Slides and Transcript
Slide 1 of 15
Let’s turn to video 4, Pediatric OCD Comorbidity with Depression, Anxiety Disorders, and ASD, Autism Spectrum Disorders.
Slide 2 of 15
This is critically important and one thing that I might mention is that some of the early, earlier pharmaceutical studies of obsessive-compulsive disorder, one of the criticisms was that for entry into some of those studies there had to be what was called clean obsessive-compulsive disorder, limited comorbidity and other restrictions.
And the criticism was that in the real-world OCD is a heavily comorbid psychiatric disorder.
Let’s go over some of these comorbidities.
References:
- Geller, D. A. (2006). Obsessive-compulsive and spectrum disorders in children and adolescents. Psychiatric Clinics of North America, 29(2), 353-370.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 15
One common comorbidity is generalized anxiety disorder, GAD for short.
And differentiating obsessions, compulsions, OCD from pathological worry that you see in generalized anxiety disorder is often more diffuse.
In generalized anxiety disorder, there are many more issues and concerns that require reassurance, whereas we talked with obsessive-compulsive disorder there’s more of a laser focus on one really concerning item that you need repeated reassurance for.
Generalized anxiety disorder involves excessive worry about real-life concerns, excessive worry about an upcoming test. OCD, on the other hand, centers on unrealistic and irrational fears beyond the scope of daily life problems.
References:
- Comer, J. S., Kendall, P. C., Franklin, M. E., Hudson, J. L., & Pimentel, S. S. (2004). Obsessing/worrying about the overlap between obsessive–compulsive disorder and generalized anxiety disorder in youth. Clinical Psychology Review, 24(6), 663-683.
Slide 4 of 15
And to make it even more complex, sometimes GAD and OCD can coexist and that is why there is a requirement to really tease out these complicated conditions that there be a trained mental health professional who does the assessment, particularly when interventions such as medication are considered.
Now, one of the things that we’re going to have to monitor very closely is what is the impact of COVID-19, wearing masks, people wearing gloves and a legitimate concern about a pandemic and becoming infected. Again, that goes in terms of that differential in terms of what is the pathological involvement, what is the dysfunction.
References:
- Comer, J. S., Kendall, P. C., Franklin, M. E., Hudson, J. L., & Pimentel, S. S. (2004). Obsessing/worrying about the overlap between obsessive–compulsive disorder and generalized anxiety disorder in youth. Clinical Psychology Review, 24(6), 663-683.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 15
The differential with mood disorder is complicated because depression is often comorbid with OCD. As we mentioned, 1/3 of patients with OCD will have depression at the time of their diagnosis and 2/3 will develop depression during their lifetime.
Comorbid depression is associated with increased OCD symptom severity and increased functional impairment.
References:
- Grant, J. E. (2014). Obsessive–compulsive disorder. New England Journal of Medicine, 371(7), 646-653.
Slide 6 of 15
So it’s critically important to determine whether depressive symptoms are primary, that is a separate condition from OCD, versus secondary, occurring in response to the stress caused by OCD to guide treatment decisions.
Mood disorders, if primary, the treatment of choice is to begin medication and/or cognitive behavioral therapy, CBT for short, treating and targeting depression.
If the mood disorder is secondary, using exposure and response prevention called ERP can lead to a decrease in comorbid depression as well as the obsessions and compulsions.
References:
- Canavera, K. E., Ollendick, T. H., Ehrenreich May, J. T., & Pincus, D. B. (2010). Clinical correlates of comorbid obsessive–compulsive disorder and depression in youth. Child Psychiatry & Human Development, 41(6), 583-594.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 15
Clinicians need to assess the content of depressive cognitions to determine whether they center on impairment and quality of life issues related to OCD.
It’s also very important to obtain a timeline of symptoms, did the depressive symptoms precede OCD or did they begin after the OCD started, to identify if depression is secondary to OCD or is in fact a distinct condition.
References:
- Canavera, K. E., Ollendick, T. H., Ehrenreich May, J. T., & Pincus, D. B. (2010). Clinical correlates of comorbid obsessive–compulsive disorder and depression in youth. Child Psychiatry & Human Development, 41(6), 583-594.
