Slides and Transcript
Slide 2 of 11
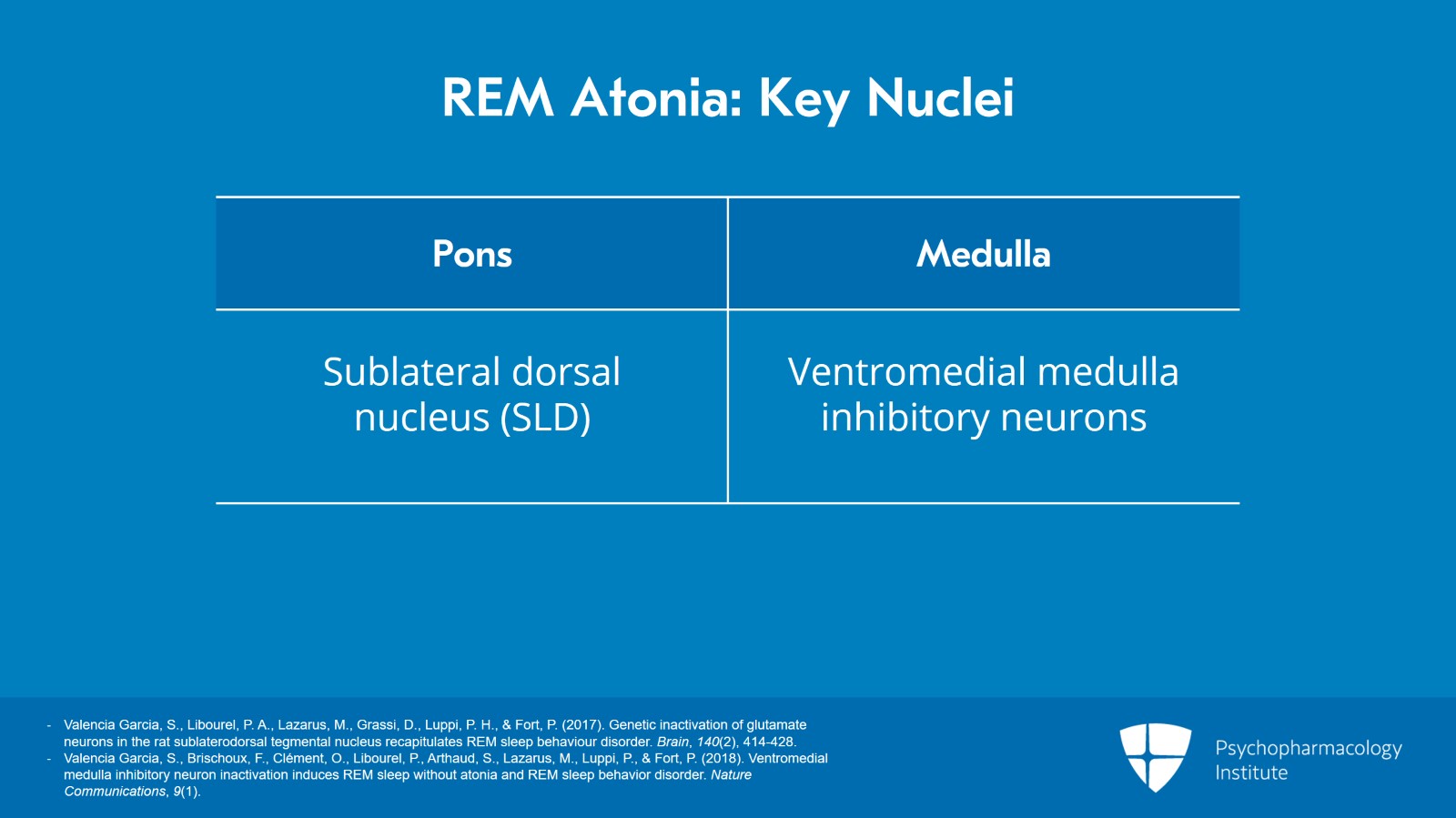
We now know through very elegant basic science studies that there are two key linked brainstem nuclei that generate REM atonia: One is in the pons and the other is in the medulla.
The pontine tegmentum has the sublateral dorsal nucleus known as the SLD that is linked with the ventromedial medulla inhibitory neurons in the medulla.
