Slides and Transcript
Slide 1 of 25
Turning to video 3, diagnostic evaluation of psychotic symptoms in children and adolescents.
Slide 2 of 25
Psychotic symptoms in child and adolescent are a common and disruptive symptom of many psychiatric, neurodevelopmental, neurologic, and medical conditions. Psychotic symptoms are of course the hallmark feature of schizophrenia and are characterized by severe disruption in thought, reality testing.
References:
- Dulcan, M. K. (2016). Dulcan's textbook of child and adolescent psychiatry (2nd ed.). American Psychiatric Pub.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 25
And are divided in the two broad clusters, namely positive symptoms which include hallucinations, delusions, and disorganized thoughts and negative symptoms which include affective flattening, alogia, avolition, and anhedonia.
References:
- Dulcan, M. K. (2016). Dulcan's textbook of child and adolescent psychiatry (2nd ed.). American Psychiatric Pub.
Slide 4 of 25
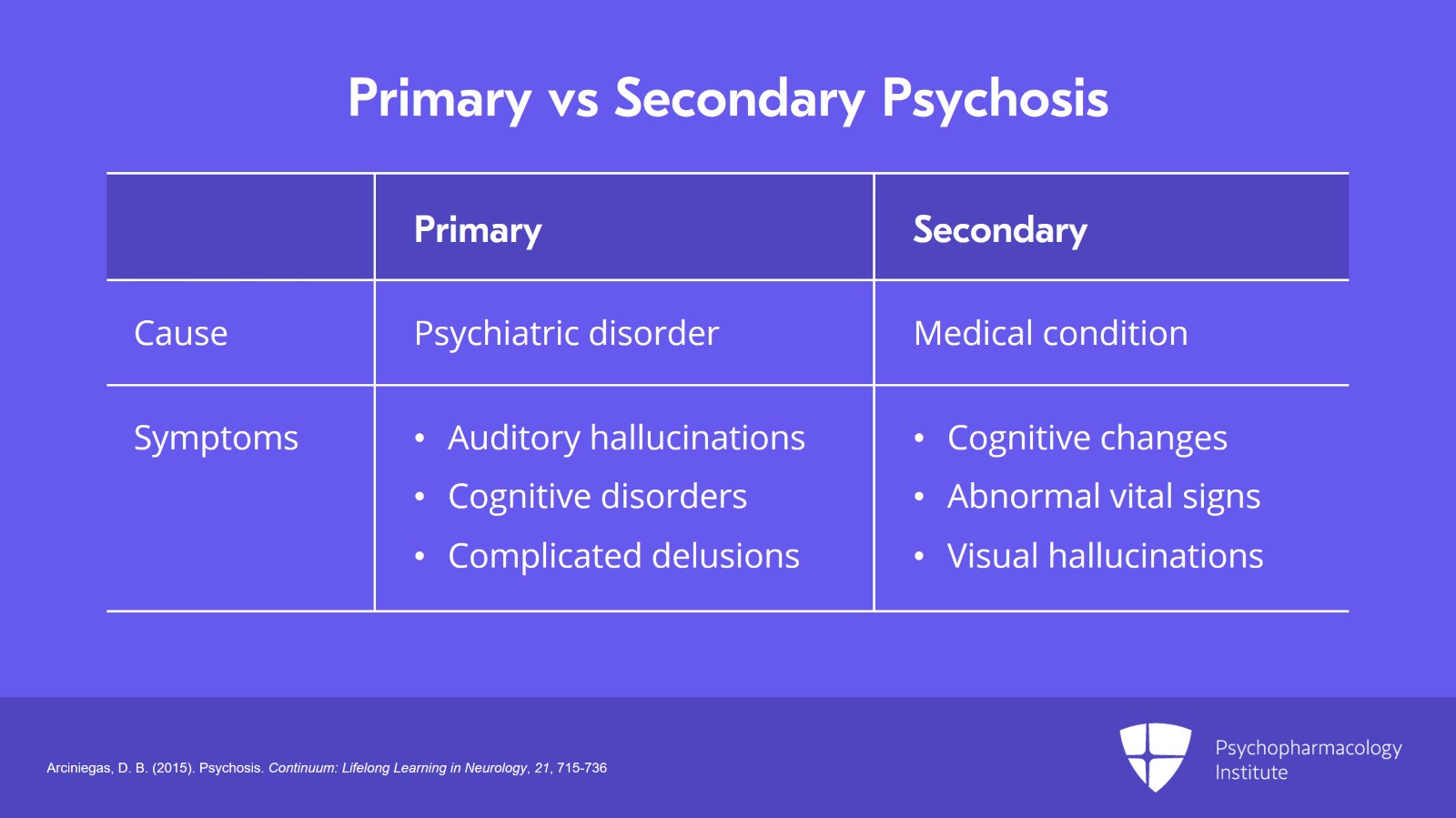
Primary versus secondary psychosis. Acute psychosis is considered primary if symptomatic of a psychiatric disorder, or secondary if it is caused by a specific medical condition such as a brain tumor or substance abuse. Patients with primary psychiatric disorders are likely to have auditory hallucinations, prominent cognitive disorders and complicated delusions. If the psychosis is caused by a medical condition, the patient may exhibit cognitive changes and abnormal vital signs and may have visual hallucinations. And again, I want you all to remember that when you see or are confronted with visual hallucinations think organic underlying medical condition until proven otherwise.
References:
- Arciniegas, D. B. (2015). Psychosis. Continuum: Lifelong Learning in Neurology, 21, 715-736.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 25
Illicit drug use is the most common medical cause of acute psychosis and we can see that with amphetamine use. We can see that with cannabis, cocaine, a whole host of illicit medications.
References:
- Arciniegas, D. B. (2015). Psychosis. Continuum: Lifelong Learning in Neurology, 21, 715-736.
Slide 6 of 25
Psychosis and magical thinking. This is very important and it has pronounced prognostic significance. Psychosis is defined as the presence of delusions, hallucinations without insight into the pathological nature, or both. Magical thinking in contrast is defined as a belief or quasi-belief or entertainment of the possibility that one's ideas, thoughts, actions, or words may somehow influence events which have no causal relationship with one another.
