Slides and Transcript
Slide 2 of 20
There are unique features of tic disorders. Specifically, tics are sudden, repetitive, stereotyped movements or sounds. Tics usually follow waxing and waning patterns in severity and frequency and involve a mixture of old and new tics. So it can sometimes be discouraging when you're seeing a patient and particularly to family or parents and they think this particular tic has gone away and then it comes back. And that's where it's important to reassure families that that's not a bad prognostic sign. That is in fact typical and very common in the course of the illness.
References:
- Murphy, T. K., Lewin, A. B., Storch, E. A., & Stock, S. (2013). Practice parameter for the assessment and treatment of children and adolescents with tic disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 52(12), 1341-1359.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 20
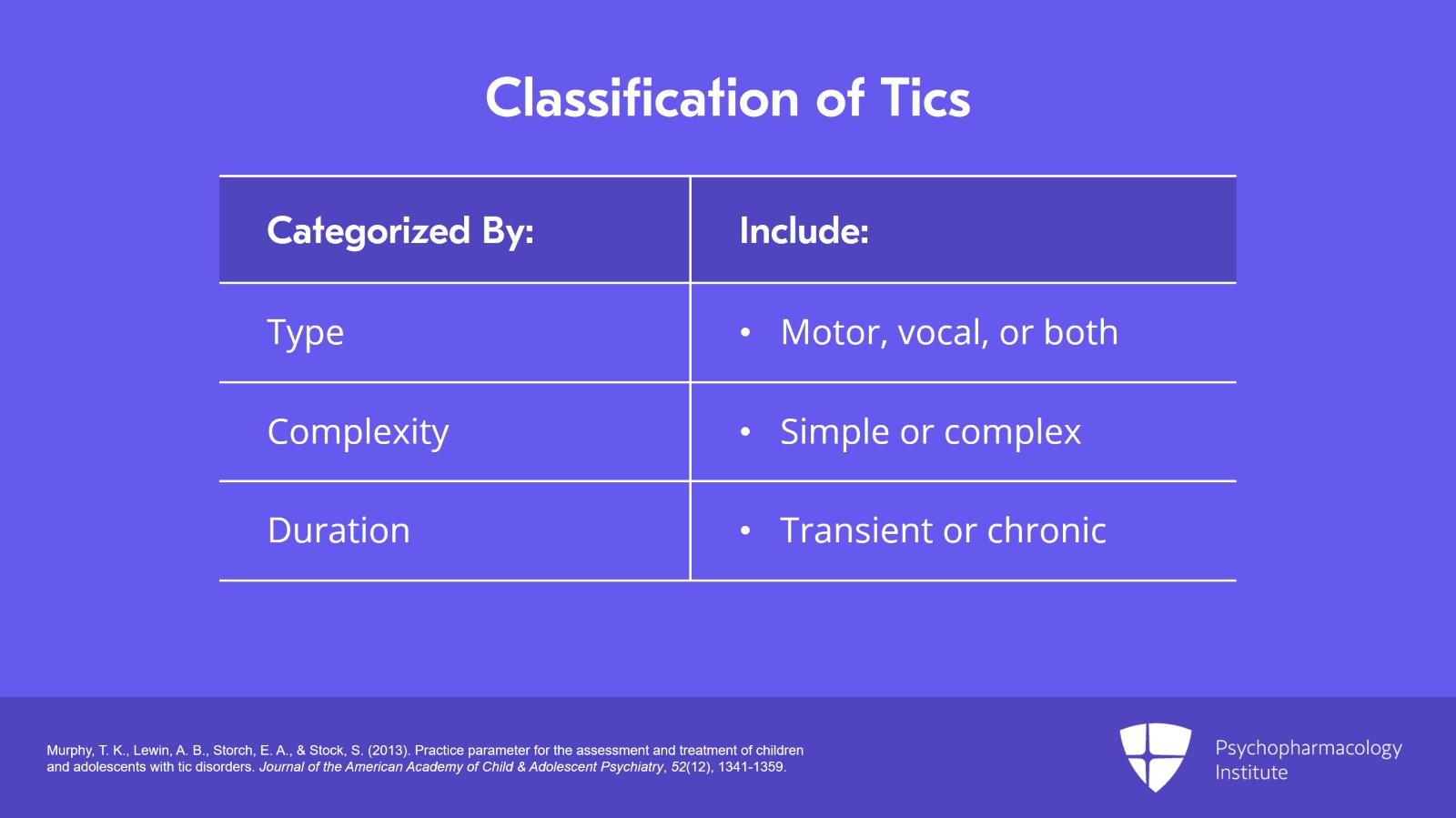
They're categorized by type (motor, vocal or both), their complexity, simple, rapid or meaningless; complex, those that are more purposeful, elaborate or orchestrated) and the duration can be transient, in some cases a duration of less than 12 consecutive months or they can be chronic with a duration of more than one year. And there are some excellent references from the Journal of the American Academy of Child and Adolescent Psychiatry. Murphy and colleagues wrote an excellent paper on this as did Ueda and Black in the Journal of Clinical Medicine in 2021.