Slide 8 of 15
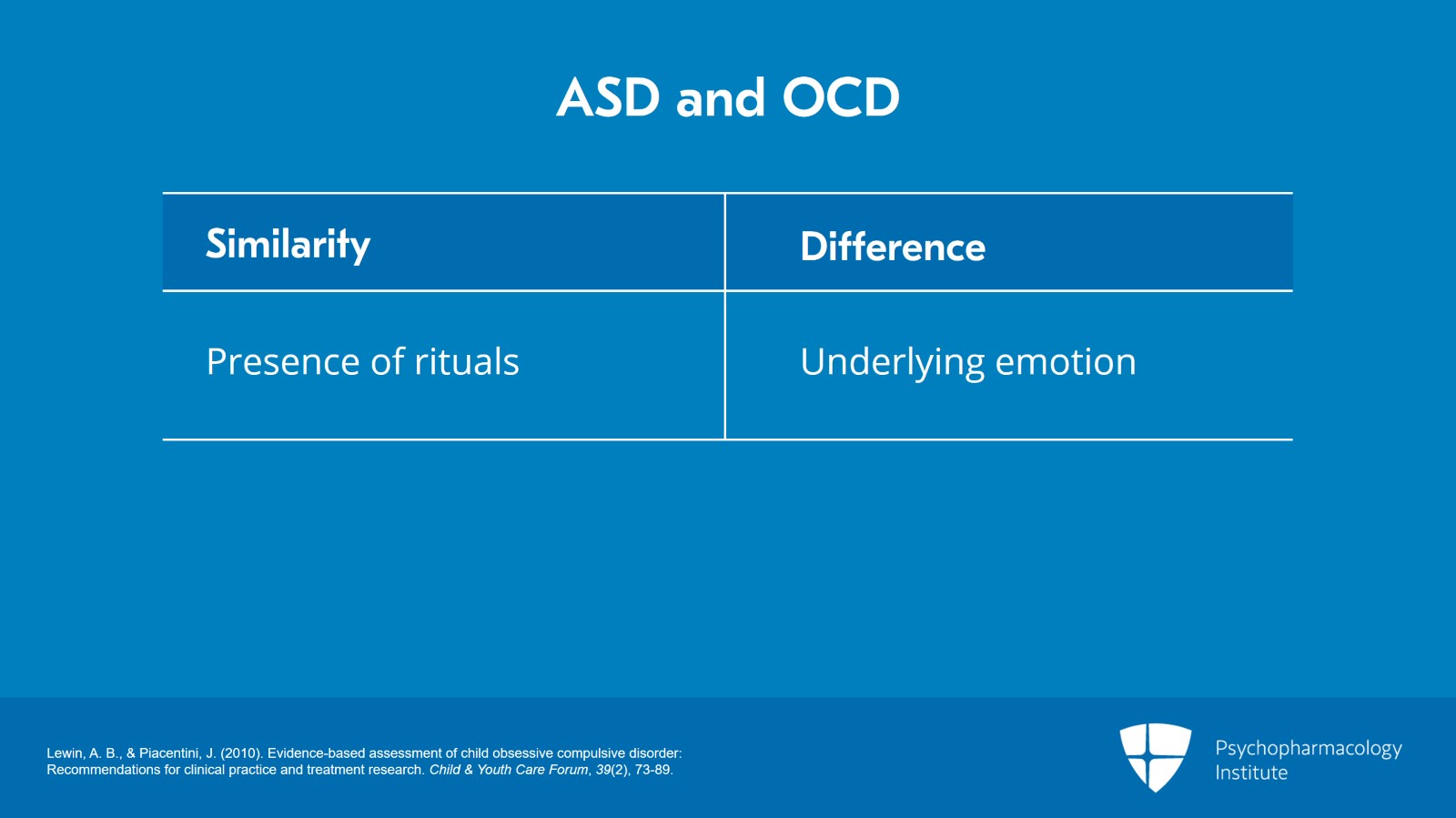
Autism spectrum disorders. Both OCD and autism spectrum disorder will have rituals it’s a hallmark of both conditions, but the underlying emotion can distinguish these two.