References:
- Valencia Garcia, S., Libourel, P. A., Lazarus, M., Grassi, D., Luppi, P. H., & Fort, P. (2017). Genetic inactivation of glutamate neurons in the rat sublaterodorsal tegmental nucleus recapitulates REM sleep behaviour disorder. Brain, 140(2), 414-428.
- Valencia Garcia, S., Brischoux, F., Clément, O., Libourel, P., Arthaud, S., Lazarus, M., Luppi, P., & Fort, P. (2018). Ventromedial medulla inhibitory neuron inactivation induces REM sleep without atonia and REM sleep behavior disorder. Nature Communications, 9(1).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 11
Genetic inactivation of these two nuclei results in a loss of REM atonia and REM sleep behavior disorder in rats.
References:
- Valencia Garcia, S., Libourel, P. A., Lazarus, M., Grassi, D., Luppi, P. H., & Fort, P. (2017). Genetic inactivation of glutamate neurons in the rat sublaterodorsal tegmental nucleus recapitulates REM sleep behaviour disorder. Brain, 140(2), 414-428.
- Valencia Garcia, S., Brischoux, F., Clément, O., Libourel, P., Arthaud, S., Lazarus, M., Luppi, P., & Fort, P. (2018). Ventromedial medulla inhibitory neuron inactivation induces REM sleep without atonia and REM sleep behavior disorder. Nature Communications, 9(1).
Slide 4 of 11
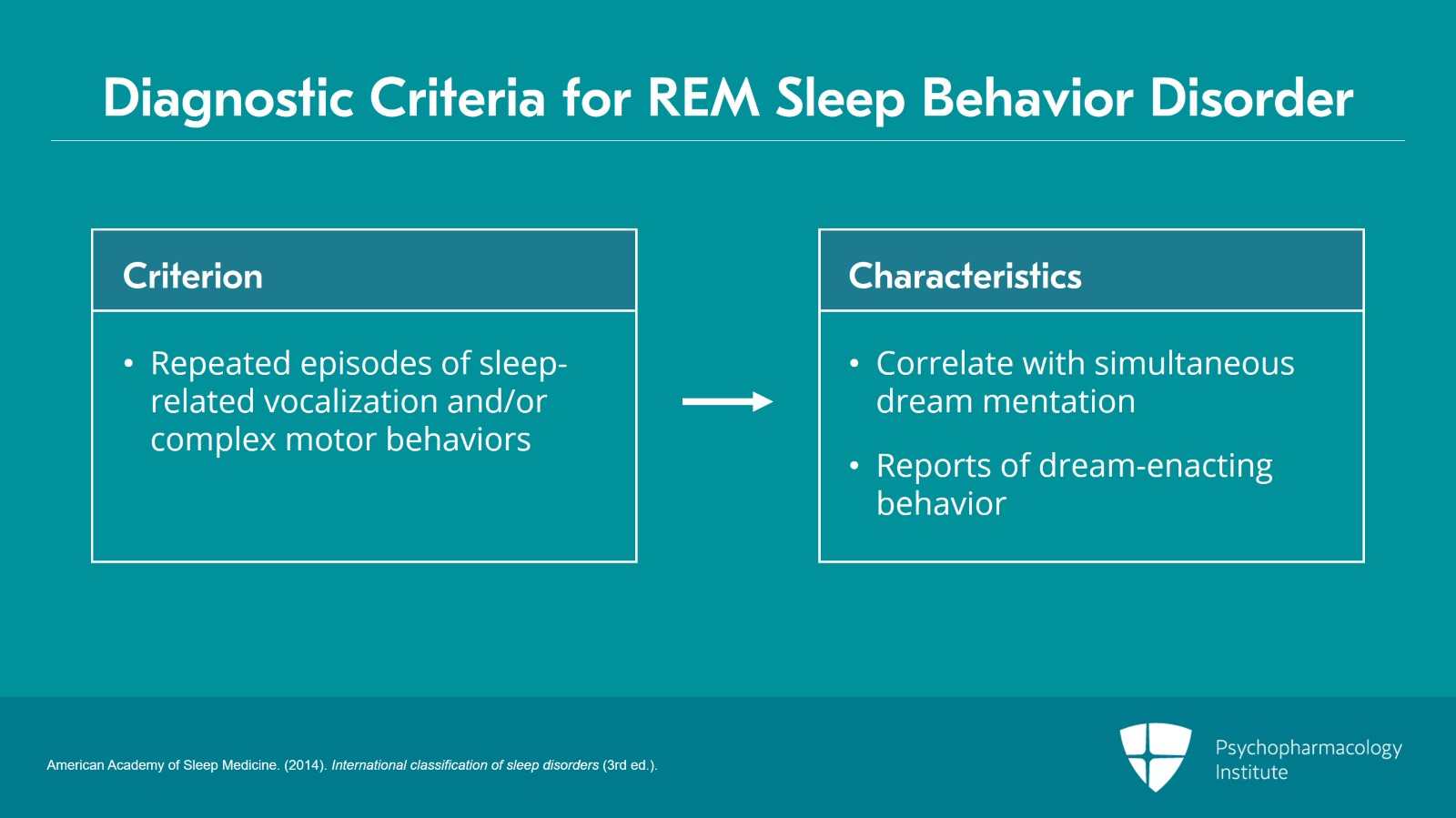
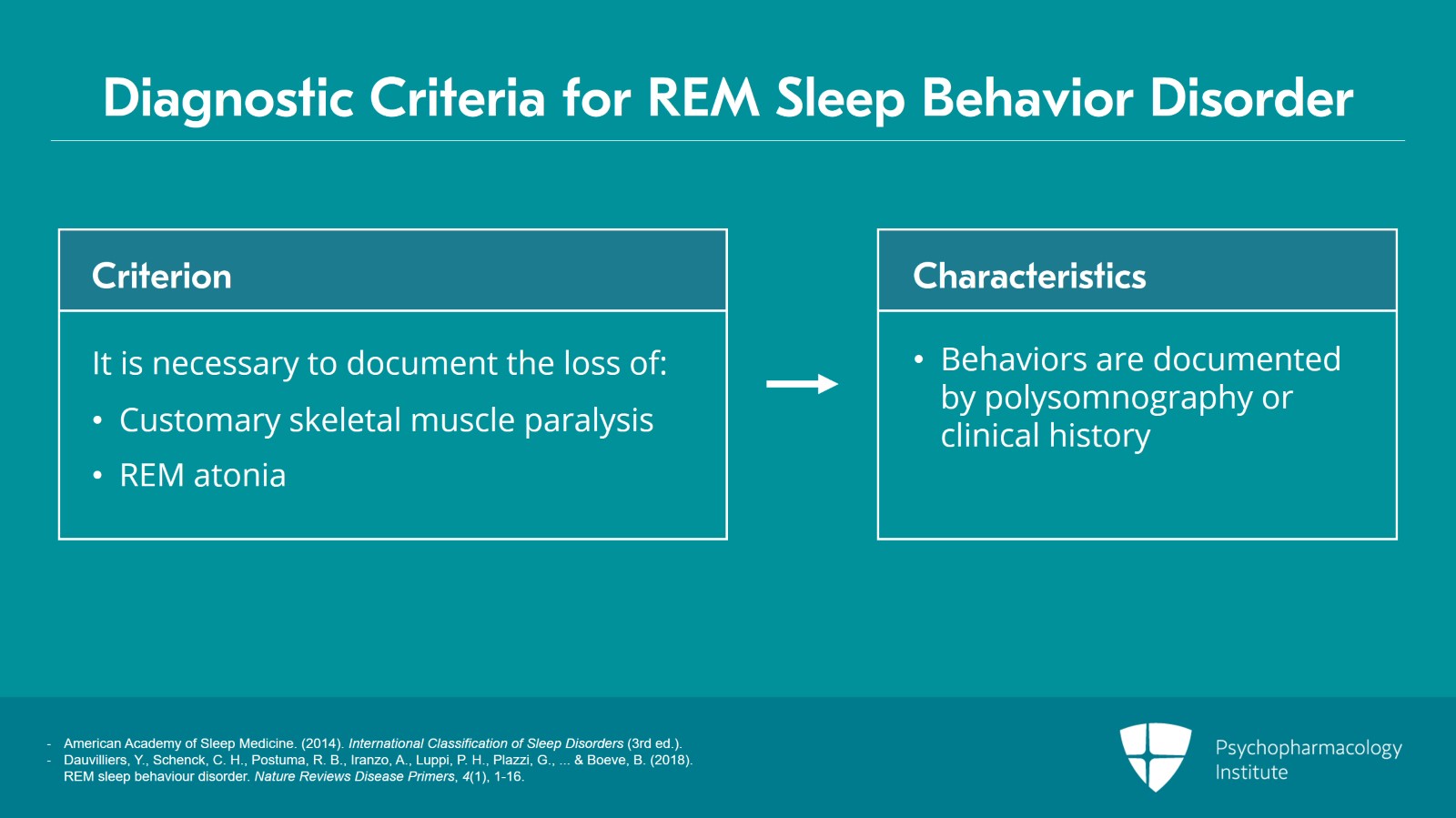
The diagnostic criteria for RBD in humans from the International classification of sleep disorders:
First of all, repeated episodes of sleep-related vocalization and/or complex motor behaviors.
