Slides and Transcript
Slide 1 of 21
Constipation represents one of the most serious adverse effects of clozapine and every clinician really needs to become expert in managing this.
Slide 2 of 21
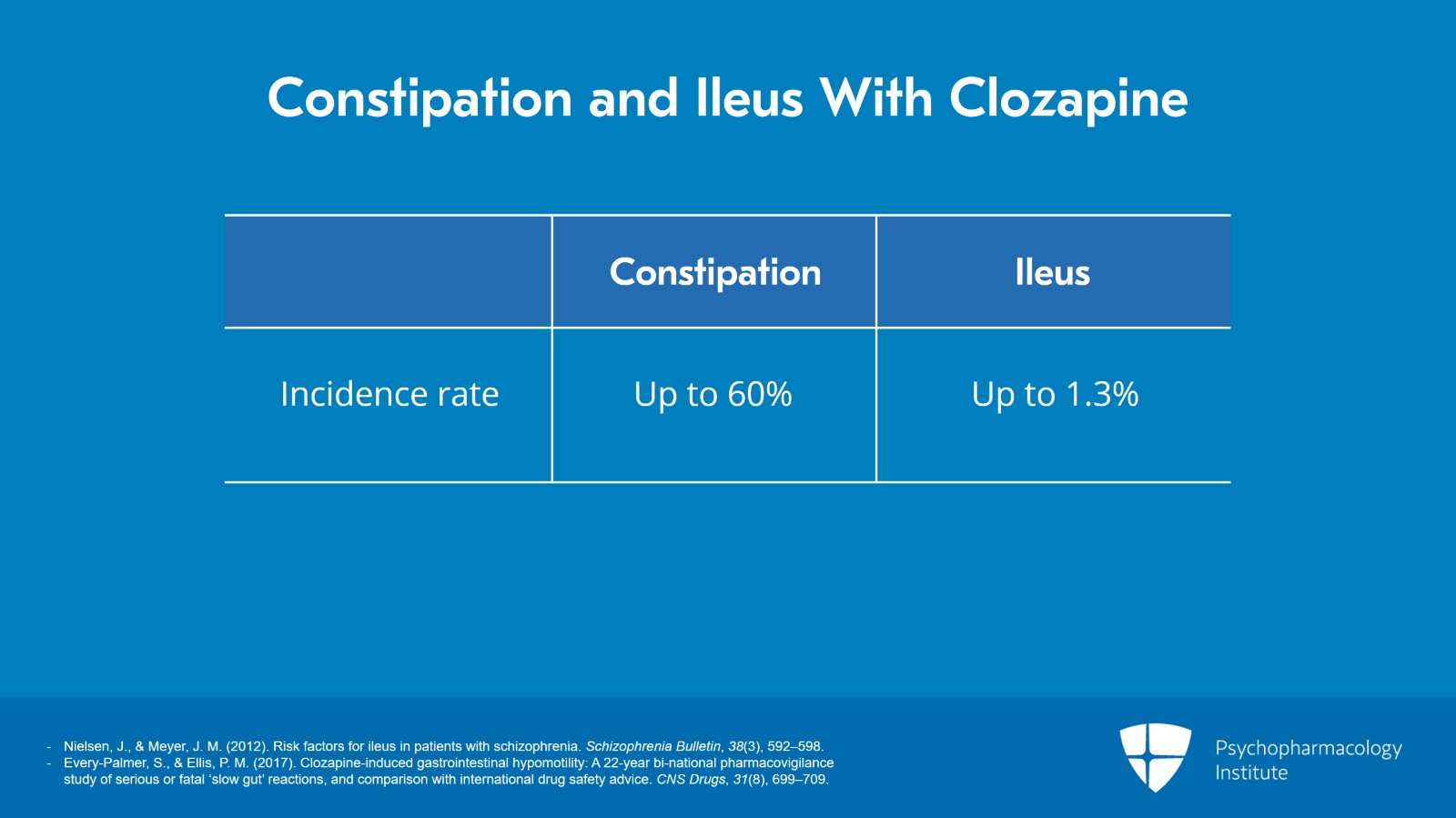
The rate of constipation is very high, up to 60% incidence reported. And for ileus, the rate is up to 1.3% and it is sometimes fatal. In fact, in January 2020, the US FDA issued a warning in a bulletin about patients developing ileus on clozapine.
References:
- Nielsen, J., & Meyer, J. M. (2012). Risk factors for ileus in patients with schizophrenia. Schizophrenia Bulletin, 38(3), 592–598.