References:
- Murphy, T. K., Lewin, A. B., Storch, E. A., & Stock, S. (2013). Practice parameter for the assessment and treatment of children and adolescents with tic disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 52(12), 1341-1359.
Slide 4 of 20
Psychological strains, any kind of stress, anxiety, excitement, anger, physical strains such as fatigue, sleep deprivation and infections, environmental changes can temporarily exacerbate tics.
References:
- Murphy, T. K., Lewin, A. B., Storch, E. A., & Stock, S. (2013). Practice parameter for the assessment and treatment of children and adolescents with tic disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 52(12), 1341-1359.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 20
And tic disorders are frequently associated with comorbid psychiatric disorders such as ADHD and OCD that can markedly impact functioning and become more problematic than tic symptoms. And this is especially important because comorbidity is frequent and it's the exception or at least less frequent not to have comorbidity. And when tic disorders are associated with comorbid conditions, that can make the prognosis more challenging.
References:
- Murphy, T. K., Lewin, A. B., Storch, E. A., & Stock, S. (2013). Practice parameter for the assessment and treatment of children and adolescents with tic disorders. Journal of the American Academy of Child & Adolescent Psychiatry, 52(12), 1341-1359.
Slide 6 of 20
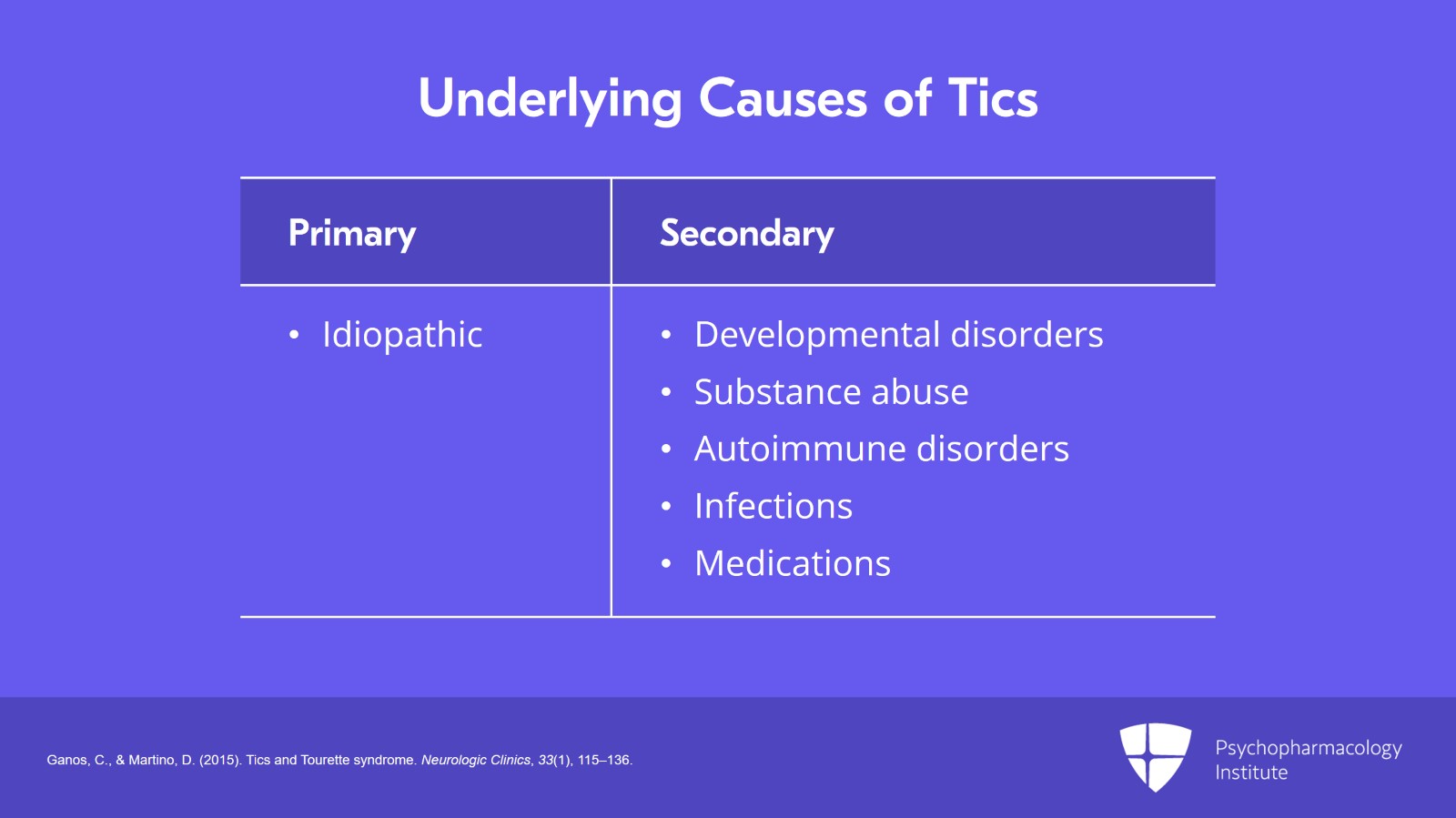
Underlying causes of tics can be primary, idiopathic or unknown, or secondary, due to specific recognized other causes. Many conditions present with secondary tics such as developmental disorders, neurodegenerative diseases, substance abuse, pregnancy, autoimmune disorders or infections, medications or various toxins.