References:
- Arciniegas, D. B. (2015). Psychosis. Continuum: Lifelong Learning in Neurology, 21, 715-736.
- García-Montes, J. M., Pérez-Álvarez, M., Odriozola-González, P., Vallina-Fernández, O., & Perona-Garcelán, S. (2014). The role of magical thinking in hallucinations. Comparisons of clinical and non-clinical groups. Nordic Journal of Psychiatry, 68(8), 605-610.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 25
Adults with schizophrenia have a much stronger tendency for magical thinking than both adults with no psychiatric diagnoses as well as those who are diagnosed with another psychiatric diagnosis. Magical thinking is actually considered one of the most influential predictors of late development of schizophrenia and has been linked to the onset of visual and auditory hallucinations.
References:
- Arciniegas, D. B. (2015). Psychosis. Continuum: Lifelong Learning in Neurology, 21, 715-736.
- García-Montes, J. M., Pérez-Álvarez, M., Odriozola-González, P., Vallina-Fernández, O., & Perona-Garcelán, S. (2014). The role of magical thinking in hallucinations. Comparisons of clinical and non-clinical groups. Nordic Journal of Psychiatry, 68(8), 605-610.
Slide 8 of 25
How do we assess psychotic symptoms in children and adolescents? Well, I'll tell you it is more complicated than in adults so that evaluating youth with psychosis requires a very thorough assessment that includes a detailed patient history. If you're considering psychosis in a child or adolescent, by definition, you have to do a comprehensive medical, neurological examination to rule out confounding, complicating, contributing, causative factors, as well as observation of the patient and family over several visits to identify and rule out other contributing medical or psychiatric conditions or psychosocial stressors.
References:
- Skikic, M., & Arriola, J. A. (2020). First episode psychosis medical workup. Child and Adolescent Psychiatric Clinics of North America, 29(1), 15-28.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 25
The process needs to begin with careful consideration of differential diagnoses and be followed and supported by appropriate laboratory, encephalographic or EEG, and brain imaging studies. And it's essential for providers to know which clinical findings and elements of the history warrant additional testing.
