Slides and Transcript
Slide 1 of 12
So in this next section, we’re going to discuss the differential diagnoses of explosive behavior and in particular we’re going to discuss the psychiatric conditions that can cause or contribute to explosive behavior. We’re then going to go more in depth into mood and anxiety disorders and disruptive behavior disorders and how explosive behavior may present in those conditions.
Slide 2 of 12
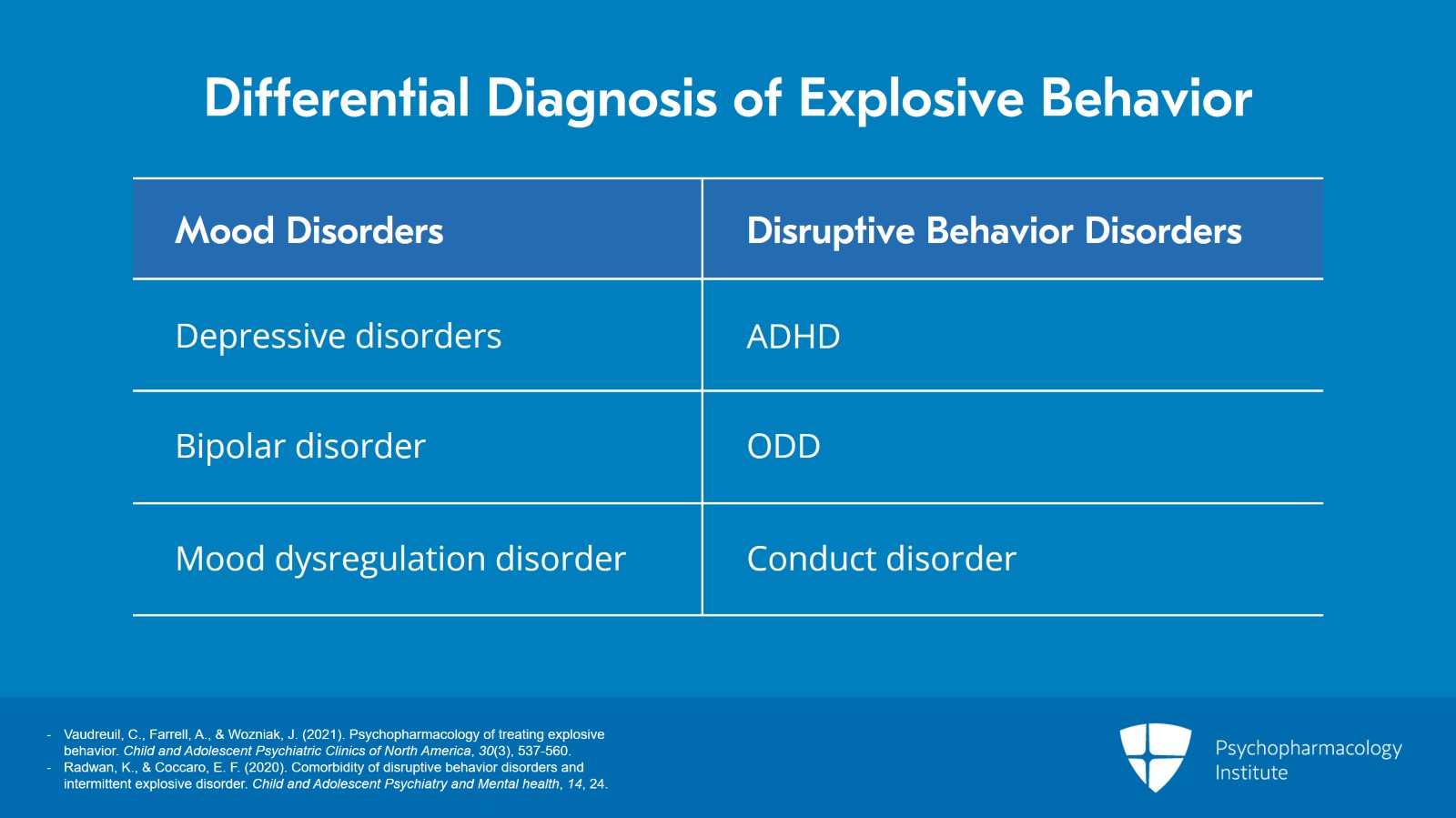
So the psychiatric differential diagnosis of explosive behavior is incredibly broad.
First, you want to consider mood disorders including depressive disorders, bipolar disorder, disruptive mood dysregulation disorder.
You want to consider all of the disruptive behavior disorders including ADHD, oppositional defiant disorder, and conduct disorder.