References:
- Ganos, C., & Martino, D. (2015). Tics and Tourette syndrome. Neurologic Clinics, 33(1), 115–136.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 20
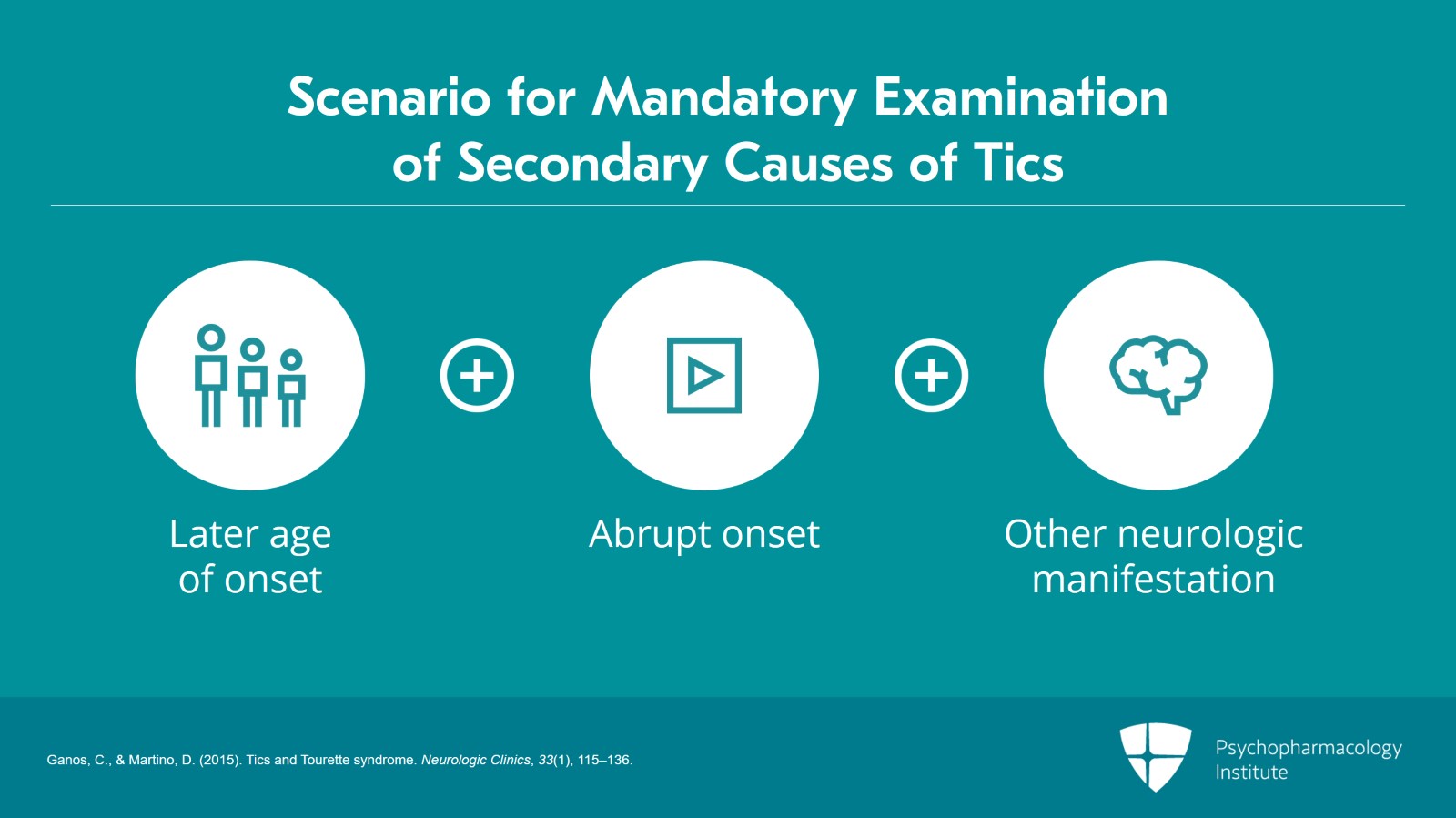
Later age at onset such as late adolescence or adulthood, abrupt onset and association with other neurological manifestation must prompt an examination of possible secondary causes of tics.