References:
- Skikic, M., & Arriola, J. A. (2020). First episode psychosis medical workup. Child and Adolescent Psychiatric Clinics of North America, 29(1), 15-28.
Slide 10 of 25
Now, components of the diagnostic evaluation for psychotic symptoms include the comprehensive psychiatric history that focuses on the longitudinal characterization of the patient's current and past symptoms. Information from multiple sources here can be enormously helpful to improve the accuracy.
References:
- Dulcan, M. K. (2016). Dulcan's textbook of child and adolescent psychiatry (2nd ed.). American Psychiatric Pub.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 25
A comprehensive psychosocial history which includes academic, interpersonal functioning, in utero exposures.
References:
- Dulcan, M. K. (2016). Dulcan's textbook of child and adolescent psychiatry (2nd ed.). American Psychiatric Pub.
Slide 12 of 25
Familial psychiatric history, past exposure to trauma or neglect, and familial strengths and weaknesses.
References:
- Dulcan, M. K. (2016). Dulcan's textbook of child and adolescent psychiatry (2nd ed.). American Psychiatric Pub.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 25
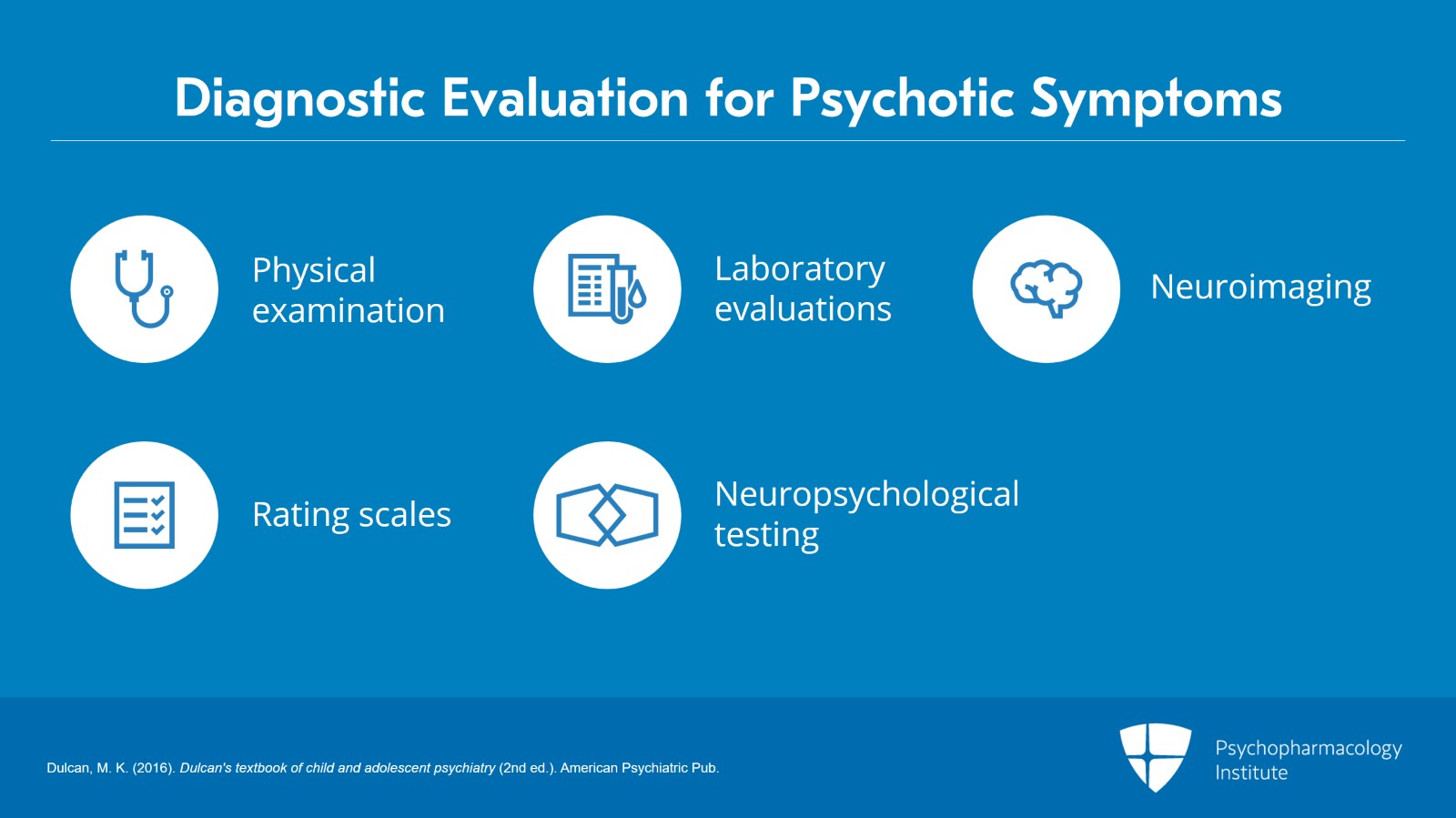
A comprehensive physical examination to rule out non-psychiatric medical conditions as a cause of psychosis; laboratory evaluations and neuroimaging as clinically indicated; standardized rating scales and, if warranted, neuropsychological testing can be very helpful to assess for learning and developmental disability, very common in psychosis, and offer insights into what academic supports might be most helpful and beneficial.
References:
- Dulcan, M. K. (2016). Dulcan's textbook of child and adolescent psychiatry (2nd ed.). American Psychiatric Pub.
Slide 14 of 25
Rating scales for assessing psychotic symptoms in children and adolescents. There are a few different symptom rating scales that are available to assist with determining symptom severity and these scores really only comprise a limited part of outcome measurement. They're more commonly used to create a standardized criteria of symptom remission for treatment studies used in various research studies.
References:
- Dulcan, M. K. (2016). Dulcan's textbook of child and adolescent psychiatry (2nd ed.). American Psychiatric Pub.