References:
- Vaudreuil, C., Farrell, A., & Wozniak, J. (2021). Psychopharmacology of treating explosive behavior. Child and Adolescent Psychiatric Clinics of North America, 30(3), 537-560.
- Radwan, K., & Coccaro, E. F. (2020). Comorbidity of disruptive behavior disorders and intermittent explosive disorder. Child and Adolescent Psychiatry and Mental health, 14, 24.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 12
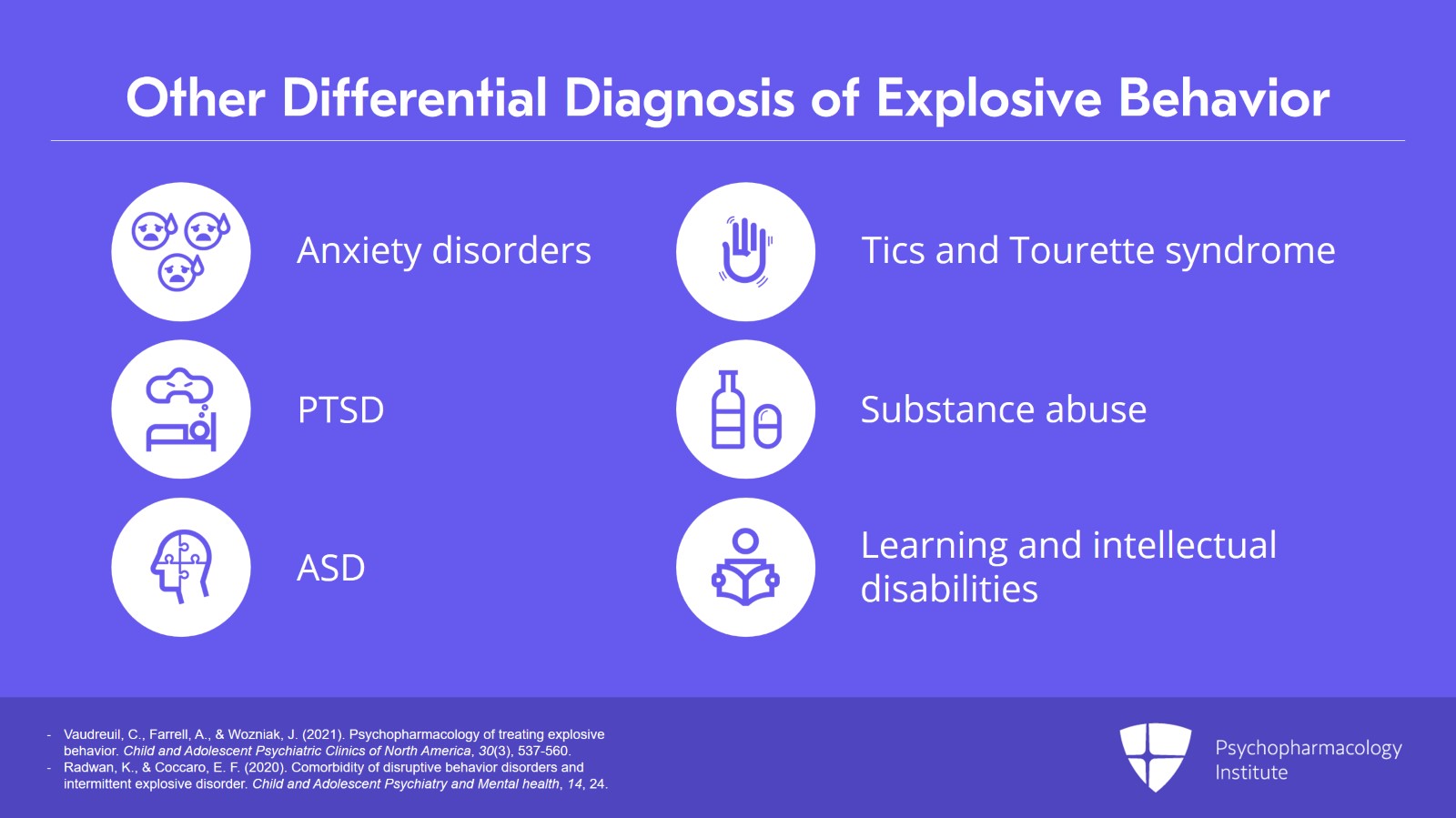
And then further, you need to consider anxiety disorders, PTSD, autism spectrum disorders, tics and Tourette syndrome, substance abuse, learning disabilities, and intellectual disability.
So, there’s a large number of psychiatric conditions that can present with explosive behavior.
References:
- Vaudreuil, C., Farrell, A., & Wozniak, J. (2021). Psychopharmacology of treating explosive behavior. Child and Adolescent Psychiatric Clinics of North America, 30(3), 537-560.
