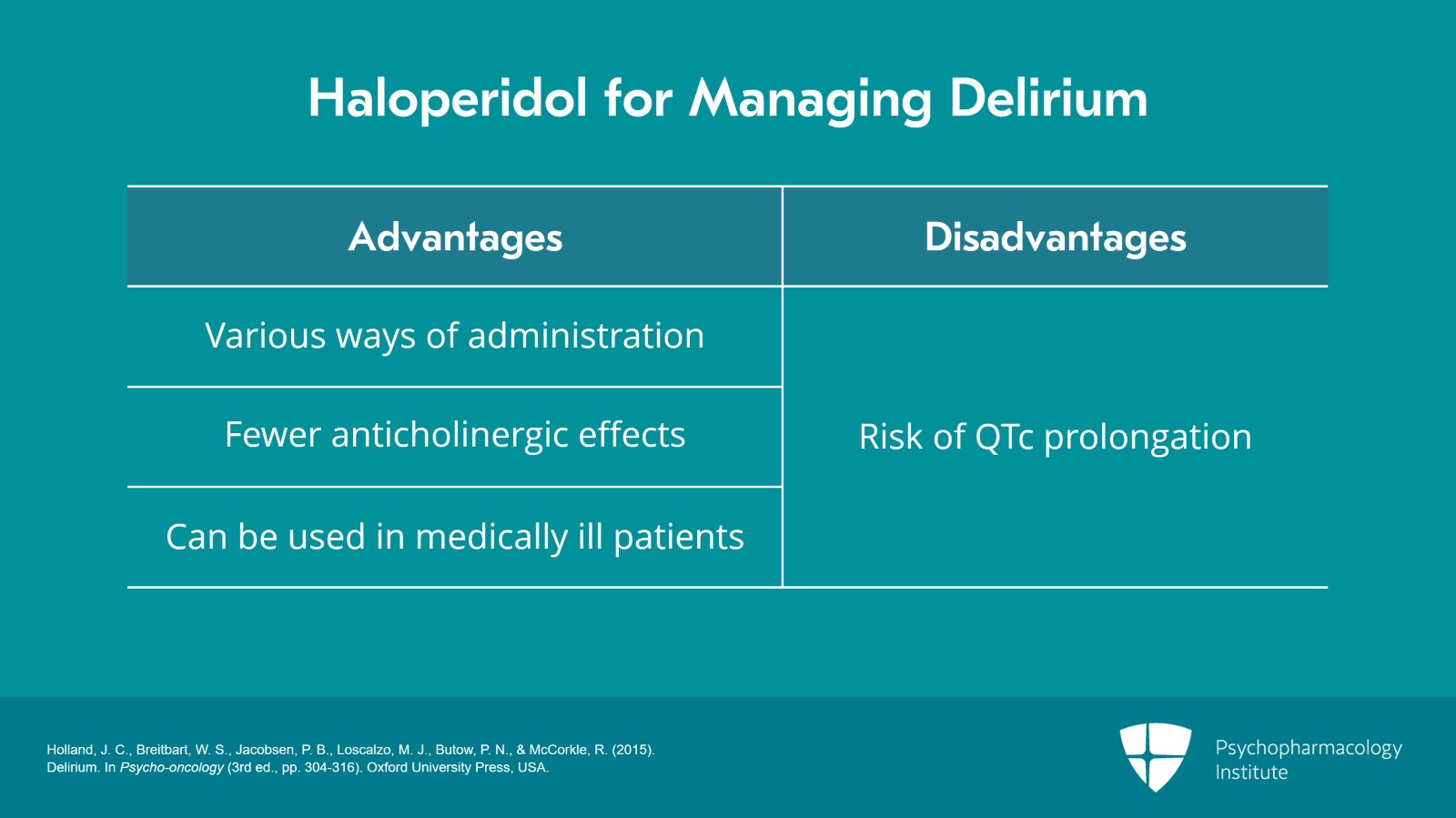
One of the most commonly, and probably historically, most commonly used antipsychotic is haloperidol, which has several advantages including various ways of administrations like p.o., subcutaneously, IV. Haloperidol has fewer anticholinergic effects, and does not have active metabolites, and can be safely used in medically ill patients. In our cancer patient population, we tend to avoid administering any medications via IM, intramuscularly, including antipsychotics, so that's not a common practice for us, but it is pretty common to use haloperidol via IV, in which case you want to make sure that you're monitoring the patient's cardiac function and especially the QTc interval, because there is a risk of QTc prolongation.
References:
- Holland, J. C., Breitbart, W. S., Jacobsen, P. B., Loscalzo, M. J., Butow, P. N., & McCorkle, R. (2015). Delirium. In Psycho-oncology (3rd ed., pp. 304-316). Oxford University Press, USA.12
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 18
As you may know, the FDA had issued a black box warning on all of antipsychotics when used in elderly and particularly in patients with dementia. They can increase risk of death in this patient population.
References:
- Meeks TW, Jeste DV. Beyond the Black Box: what is the role for antipsychotics in dementia? Curr Psychiatr. 2008 Jun 1;7(6):50-65.