- Overall, J. E., & Gorham, D. R. (1962). The brief psychiatric rating scale. Psychological Reports, 10(3), 799-812.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 25
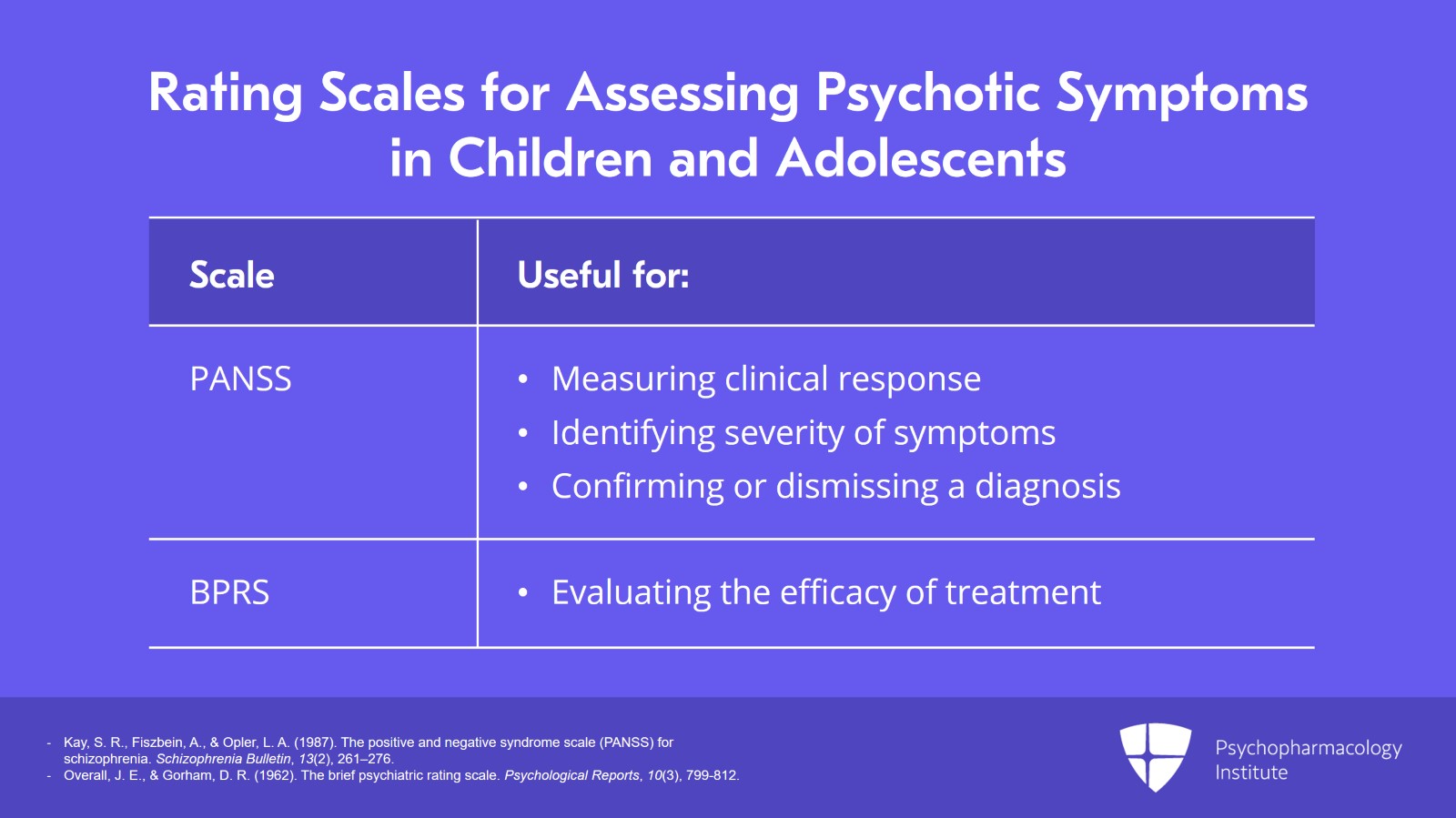
One of the most common is the Positive and Negative Syndrome Scale, the PANSS, which provides objective measurement of clinical response to pharmacologic treatments. The PANSS identifies the severity of positive symptoms and negative symptoms and can assist with confirming or dismissing a diagnosis of schizophrenia. The Brief Psychiatric Rating Scale, BPRS, is another tool used to assess the level of 18 symptom constructs such as hostility, suspiciousness, hallucination, grandiosity and that's also been used a lot in research. The BPRS is particularly useful in evaluating the efficacy or lack thereof in treatment in patients who have moderate to severe psychoses.
References:
- Kay, S. R., Fiszbein, A., & Opler, L. A. (1987). The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophrenia Bulletin, 13(2), 261–276.
- Overall, J. E., & Gorham, D. R. (1962). The brief psychiatric rating scale. Psychological Reports, 10(3), 799-812.