- Every-Palmer, S., & Ellis, P. M. (2017). Clozapine-induced gastrointestinal hypomotility: A 22-year bi-national pharmacovigilance study of serious or fatal ‘slow gut’ reactions, and comparison with international drug safety advice. CNS Drugs, 31(8), 699–709.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 21
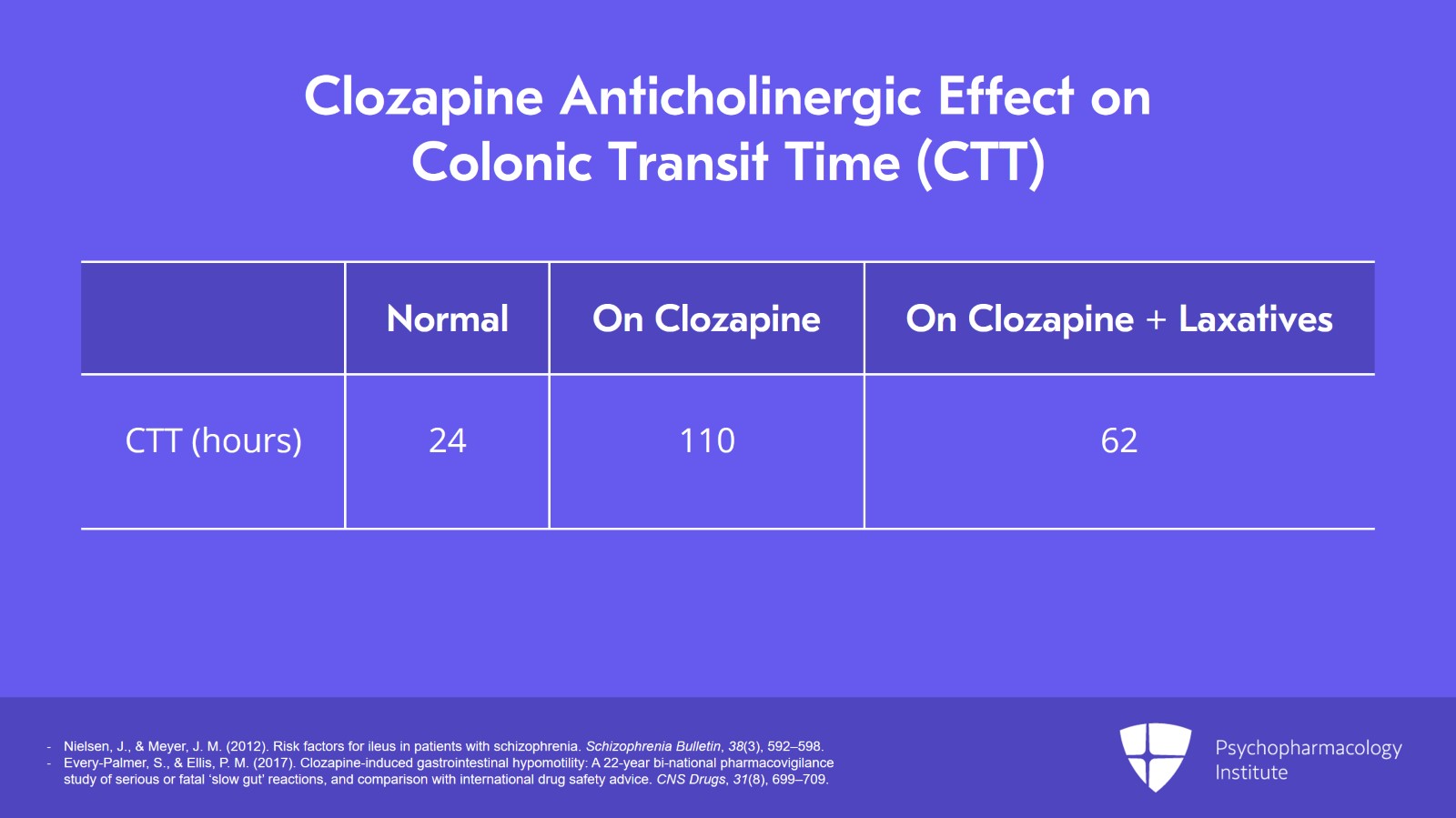
The reason constipation is such a problem is that clozapine is strongly anticholinergic. The average colonic transit time or CTT in normal adults is 24 hours but on clozapine patients have median colonic transit times of 110 hours. Once you treat these clozapine patients with maximal doses of each of the three common classes of laxatives such as docusate plus an osmotic plus a stimulant, even then the median colonic transit time remains elevated at 62 hours.
References:
- Nielsen, J., & Meyer, J. M. (2012). Risk factors for ileus in patients with schizophrenia. Schizophrenia Bulletin, 38(3), 592–598.
- Every-Palmer, S., & Ellis, P. M. (2017). Clozapine-induced gastrointestinal hypomotility: A 22-year bi-national pharmacovigilance study of serious or fatal ‘slow gut’ reactions, and comparison with international drug safety advice. CNS Drugs, 31(8), 699–709.