References:
- Ganos, C., & Martino, D. (2015). Tics and Tourette syndrome. Neurologic Clinics, 33(1), 115–136.
Slide 8 of 20
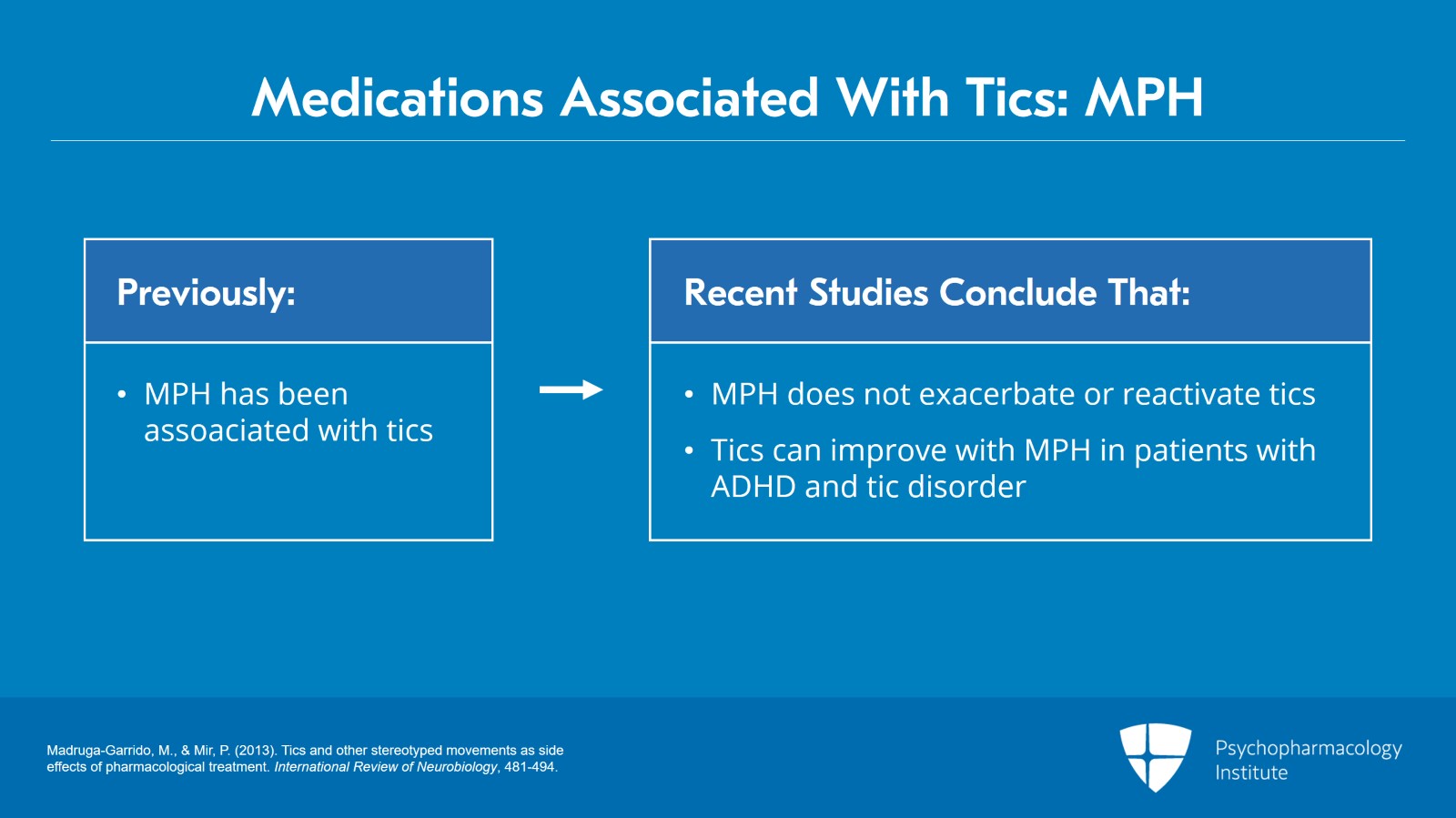
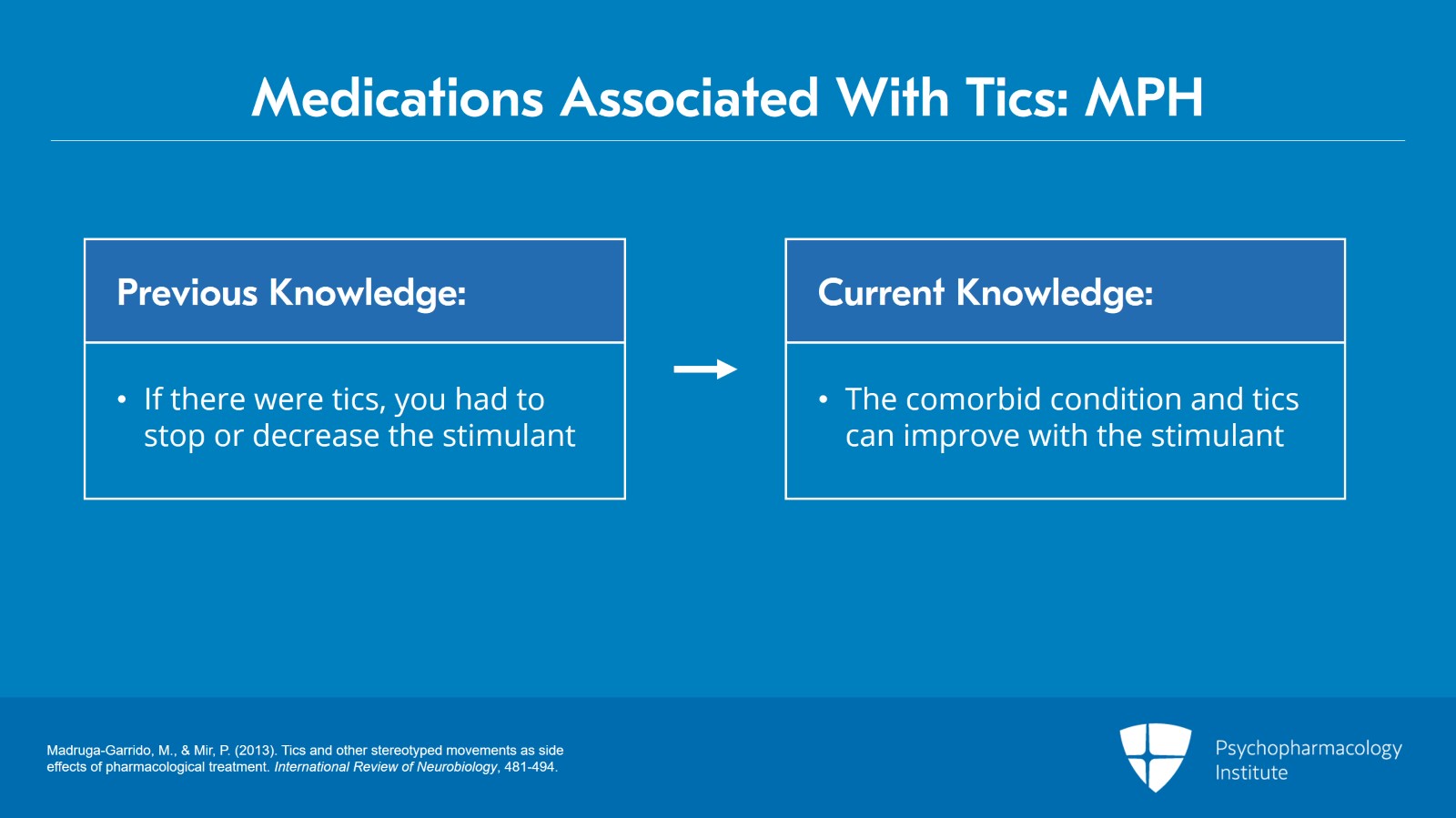
There are medications that are associated with tics. And I want to bring this up because it's important to emphasize that while psychostimulants particularly methylphenidate have been reported to be associated with tics due to increased dopamine activity caused by stimulants there are several recent studies that have concluded very compellingly that methylphenidate actually does not exacerbate or reactivate tics and that tics can actually improve with its use in patients with associated ADHD and tic disorder.
References:
- Madruga-Garrido, M., & Mir, P. (2013). Tics and other stereotyped movements as side effects of pharmacological treatment. International Review of Neurobiology, 481-494.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 20
And this is something critically important because there had been a belief for a considerable period of time that if there were tics associated with stimulant medicines you had to stop or decrease or be very, very careful with using stimulant. And while caution is necessary for the use of any psychotropic medicine, the more we're learning about this is that oftentimes not only will the comorbid condition, in this case ADHD, be improved with a stimulant but the tics as well. So we shouldn't rush to discontinue a medicine that may in fact be effective.
References:
- Madruga-Garrido, M., & Mir, P. (2013). Tics and other stereotyped movements as side effects of pharmacological treatment. International Review of Neurobiology, 481-494.