The observed vocalizations or behaviors often correlate with simultaneously occurring dream mentation leading to the frequent report of “acting out one’s dreams.” Dream-enacting behavior is very common with RBD but it’s not universally found which is why it’s not one of the diagnostic criteria.
References:
- American Academy of Sleep Medicine. (2014). International classification of sleep disorders (3rd ed.).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 11
I should point out that REM sleep behavior disorder is the only parasomnia for which video polysomnography is required. It is necessary to document the loss of the customary skeletal muscle paralysis or REM atonia of mammalian REM sleep. This is critical. An objective diagnosis is needed to document and diagnose REM sleep behavior disorder.
These behaviors are documented by polysomnography to occur during REM sleep or based on clinical history of dream enactment are presumed to occur during REM sleep.
References:
- American Academy of Sleep Medicine. (2014). International Classification of Sleep Disorders (3rd ed.).
- Dauvilliers, Y., Schenck, C. H., Postuma, R. B., Iranzo, A., Luppi, P. H., Plazzi, G., … & Boeve, B. (2018). REM sleep behaviour disorder. Nature Reviews Disease Primers, 4(1), 1-16.
Slide 6 of 11
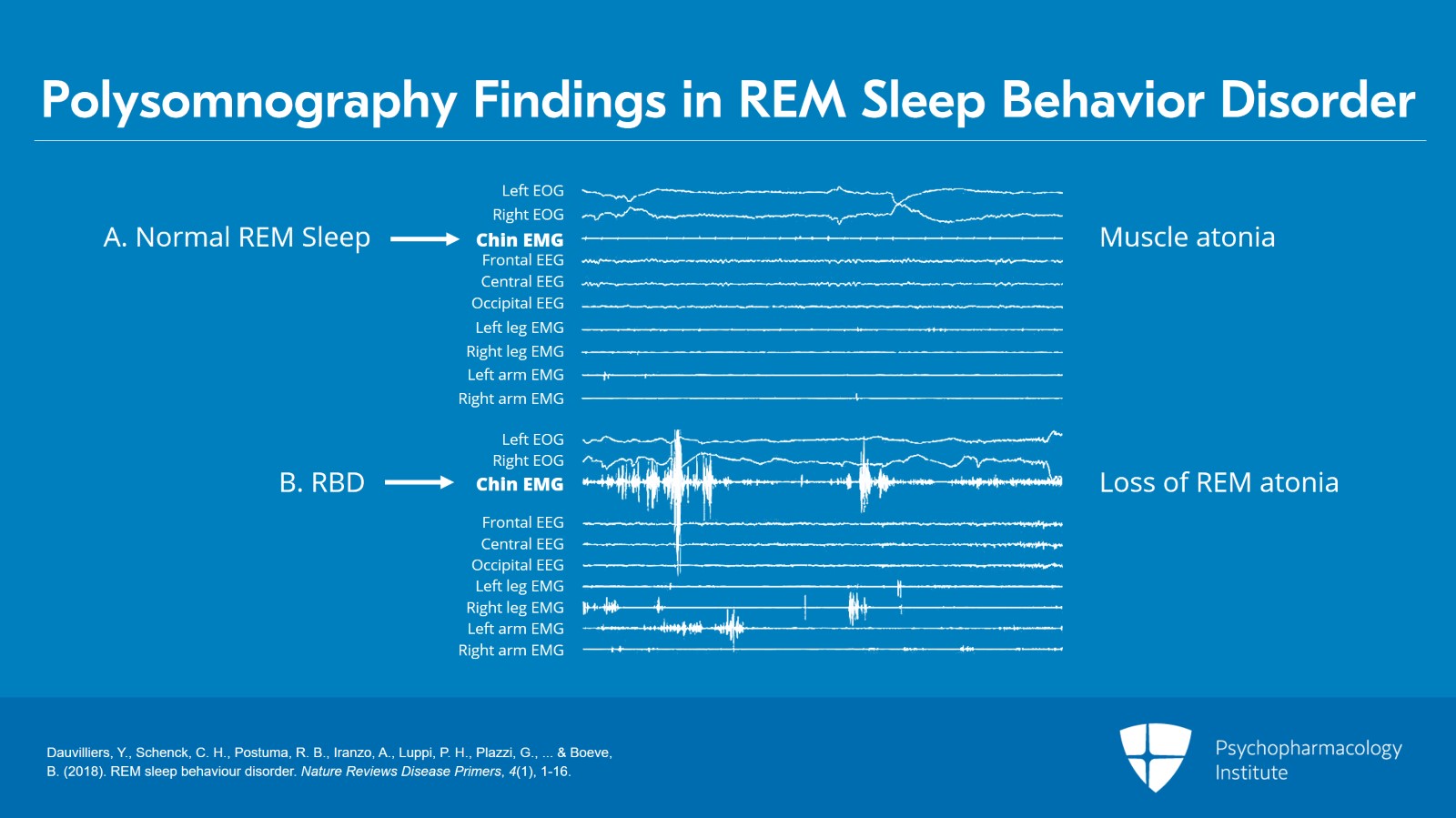
And in the figure that we have here in the top panel A, if you look at the third tracing for the chin electromyogram, this is the chin EMG of normal REM sleep and you will see a flat line indicating muscle atonia. It’s an active muscle paralysis generated in the brainstem.
However, in contrast, in panel B, if you look at the chin EMG, you see increased muscle tone and phasic twitching. This is abnormal and this is what’s found with REM sleep behavior disorder. So it’s really easy to pick up the loss of REM atonia with RBD in contrast to normal REM sleep and normal REM sleep atonia.