Slide 4 of 21
Because the CTT, the colonic transit time, is so slow, you should not use bulk-forming laxatives containing psyllium in patients on clozapine to manage their constipation. The reason being is that the motility is so slow the psyllium can exacerbate the problem because it sits in the colon and dries out. The technical term is it becomes inspissated.
References:
- Nielsen, J., & Meyer, J. M. (2012). Risk factors for ileus in patients with schizophrenia. Schizophrenia Bulletin, 38(3), 592–598.
- Every-Palmer, S., & Ellis, P. M. (2017). Clozapine-induced gastrointestinal hypomotility: A 22-year bi-national pharmacovigilance study of serious or fatal ‘slow gut’ reactions, and comparison with international drug safety advice. CNS Drugs, 31(8), 699–709.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 21
Well, what are the basic principles? Well, number one, clozapine is an anticholinergic so minimize other systemically acting anticholinergics.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
- Nielsen, J., & Meyer, J. M. (2012). Risk factors for ileus in patients with schizophrenia. Schizophrenia Bulletin, 38(3), 592–598.
Slide 6 of 21
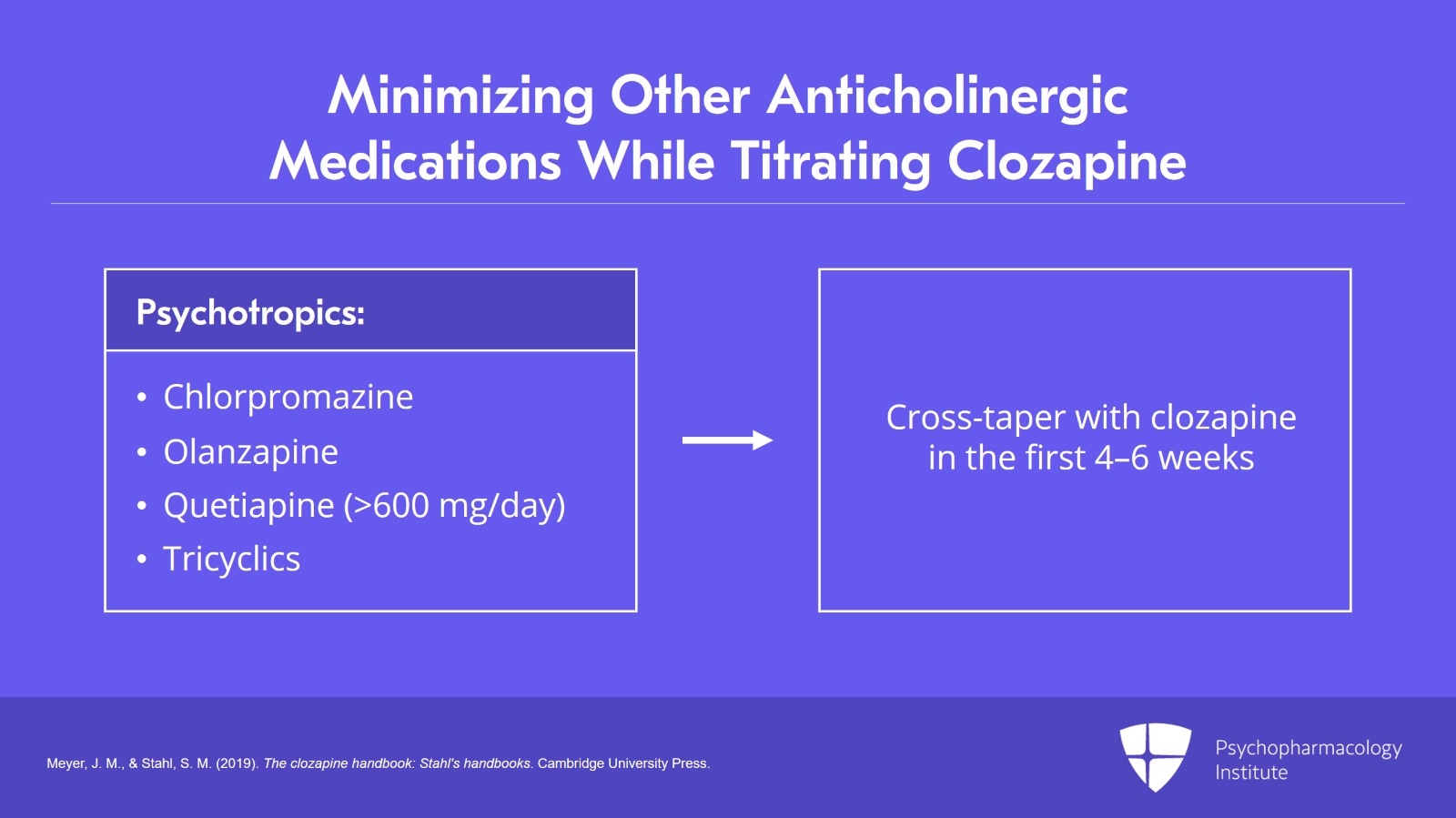