Slide 16 of 25
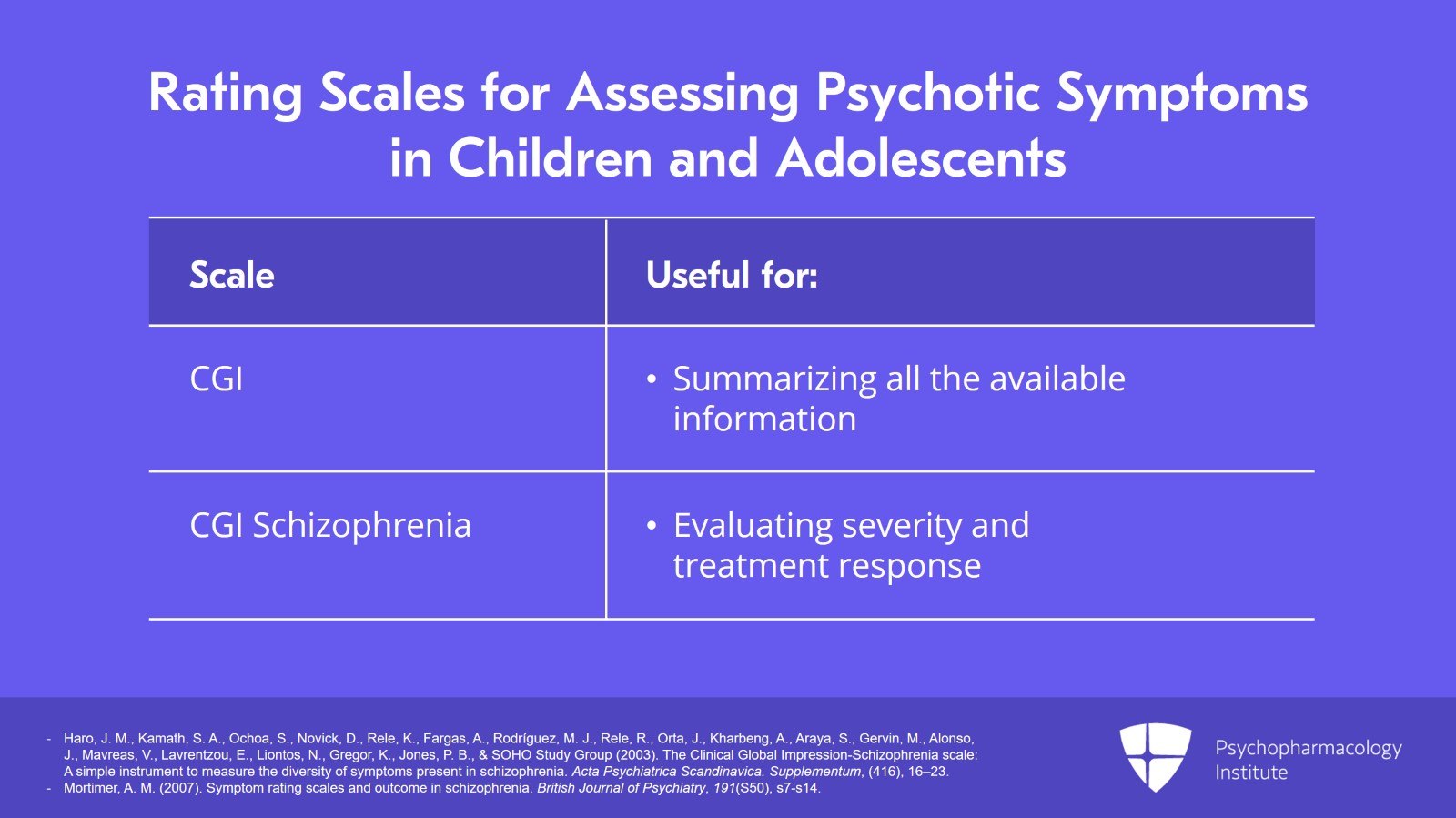
The Clinical Global Impression Scale and the Clinical Global Impression Schizophrenia Scale are two additional tools that clinicians often use. The CGI provides an overall clinician-determined summary measure that considers all the available information, that is patient's history, the psychosocial circumstances, the symptoms (present and past), the behavior and the impact of the symptoms on the patient's ability to function, while the CGI Schizophrenia evaluates severity and treatment response directly related to schizophrenia symptoms. Both instruments are simple. They're concise. They're quick and easy to administer which makes them appropriate for use in observational research studies and even in routine clinical practice.
References:
- Haro, J. M., Kamath, S. A., Ochoa, S., Novick, D., Rele, K., Fargas, A., Rodríguez, M. J., Rele, R., Orta, J., Kharbeng, A., Araya, S., Gervin, M., Alonso, J., Mavreas, V., Lavrentzou, E., Liontos, N., Gregor, K., Jones, P. B., & SOHO Study Group (2003). The Clinical Global Impression-Schizophrenia scale: A simple instrument to measure the diversity of symptoms present in schizophrenia. Acta Psychiatrica Scandinavica. Supplementum, (416), 16–23.