References:
- Dauvilliers, Y., Schenck, C. H., Postuma, R. B., Iranzo, A., Luppi, P. H., Plazzi, G., … & Boeve, B. (2018). REM sleep behaviour disorder. Nature Reviews Disease Primers, 4(1), 1-16.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 11
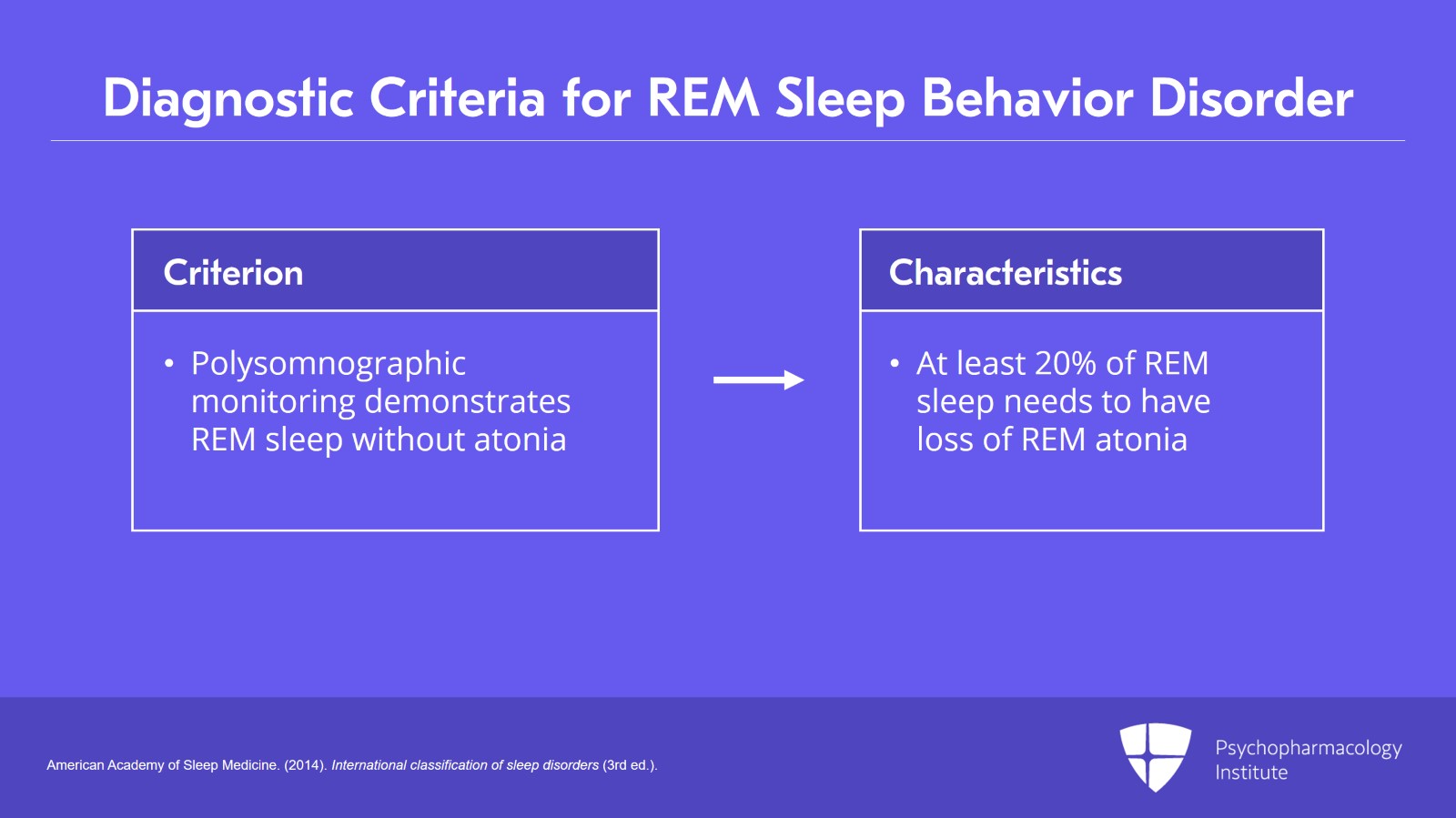
Third, polysomnographic monitoring demonstrates REM sleep without atonia known as RWA.
One question that’s frequently asked of me by sleep physicians, not just other specialists, is how much loss of REM atonia do you need to feel confident in diagnosing REM sleep behavior disorder because there’s no absolute cut-off. And generally, it’s at least 20% of REM sleep needs to have loss of REM atonia to feel confident with the diagnosis, particularly if there’s a convincing clinical history of dream enactment.
References:
- American Academy of Sleep Medicine. (2014). International classification of sleep disorders (3rd ed.).