Slide 10 of 20
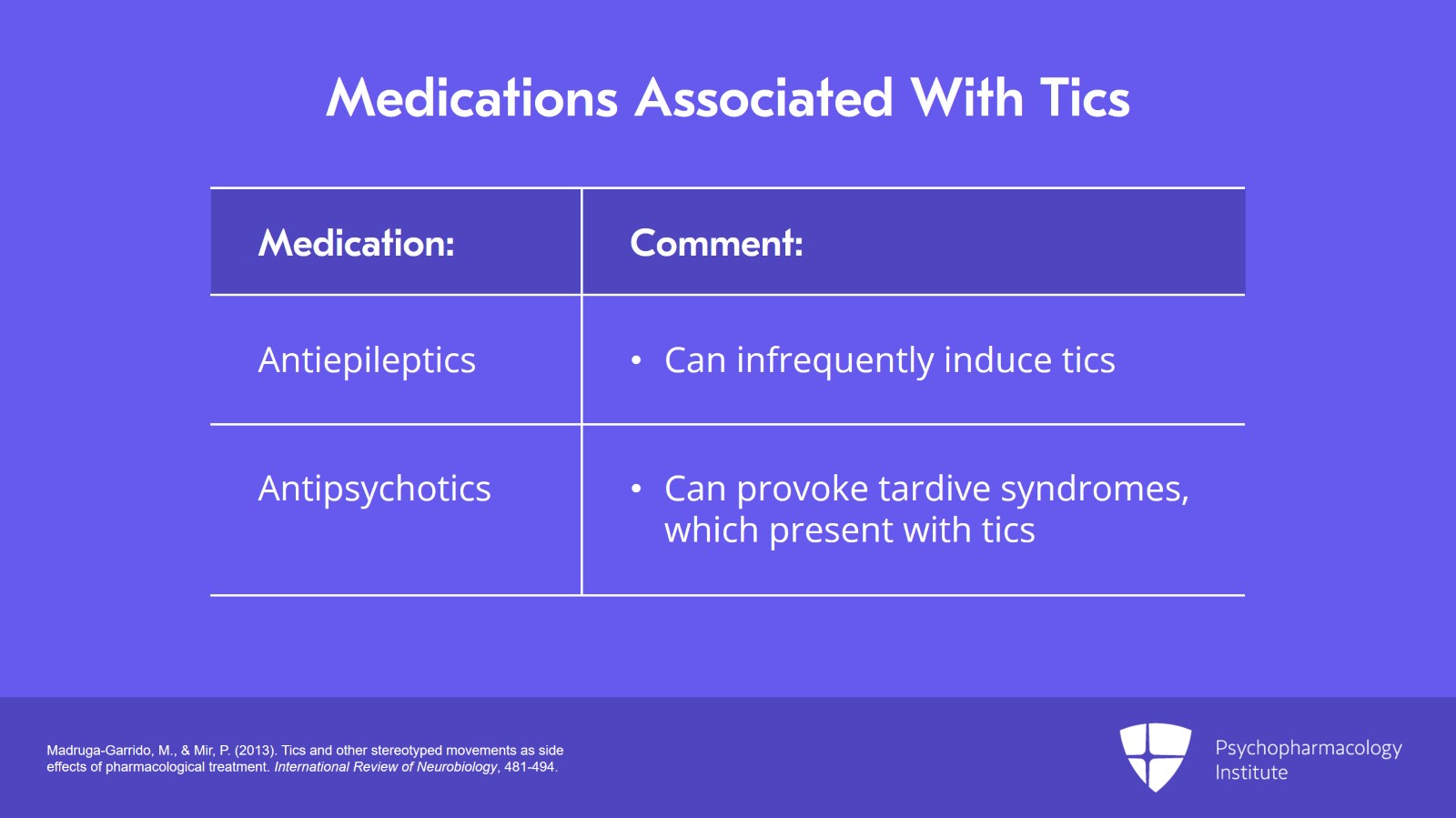
Antiepileptic drugs can infrequently induce tics with carbamazepine and lamotrigine described as tic inducers. Antipsychotic medications particularly the traditional antipsychotics such as haloperidol can provoke tardive syndromes such as tardive tics, tardive dyskinesia, or tardive akathisia which present with tics or stereotype movements.
References:
- Madruga-Garrido, M., & Mir, P. (2013). Tics and other stereotyped movements as side effects of pharmacological treatment. International Review of Neurobiology, 481-494.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 20
Many children with mild-to-moderate tic severity experience absolutely no distress or impairment and may even be unaware of their tics.
References:
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Slide 12 of 20
Individuals with more severe symptoms generally have more impairment in daily living but may still function well. Less commonly, tics disrupt functioning and daily activities and result in social isolation interpersonal conflict, bullying from peers, inability to work or go to school, substantial psychological distress and lower quality of life.