- Radwan, K., & Coccaro, E. F. (2020). Comorbidity of disruptive behavior disorders and intermittent explosive disorder. Child and Adolescent Psychiatry and Mental health, 14, 24.
Slide 4 of 12
The first thing we’re going to do is discuss mood and anxiety disorders. So how might you evaluate for whether or not a child who’s having explosive behavior may have an accompanying mood or anxiety disorder?
The first thing to look for is whether or not the child has a negative, abnormal, or mixed emotional state that persists outside of the explosive episodes.
References:
- Radwan, K., & Coccaro, E. F. (2020). Comorbidity of disruptive behavior disorders and intermittent explosive disorder. Child and Adolescent Psychiatry and Mental health, 14, 24.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 12
So for example, a child who has sad or depressed mood most of the time, a child who is irritable most of the time, a child who’s anxious most of the time, or a child who’s euphoric most of the time and this mood state seems different than their typical baseline and again this mood state persists outside of the explosive episodes.
If a child is exhibiting this, then you may want to consider a mood or anxiety disorder.
References:
- Radwan, K., & Coccaro, E. F. (2020). Comorbidity of disruptive behavior disorders and intermittent explosive disorder. Child and Adolescent Psychiatry and Mental health, 14, 24.
Slide 6 of 12
In addition, you would also look for any accompanying symptoms that might suggest a mood or anxiety disorder, for example, changes in sleep, changes in appetite, changes in energy, changes in functioning, and any excessive worries.
References:
- Radwan, K., & Coccaro, E. F. (2020). Comorbidity of disruptive behavior disorders and intermittent explosive disorder. Child and Adolescent Psychiatry and Mental health, 14, 24.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 12
In mood and anxiety disorders, explosive behavior is often triggered by a known cause. That known cause may still not warrant the explosive behavior. So for example, the explosion may seem out of proportion to what the trigger was but for example, something that might normally cause a little bit of irritability may cause a big explosion.
However, sometimes in mood and anxiety disorders, explosive behavior can also come out of nowhere or the triggering factor may not be readily apparent to the parents or adults or even the child in the situation.
References:
- Radwan, K., & Coccaro, E. F. (2020). Comorbidity of disruptive behavior disorders and intermittent explosive disorder. Child and Adolescent Psychiatry and Mental health, 14, 24.
Slide 8 of 12
Next on the differential diagnoses for explosive behavior are the disruptive behavior disorders which I mentioned previously include ADHD, oppositional defiant disorder, and conduct disorder.
Disruptive behavior disorders are often characterized by emotional impulsivity and deficient self-regulation.
So, when I talk about emotional impulsivity, what I mean is that these children are often described as going from 0 to 100 very quickly when becoming dysregulated.
Deficient self-regulation means that once the child is dysregulated they can’t calm themselves back down. So these characteristics have been well described in ADHD but can also be seen in oppositional defiant disorder and conduct disorder.
References:
- Radwan, K., & Coccaro, E. F. (2020). Comorbidity of disruptive behavior disorders and intermittent explosive disorder. Child and Adolescent Psychiatry and Mental health, 14, 24.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 12
In disruptive behavior disorders, emotional outbursts are typically triggered by something, often limit setting, restrictions around preferred activities. So for example, a common one that we see in clinic are children being told that they can’t play video games anymore, they have to get off the video game. Or an outburst may be triggered by being asked to engage in a nonpreferred activity such as getting ready for school or doing homework rather than playing with friends, playing video games, playing outside, etc.
References:
- Radwan, K., & Coccaro, E. F. (2020). Comorbidity of disruptive behavior disorders and intermittent explosive disorder. Child and Adolescent Psychiatry and Mental health, 14, 24.
Slide 10 of 12
In some scenarios, the explosions can be perceived by parents and caregivers as manipulative or that they’re used for the child to get something that they want or need. So for example, when a child is being told to do something they don’t want to do or being asked to stop doing something that they enjoy doing and the child has an explosion, a parent or caregiver may perceive that as a manipulative behavior.
Explosions are often out of proportion compared with what would be expected. We may see a large explosion that involves screaming, slamming doors, and sometimes throwing things or physical violence.
References:
- Radwan, K., & Coccaro, E. F. (2020). Comorbidity of disruptive behavior disorders and intermittent explosive disorder. Child and Adolescent Psychiatry and Mental health, 14, 24.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 12
The key points for this section are that:
1. In children with mood disorders, explosive behavior is often accompanied by changes in mood, sleep, appetite, energy, and functioning which should persist between explosive episodes.
2. In children with disruptive behavior disorders, explosive behavior often occurs in response to limit setting and may be perceived as manipulative by adults.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.