Well, here's the detailed approach to anticholinergic medications which the patient might be on and how to manage them. The strongly anticholinergic psychotropics are chlorpromazine, olanzapine, high dose quetiapine (more than 600 mg per day), and tricyclics. These medications should be cross-tapered as clozapine is added with the goal of discontinuation in the first four to six weeks.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 21
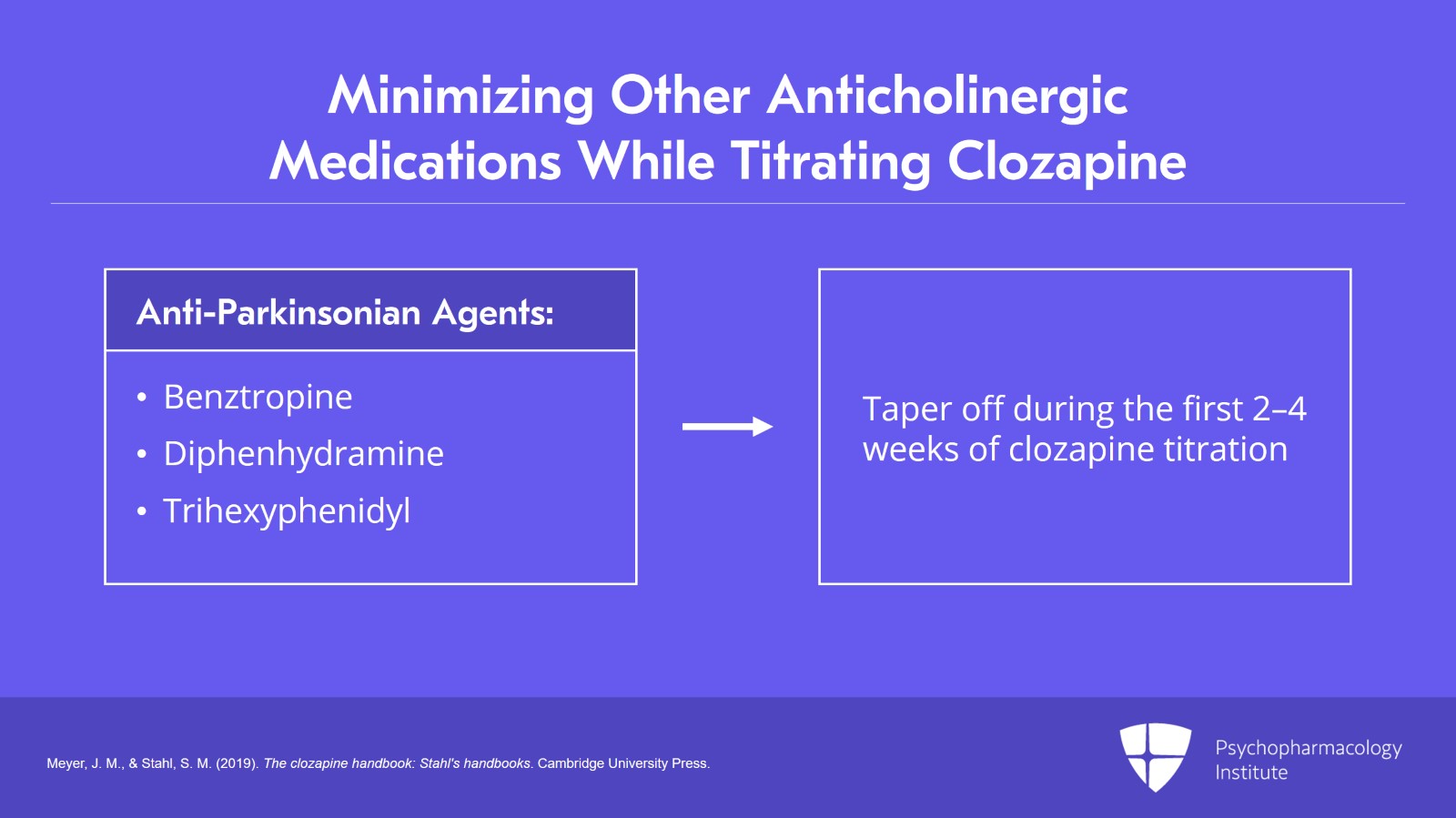
The next class of strongly anticholinergic medications are the anti-Parkinsonian agents: Benztropine, diphenhydramine, or trihexyphenidyl. Those agents should be tapered off during the first two to four weeks of clozapine titration.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
Slide 8 of 21
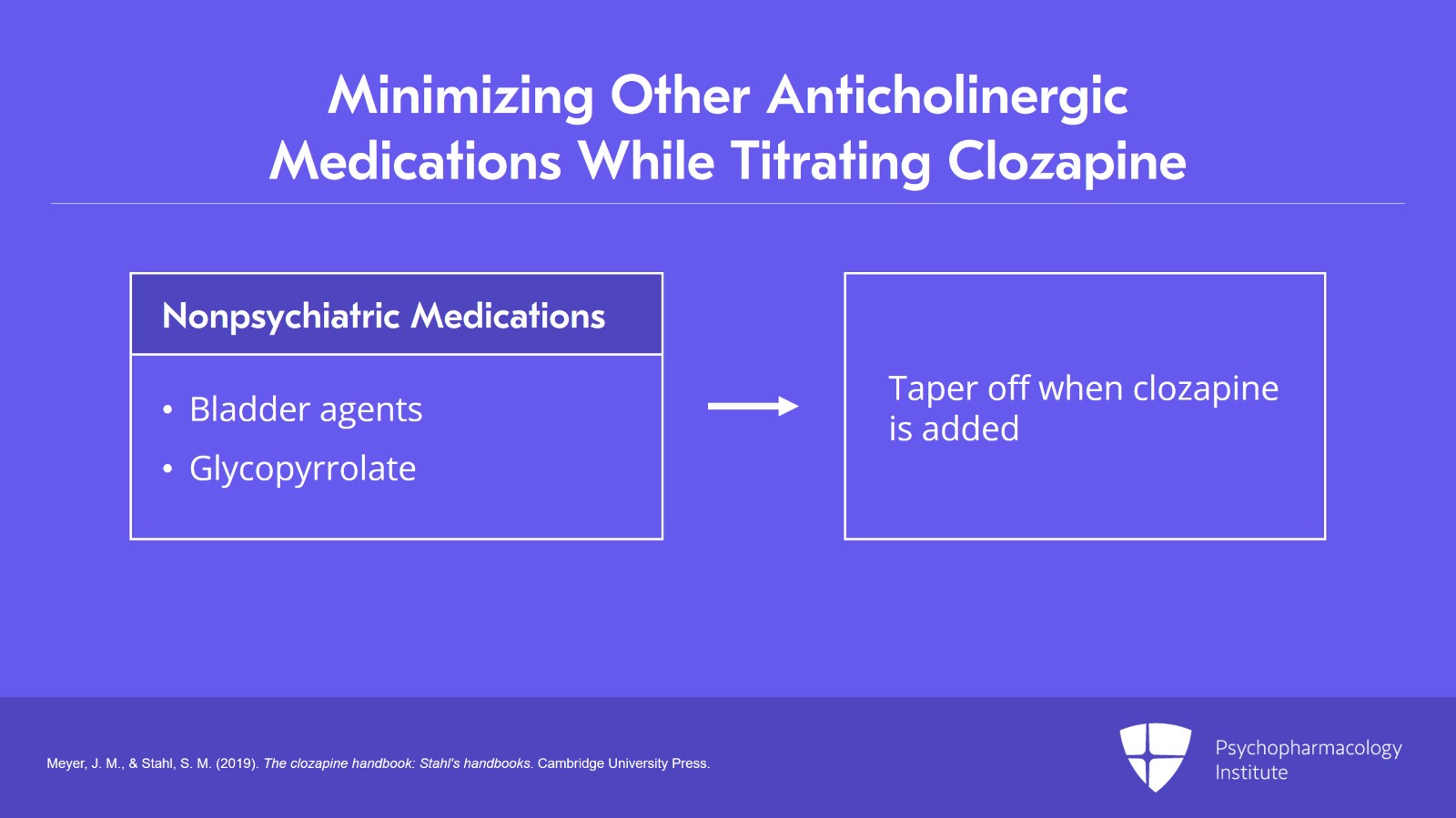
Lastly, don't forget about anticholinergic non-psychiatric medications. The bladder agents such as oxybutynin, tolterodine, and trospium and if for some reason, the patient is on glycopyrrolate this should also be tapered off when clozapine is added. As we discussed, you may have to add it back at some point to manage the sialorrhea but you really don't want it in place when you're starting clozapine therapy.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 21