- Mortimer, A. M. (2007). Symptom rating scales and outcome in schizophrenia. British Journal of Psychiatry, 191(S50), s7-s14.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 25
The assessment of schizophrenia in children and adolescents. It's really vital that clinicians exercise extreme caution when evaluating youth for schizophrenia and I can't overemphasize this. I'm a practicing child and adolescent psychiatrist and I'm certainly not hesitant to make this diagnosis or any diagnosis when it's warranted but we have to be cautious, realize the limitations and as we talked about beforehand do a longitudinal assessment. Treatment of childhood-onset schizophrenia and early-onset schizophrenia requires the use of antipsychotic medications and we're talking about medicines that can be very helpful but also have significant side effect profiles and potentially significant long-term health risks.
References:
- McClellan, J., Stock, S., & American Academy of Child and Adolescent Psychiatry (AACAP) Committee on Quality Issues (CQI) (2013). Practice parameter for the assessment and treatment of children and adolescents with schizophrenia. Journal of the American Academy of Child and Adolescent Psychiatry, 52(9), 976–990.
Slide 18 of 25
Assessment in interview also requires consideration of the developmental context of the patient's cognitive and affective functioning and other possible psychiatric disorders such as concrete interpretation of questions in autism. Clinicians must not focus too narrowly on addressing psychotic symptoms and thereby fail to overlook common comorbidities.
References:
- McClellan, J., Stock, S., & American Academy of Child and Adolescent Psychiatry (AACAP) Committee on Quality Issues (CQI) (2013). Practice parameter for the assessment and treatment of children and adolescents with schizophrenia. Journal of the American Academy of Child and Adolescent Psychiatry, 52(9), 976–990.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 19 of 25
Now as many of you know, there are many, many other causes of psychotic symptoms. The psychiatric disorders can include psychotic disorder, bipolar disorder, unipolar major depression with psychosis, schizoaffective disorder, posttraumatic stress disorder, obsessive-compulsive disorder, autism spectrum disorder, non-psychotic emotional, and behavioral disorder. Various psychosocial factors and psychosocial stressors can lead to psychotic symptoms and those include abuse or neglect, traumatic stress, secondary gain for reporting symptoms, medical conditions such as substance intoxication, delirium, brain tumor, autoimmune encephalitis, head injury, endocrine abnormalities. Many, many causes.
References:
- Dulcan, M. K. (2016). Dulcan's textbook of child and adolescent psychiatry (2nd ed.). American Psychiatric Pub.
Slide 20 of 25
Other mental disorders can also mask schizophrenia symptoms. So, we know that 50% to 75% of patients with schizophrenia have one or more comorbid psychiatric disorders.
References:
- Sadock, B., Sadock, V. A., & Ruiz, P. (2016). Kaplan & Sadock's concise textbook of clinical psychiatry. Lippincott Williams & Wilkins.
- Weber, N. S., Cowan, D. N., Millikan, A. M., & Niebuhr, D. W. (2009). Psychiatric and general medical conditions comorbid with schizophrenia in the national hospital discharge survey. Psychiatric Services, 60(8), 1059-1067.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 21 of 25
And the most common psychiatric comorbidities include ADHD, oppositional defiant disorder, anxiety and mood disorders as well as substance use disorders in adolescents.
References:
- Sadock, B., Sadock, V. A., & Ruiz, P. (2016). Kaplan & Sadock's concise textbook of clinical psychiatry. Lippincott Williams & Wilkins.
- Weber, N. S., Cowan, D. N., Millikan, A. M., & Niebuhr, D. W. (2009). Psychiatric and general medical conditions comorbid with schizophrenia in the national hospital discharge survey. Psychiatric Services, 60(8), 1059-1067.
Slide 22 of 25
Key point number one. It's really vital that clinicians exercise extreme caution when evaluating youth for schizophrenia and you must consider the developmental context of the patient's cognitive and affective functioning.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 23 of 25
Magical thinking is considered one of the most influential predictors of later development of schizophrenia. Fifty to seventy-five percent of patients with schizophrenia have one or more comorbid psychiatric disorder.
Slide 24 of 25
The most common psychiatric comorbidities of schizophrenia are ADHD, oppositional defiant disorder, anxiety, mood disorders, and substance use disorders in adolescents.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.