References:
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 20
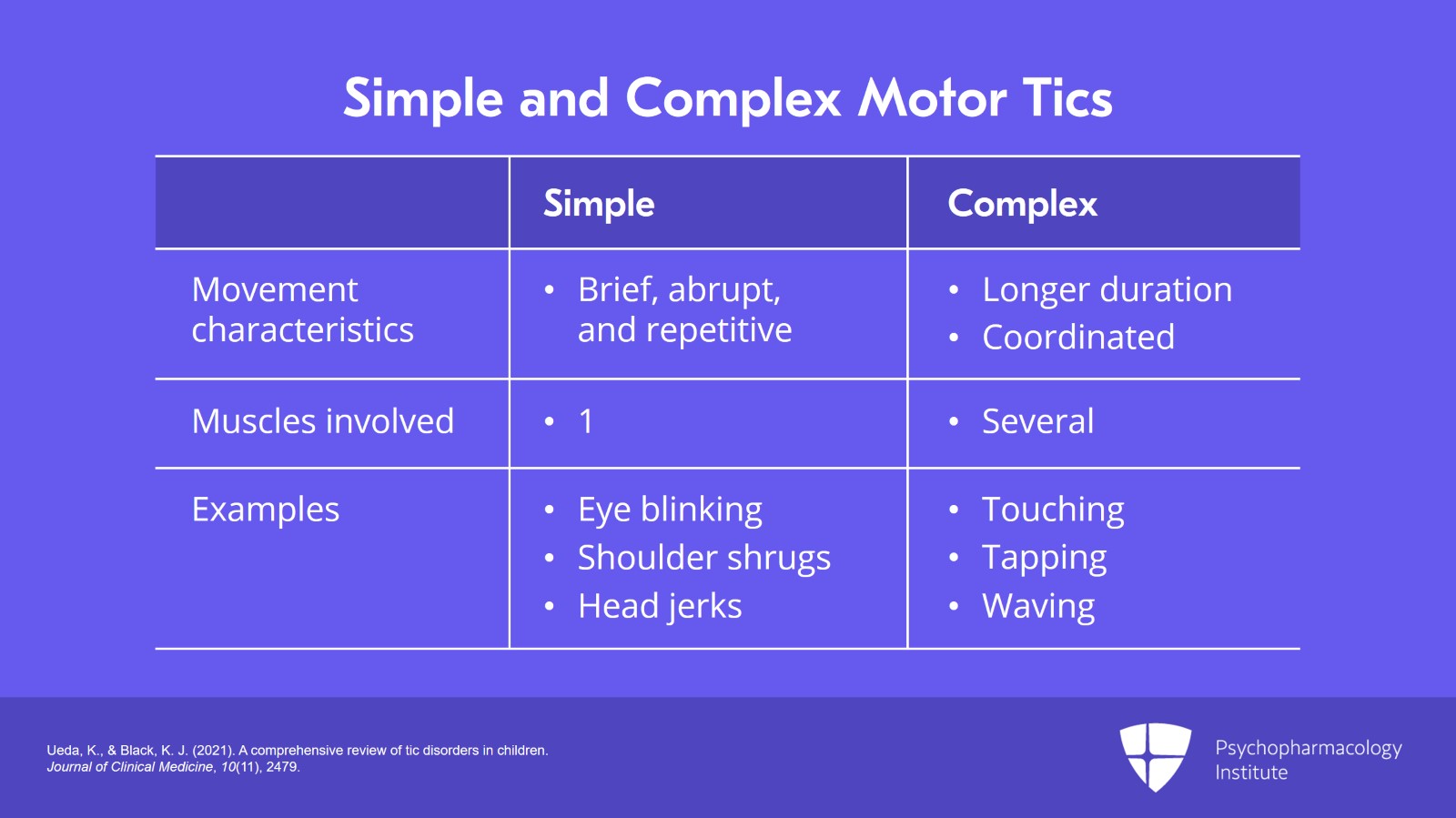
Simple motor tics are characterized by brief, abrupt, repetitive and seemingly non-purposeful movements that involve only one muscle group or body part such as the face, neck, shoulders, or hands. And examples of these are eye blinking, shoulder shrugs, head jerks, or facial grimaces. Complex motor tics are characterized by movements of longer duration caused by several muscle groups and that sometimes appear to be purposeful, coordinated, or orchestrated patterns of movement. And this would include touching, tapping, waving, kicking, jumping, mimicking other gestures (we call that echopraxia) or performing obscene or forbidden gestures or inappropriate touching (copropraxia).