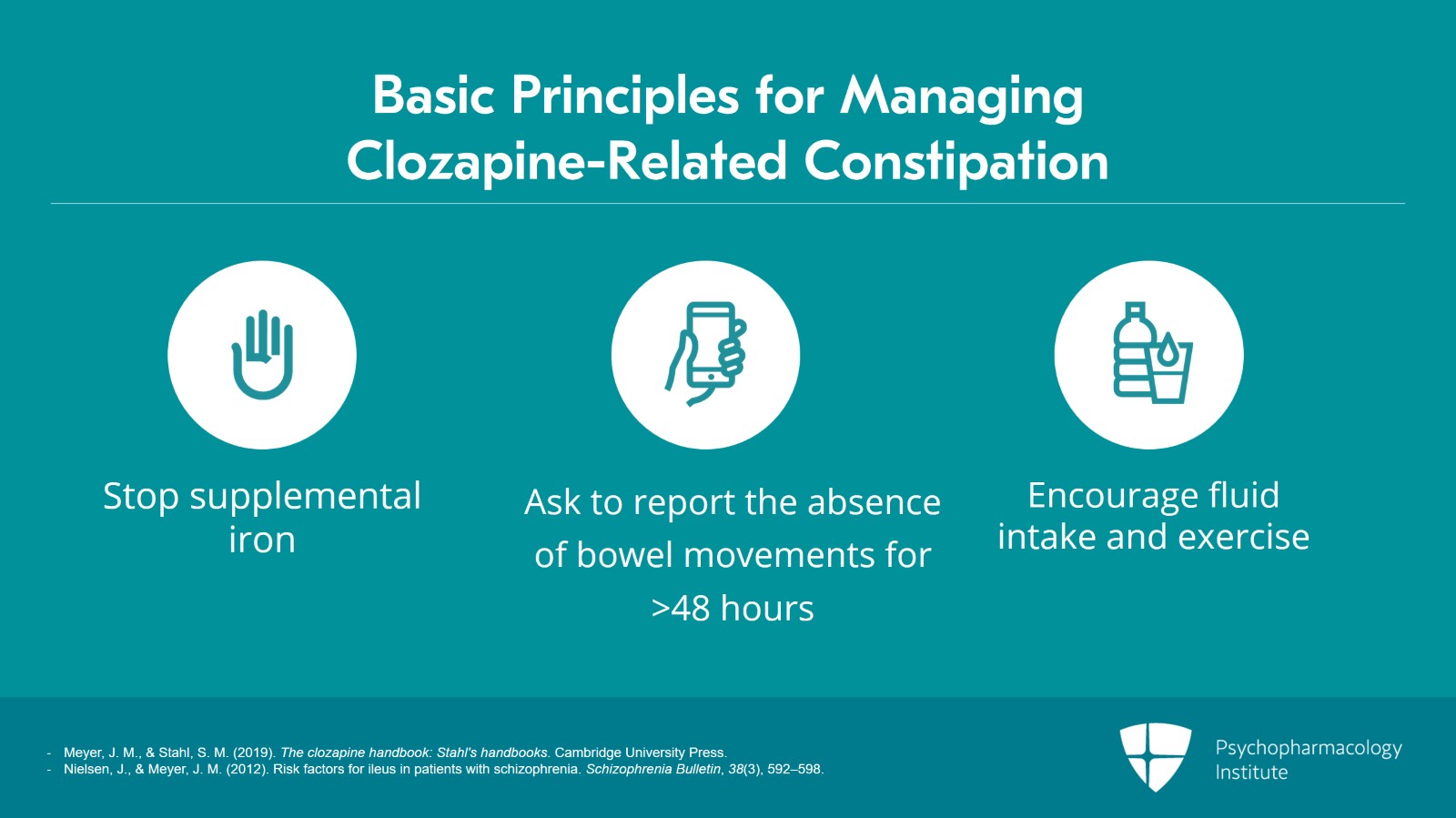
And when you're starting clozapine, initially stop supplemental iron. Patients can often be off of iron for a number of weeks with no harm. Once they are on a stable dose of clozapine and the constipation problem is managed, iron can be restarted later. Emphasize to the patient the need to report if they have no bowel movement for more than 48 hours. And of course, encourage fluid intake and exercise. Caregivers should also be given the same information so they can help monitor to see if their loved one with clozapine treatment is starting to develop problems of not having bowel movements over 48 hours.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
- Nielsen, J., & Meyer, J. M. (2012). Risk factors for ileus in patients with schizophrenia. Schizophrenia Bulletin, 38(3), 592–598.
Slide 10 of 21
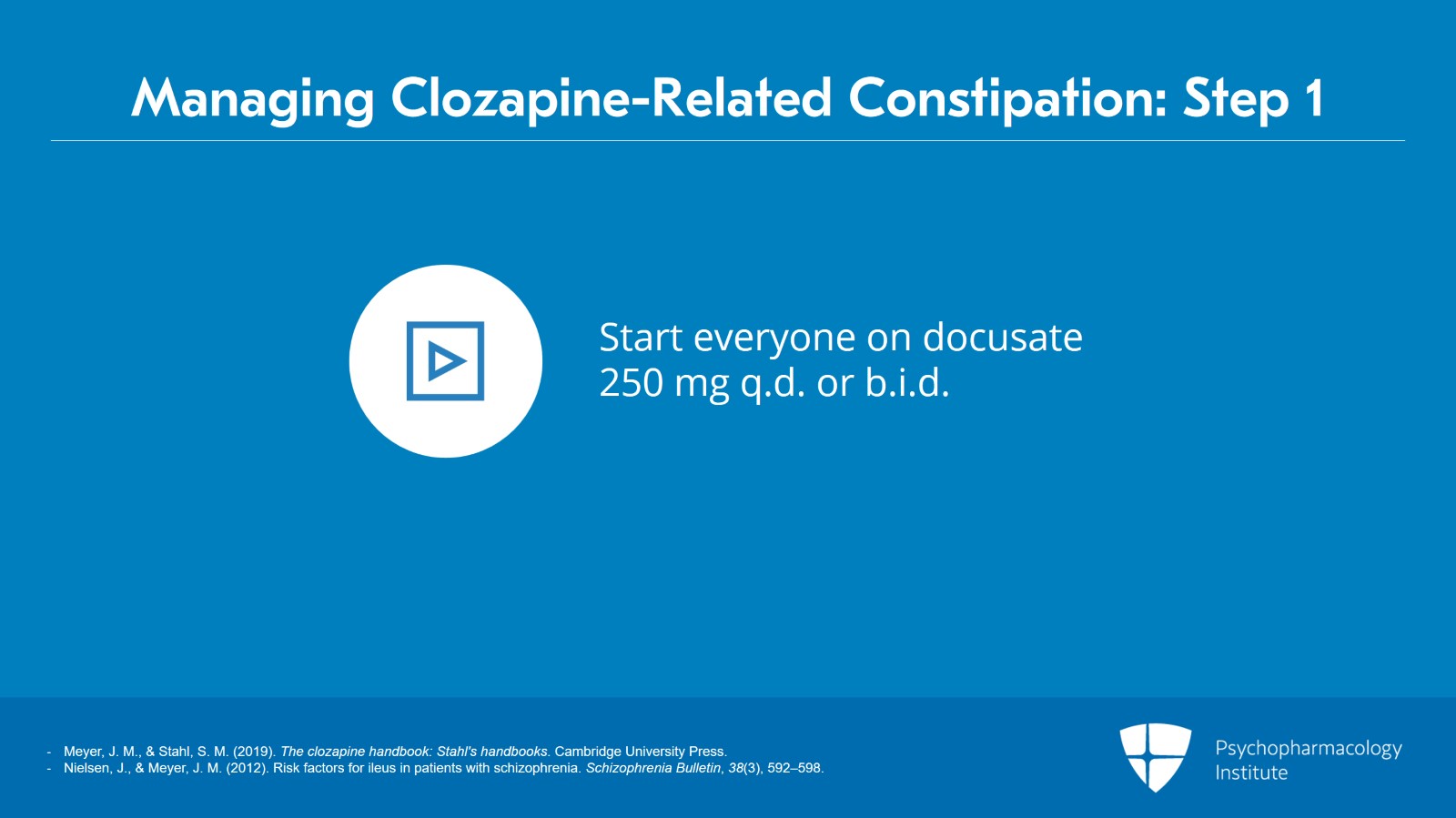
Everyone starting clozapine should be routinely commenced on docusate at a dose of 250 mg once a day or twice a day.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
- Nielsen, J., & Meyer, J. M. (2012). Risk factors for ileus in patients with schizophrenia. Schizophrenia Bulletin, 38(3), 592–598