References:
- Lewin, A. B., & Piacentini, J. (2010). Evidence-based assessment of child obsessive compulsive disorder: Recommendations for clinical practice and treatment research. Child & Youth Care Forum, 39(2), 73-89.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 15
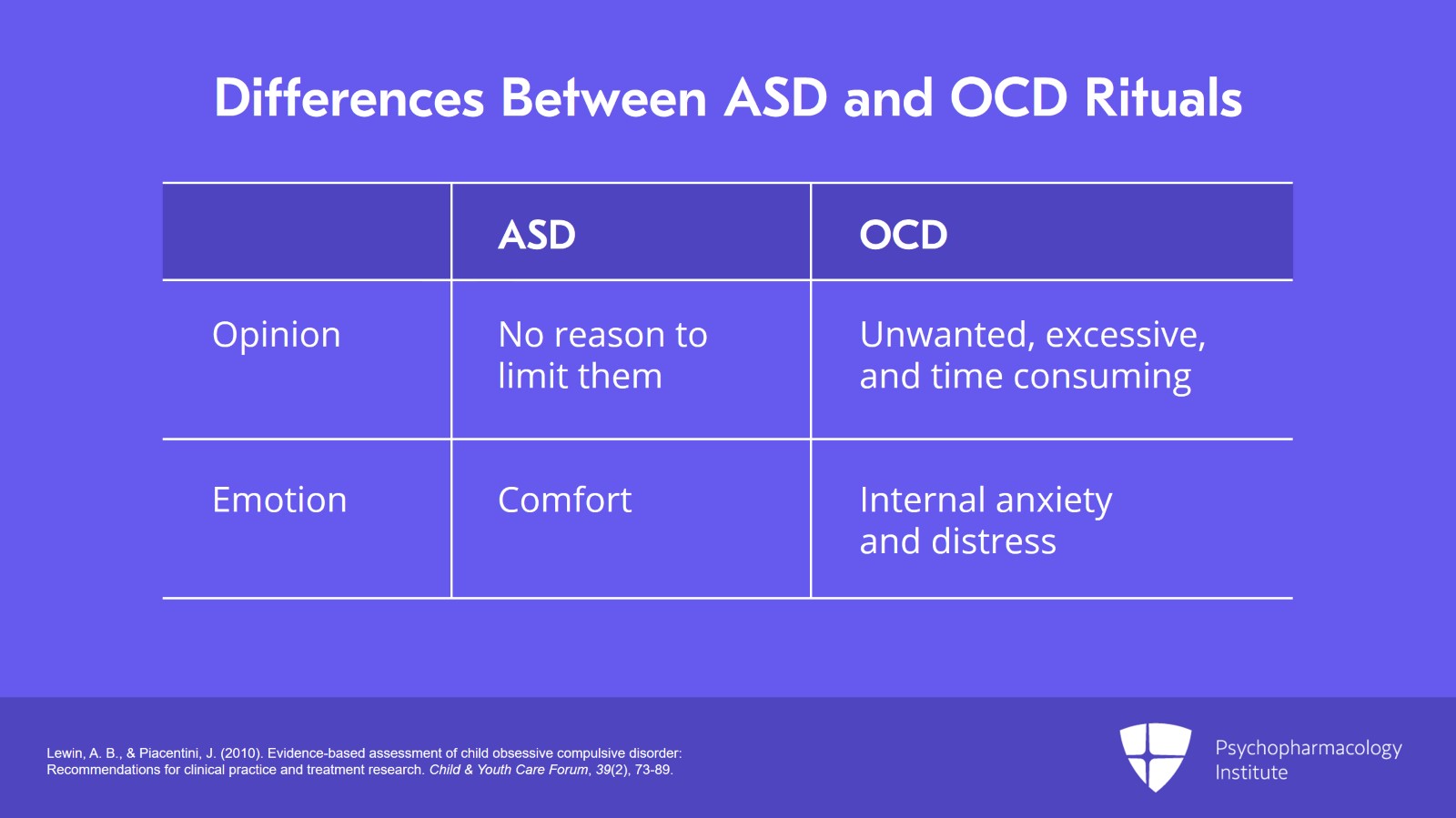
In ASD, autism spectrum disorder, the child actually enjoys the rituals and sees no reason to limit or stop them. They’re comforting.
Whereas, the compulsive behaviors and rituals associated with OCD are more frequently associated with internal anxiety and distress and the rituals may be recognized as being unwanted, excessive, and time consuming.
References:
- Lewin, A. B., & Piacentini, J. (2010). Evidence-based assessment of child obsessive compulsive disorder: Recommendations for clinical practice and treatment research. Child & Youth Care Forum, 39(2), 73-89.