Slide 8 of 11
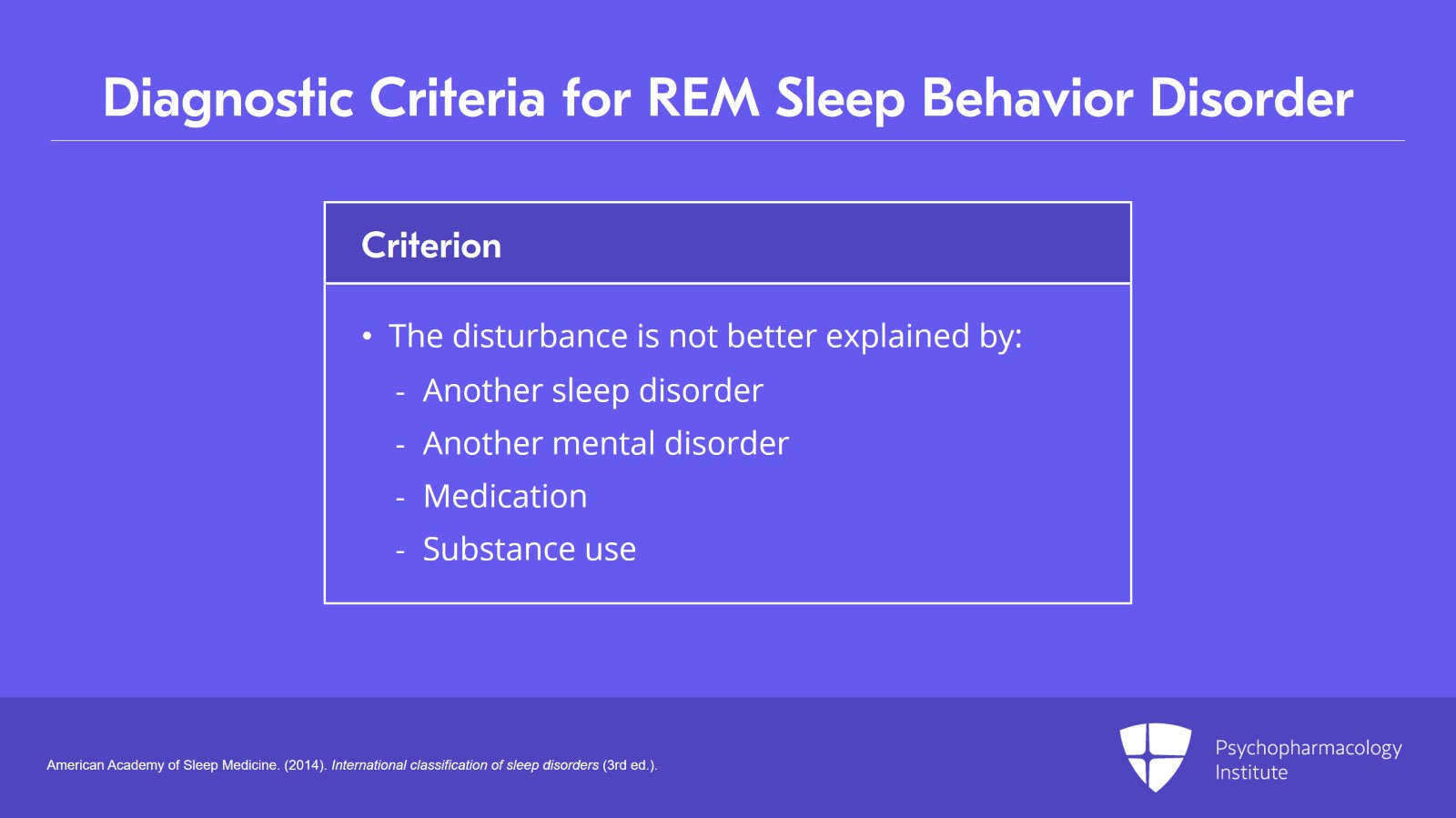
And fourth, the disturbance is not better explained by another sleep disorder, mental disorder, medication or substance use.
And this is not particularly relevant with RBD because of the objective finding of REM without atonia.
References:
- American Academy of Sleep Medicine. (2014). International classification of sleep disorders (3rd ed.).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 11
Now, the first study that came from our center on REM sleep behavior disorder was in 1986 on a series of five patients.
We then followed up the next year in the Journal of the American Medical Association that we named RBD in the title: Rapid Eye Movement Sleep Behavior Disorder, a Treatable Parasomnia Affecting Older Adults. And so, in our first series of 10 patients, five had an identified neurological disorder that caused RBD, and five patients had no identified neurological disorder and we called them idiopathic RBD.
References:
- Schenck, C. H., Bundlie, S. R., Patterson, A. L., & Mahowald, M. W. (1987). Rapid eye movement sleep behavior disorder: A treatable parasomnia affecting older adults. JAMA, 257(13), 1786-1789.
Slide 10 of 11
So the key points are:
Specific nuclei in the pons and medulla in the brainstem generate the muscle paralysis of REM sleep called REM atonia.
Various neurological and other disorders can damage these brainstem nuclei causing loss of REM atonia and emergence of RBD.
And lastly, loss of REM atonia and objective finding from polysomnography is required to diagnose RBD.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.