References:
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Slide 14 of 20
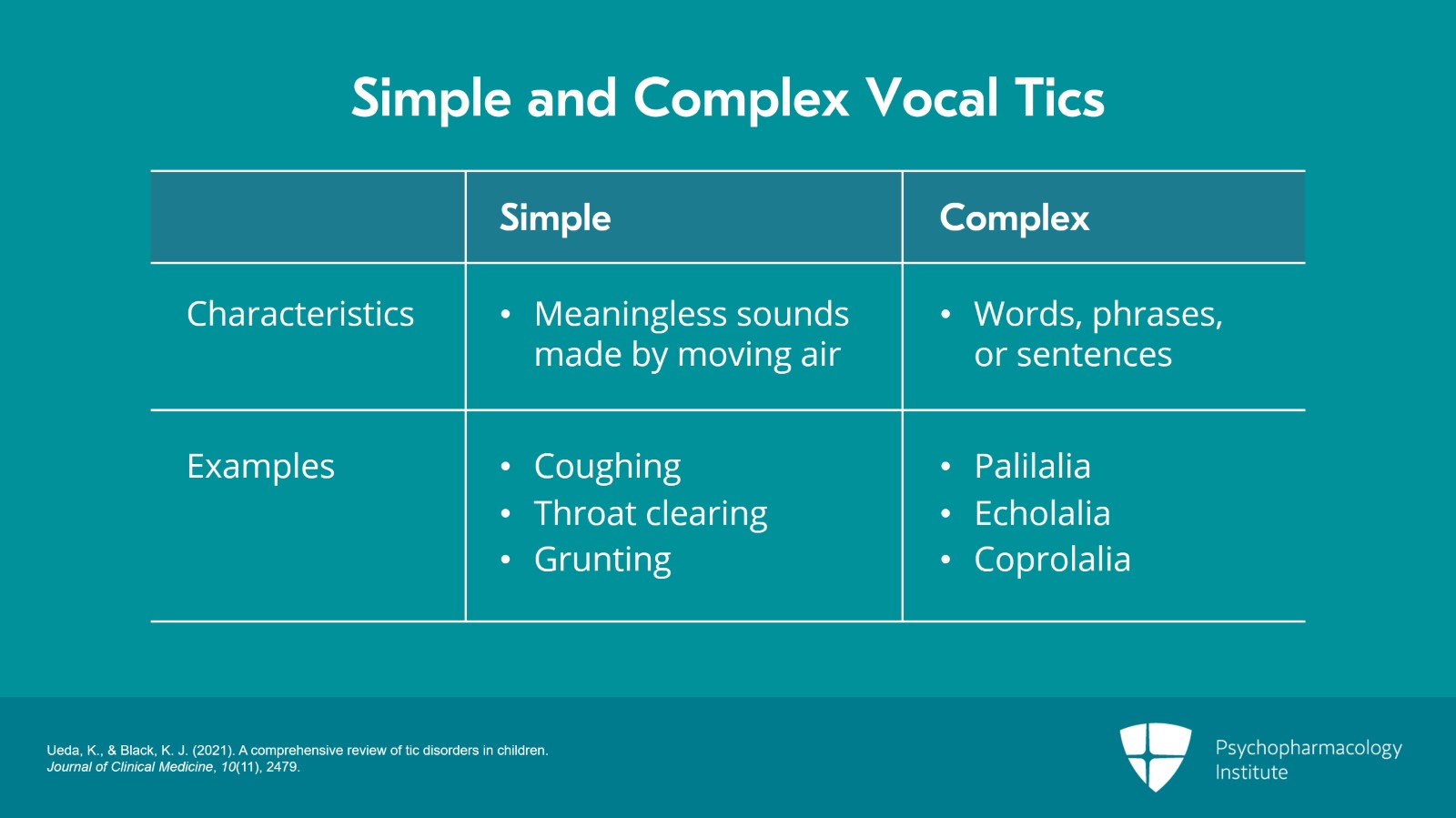
Vocal/phonic tics. Simple vocal/phonic tics are meaningless sounds made by moving air through the nose, mouth or throat. The sound may be produced by the contraction of the vocal cords as well as nasal, oral, laryngeal, pharyngeal, or respiratory muscles such as coughing, throat clearing, grunting, mimicking animal noises, screaming, or tongue clicking. In contrast, complex vocal or phonic tics involve several muscle groups and are characterized by words, phrases or sentences, include repeating one's own sounds or words (palilalia), repeating the last word or phrase (echolalia) or uttering socially unacceptable words including obscenities or ethnic, racial or religious slurs (coprolalia). And there's been a lot of discussion about coprolalia or uncontrolled swearing. Fortunately, that occurs in a minority of patients with tic disorders.
References:
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 20
Although tic disorders are defined by motor and/or vocal tics, many individuals also experience recurrent unpleasant somatosensory sensations that we refer to as premonitory urges. And premonitory urges are often described as pressure, discomfort or tingling in the muscles involved in the performance of the tics. These sensations prompt the performance of the tic which is followed by momentary relief of the associated discomfort but I emphasize momentary.
References:
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Slide 16 of 20
Up to 90% of individuals with tic disorders report experiencing premonitory urges with some reporting that the urges cause more distress than the tics themselves.
References:
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 20
Tics may also be voluntary suppressed for short periods of time and many report that intensity of premonitory urges increases during tic suppression. And that's important because there can be rebound periods where there's just a great exacerbation after trying to hold in the tics for a long time. So they can get worse or there's a necessary release after working hard to control the tics.
References:
- Ueda, K., & Black, K. J. (2021). A comprehensive review of tic disorders in children. Journal of Clinical Medicine, 10(11), 2479.
Slide 18 of 20
Key points that are important to take home are: The psychological, physical strains, and environmental changes can in fact exacerbate tics. And we know that later age of onset and abrupt versus a more gradual onset and an association with other neurological manifestations mandate prompt examination of secondary causes of tics.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 20
And finally, and this is due to more recent investigation, while psychostimulants mainly methylphenidate are thought to be associated with tics, there are now several good studies that demonstrate that methylphenidate does not exacerbate or reactivate tics but can improve these in patients with associated ADHD and tic disorders.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.