Slide 10 of 15
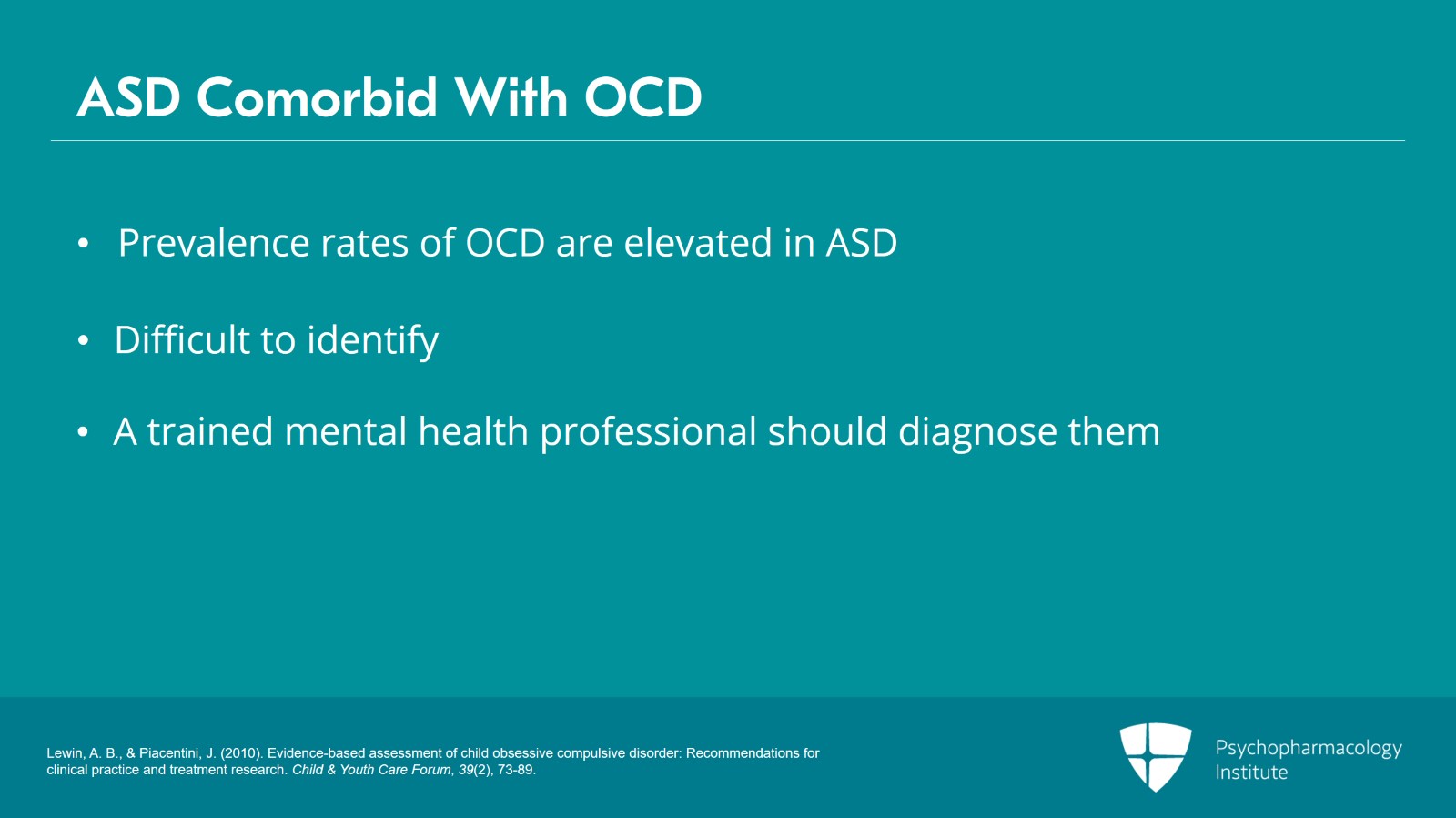
Prevalence rates of OCD are significantly elevated among autism spectrum disorder individuals.
Comorbidity of OCD in children with autism can be difficult to identify and that’s why it’s so critically important that a trained, experienced mental health professional diagnose these conditions particularly when treatment, medication, intervention is indicated.
References:
- Lewin, A. B., & Piacentini, J. (2010). Evidence-based assessment of child obsessive compulsive disorder: Recommendations for clinical practice and treatment research. Child & Youth Care Forum, 39(2), 73-89.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 15
So, treatment plan in patients with comorbid autism spectrum disorder and OCD.
OCD and ASD share many similar symptoms but the processes that underlie these symptoms can require different treatment approaches.
Treatment for OCD-based compulsions has to be targeted toward controlling the thought process and fears that cause the compulsions. For example, therapists may use exposure and response prevention interventions aimed at reducing anxiety in OCD patients.
On the other hand, with autism spectrum disorder, anxiety typically arises from impulsivity, overstimulation, or misunderstanding of social cues. Therefore, treatment of ASD-related symptoms has to be targeted toward treating the sudden burst of anger which stem from this anxiety by using techniques such as anger management, desensitization training, and parent management techniques.
References:
- Lewin, A. B., & Piacentini, J. (2010). Evidence-based assessment of child obsessive compulsive disorder: Recommendations for clinical practice and treatment research. Child & Youth Care Forum, 39(2), 73-89.
Slide 12 of 15
The key take-home points are the following. Generalized anxiety disorder, mood disorders and/or autism spectrum disorders are often comorbid with OCD.
Comorbid depression is associated with increased OCD symptom severity and increased functional impairment.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 15
And it’s critically important to determine whether depressive symptoms are primary, that is separate from OCD, versus secondary, that is occurring in response to the stress caused by OCD.
The prevalence of OCD is significantly elevated among autism spectrum disorder individuals.
Slide 14 of 15
OCD symptoms can often be difficult to identify from ASD due to an overlap in repetitive behaviors and rituals in both disorders.
The major point of distinction is the underlying emotion associated with rituals.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.