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 21
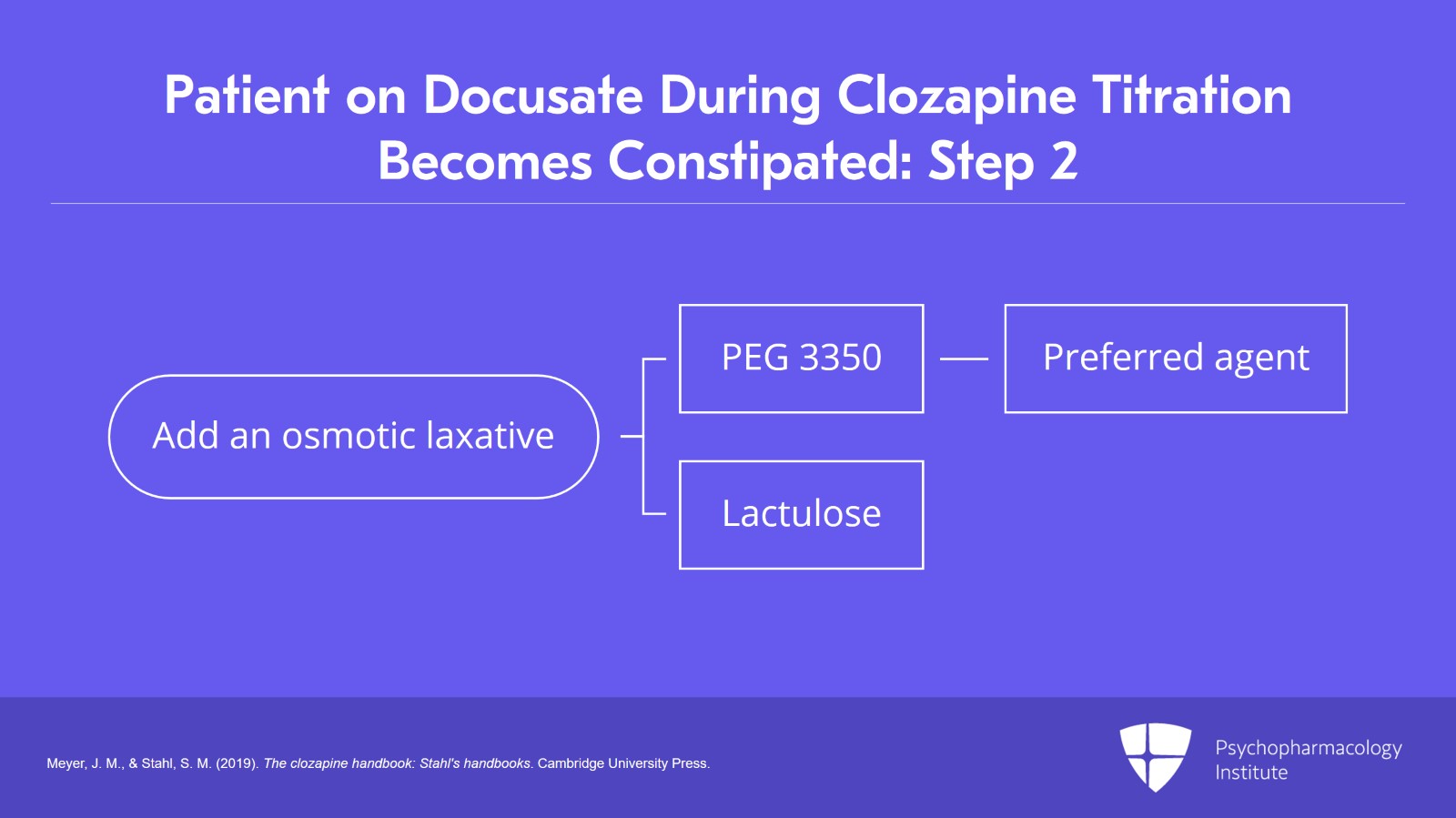
The patient is on docusate. You're titrating clozapine. They become constipated. What is the next step? Step two is to add an osmotic laxative. The two agents out there are either what's called PEG 3350 or polyethylene glycol 3350 or lactulose. PEG 3350 has better efficacy data overall for constipation and this is the agent we prefer to use as step two.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
Slide 12 of 21
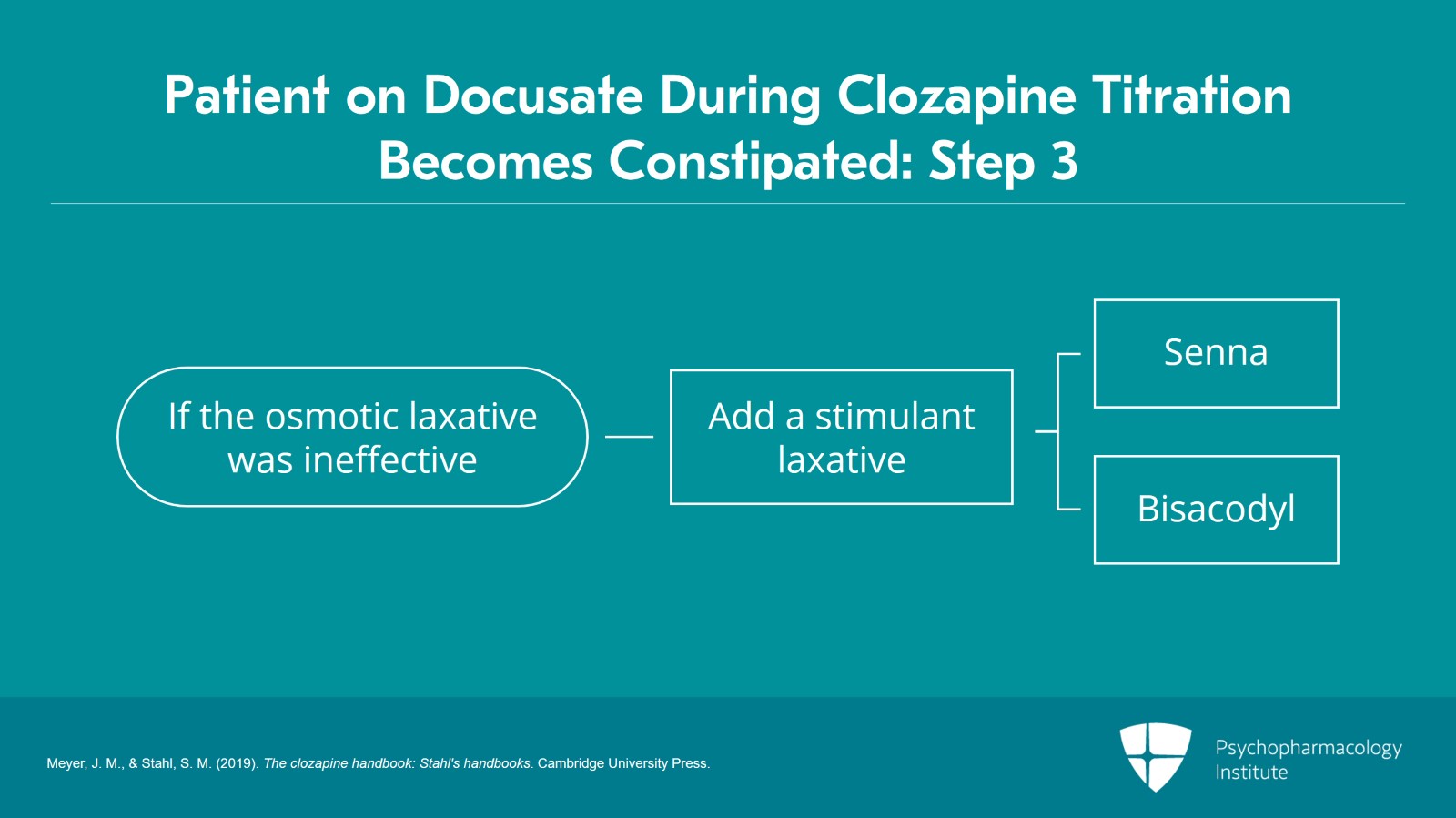
If that combination is ineffective, now we go to the stimulants. Your choices of stimulant laxatives are either senna or bisacodyl and those will be added and pushed up to the daily maximum dose. There used to be an old concern that the use of stimulant laxatives would harm the muscular tone of the colon. This is proven not to be true. Add this as step three.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 21
When a patient fails the combination of docusate plus an osmotic plus a stimulant the last step in constipation management of clozapine is using the newer secretagogues which have been available now for a number of years. The reason being is that if you end up taking the patient off clozapine you often have nothing else to offer them to manage their treatment-resistant illness.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