Slide 14 of 18
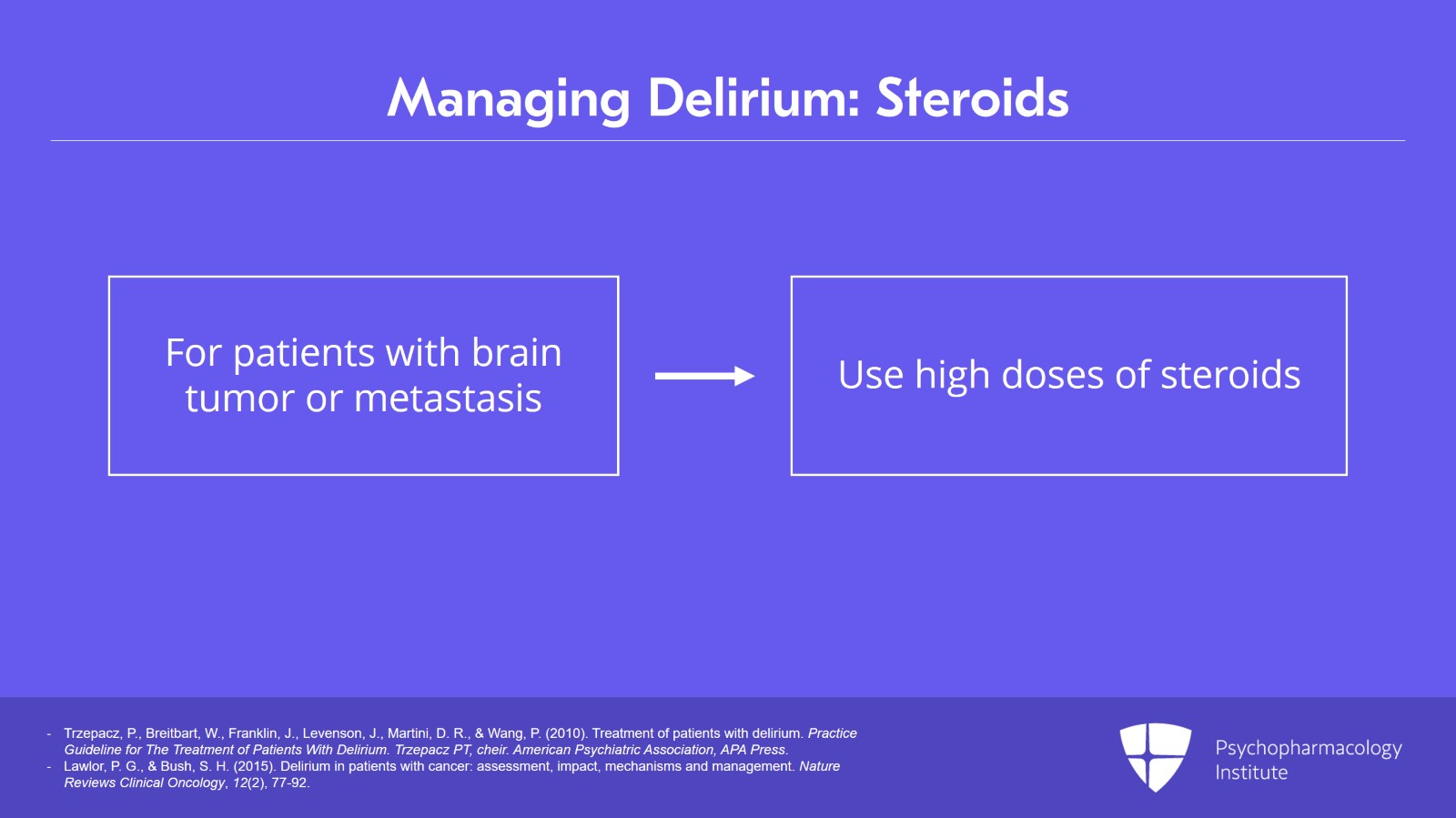
If the patient has a brain tumor or metastasis to their brain, high doses of steroids can help relieve those symptoms that could be due to surrounding edema.
References:
- Trzepacz, P., Breitbart, W., Franklin, J., Levenson, J., Martini, D. R., & Wang, P. (2010). Treatment of patients with delirium. Practice Guideline for The Treatment of Patients With Delirium. Trzepacz PT, cheir. American Psychiatric Association, APA Press.
- Lawlor, P. G., & Bush, S. H. (2015). Delirium in patients with cancer: assessment, impact, mechanisms and management. Nature Reviews Clinical Oncology, 12(2), 77-92.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 18
We generally recommend to avoid benzodiazepines and anticholinergic agents, with the caveat that benzodiazepines can actually have an important and helpful role in palliation of patients who are actively dying. So, for those patients we use benzodiazepines whenever that's appropriate and sometimes in combination with antipsychotic medications. Outside of that setting, benzodiazepines should be reserved for alcohol or sedative-hypnotics withdrawal management.
References:
- Pandharipande, P., Shintani, A., Peterson, J., Pun, B. T., Wilkinson, G. R., Dittus, R. S., … & Ely, E. W. (2006). Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. The Journal of the American Society of Anesthesiologists, 104(1), 21-26.
Slide 16 of 18
In summary: Non-pharmacologic interventions have both the preventive and treatment importance in managing delirium. Medications that can trigger or worsen delirium should be discontinued if at all possible.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 18
Benzodiazepines should be reserved for management of terminal delirium where antipsychotic agents are not sufficient for symptom control. Antipsychotic agents are used for symptomatic management especially in cases of highly hyperactive, agitated delirium, but they can also be useful in some of the hypoactive cases, particularly in patients who have hypoactive delirium but also are reporting hallucinations or anxiety.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.