Slide 14 of 21
There are four secretagogues which are available worldwide. And I have some comments which I'll give in all four of these. You should give it with food and water and there are no drug interactions.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 21
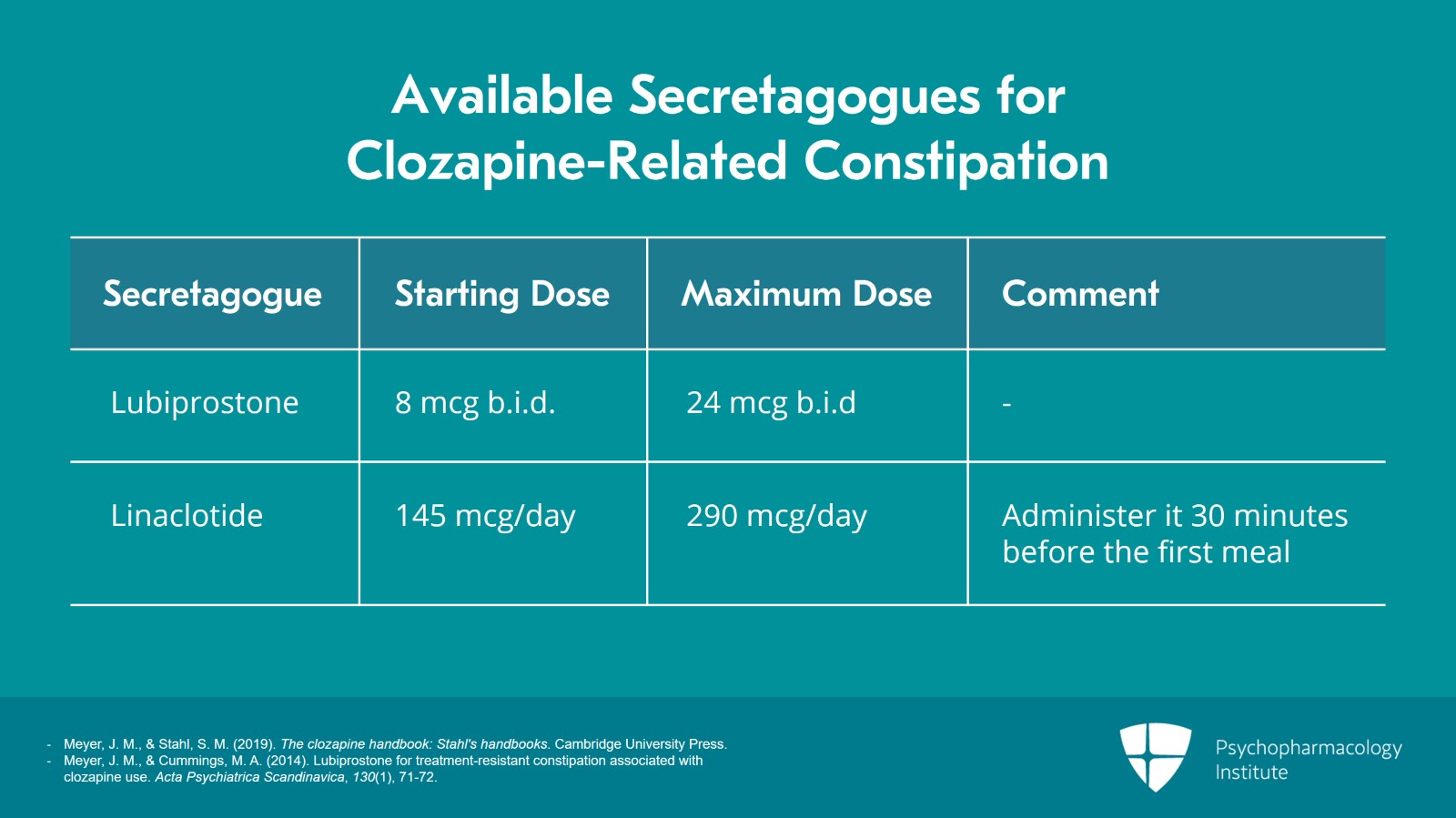
So here are the four secretagogues which are available worldwide. The first one is lubiprostone. Its mechanism of action is a prostaglandin E1 analogue. The starting dose is 8 mcg b.i.d. The maximum dose is 24 mcg b.i.d. The next one which became available is called linaclotide. This is a guanylate cyclase C agonist as its mechanism of action. The starting dose is 145 mcg daily. The maximum dose is 290 mcg daily. The only comment here is that it should be given more than 30 minutes before their first meal of the day.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
- Meyer, J. M., & Cummings, M. A. (2014). Lubiprostone for treatment-resistant constipation associated with clozapine use. Acta Psychiatrica Scandinavica, 130(1), 71-72.
Slide 16 of 21
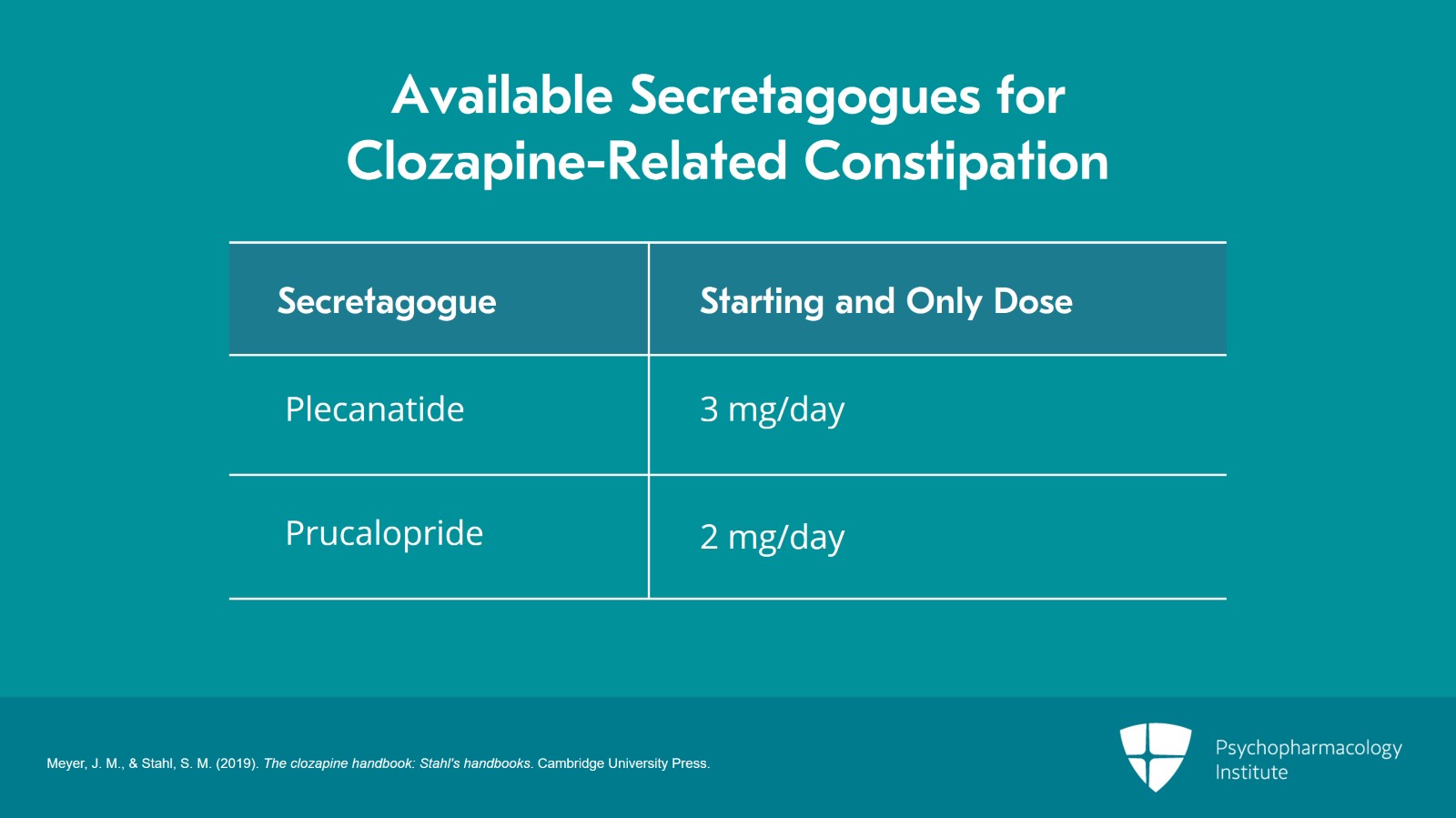
The next agent available in the US was called plecanatide. This is also a guanylate cyclase C agonist. The starting dose is 3 mg per day and it's the only dose, 3 mg per day. Easy to use. Give it a try. The last drug on the list is prucalopride. This has been available outside the US for more than a decade and there are case reports of people using it in Australia, in other places for clozapine-related constipation. Its mechanism is as a serotonin 4 agonist. The starting dose and the only dose out there is 2 mg.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 21
We have extensive experience at the California Department of State Hospitals with lubiprostone and linaclotide. Anecdotally, we find linaclotide might be a bit more effective and we've gravitated towards that as our preferred secretagogue. But most importantly, you must use these. Otherwise, you're going to end up having to take your patient off of clozapine and that's not a good outcome. Often, when we start the secretagogues, they are so effective we can actually remove some of the prior agents which have been added such as the stimulant and the osmotic.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
- Meyer, J. M., & Cummings, M. A. (2014). Lubiprostone for treatment-resistant constipation associated with clozapine use. Acta Psychiatrica Scandinavica, 130(1), 71-72.
Slide 18 of 21
And most importantly, at any step in this process if the patient experiences severe abdominal pain or certainly feculent vomitus, this is an emergency and they need to go to the ER.
References:
- Meyer, J. M., & Stahl, S. M. (2019). The clozapine handbook: Stahl's handbooks. Cambridge University Press.
- Nielsen, J., & Meyer, J. M. (2012). Risk factors for ileus in patients with schizophrenia. Schizophrenia Bulletin, 38(3), 592–598.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 21
The key point is that when treating constipation in patients on clozapine bulk-forming agents containing psyllium must be avoided. Everyone gets started on docusate.
Slide 20 of 21
After docusate, the next agents to add are an osmotic agent and then in step 3, a stimulant. Lastly, if the other three medication combination fails, learn to use the secretagogues.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.