Slides and Transcript
Slide 2 of 16
As I mentioned in the previous video, cannabis use is higher in persons who have a psychiatric diagnosis. This includes a wide range of disorders from mood and anxiety disorders to psychosis and personality disorders. This raises the question: Does cannabis cause mental illness in people who use it?
References:
- Lowe, D. J., Sasiadek, J. D., Coles, A. S., & George, T. P. (2018). Cannabis and mental illness: A review. European Archives of Psychiatry and Clinical Neuroscience, 269(1), 107-120.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 16
I'll refer again to the 2017 National Academy of Sciences report and this report found moderate evidence for the following associations. There was an association between regular cannabis use and an increased incidence of social anxiety disorder. There was a small but increased risk for the development of depression in cannabis users. And there was an increase in suicidal ideation and attempts with a higher incidence in heavy users. And they found an increase in the incidence of suicide completion. This report also found limited evidence of an association between cannabis use and the development of bipolar disorder in regular or daily users and an association between cannabis use and the development of other types of anxiety disorders besides a social anxiety disorder.
References:
- Lowe, D. J., Sasiadek, J. D., Coles, A. S., & George, T. P. (2018). Cannabis and mental illness: A review. European Archives of Psychiatry and Clinical Neuroscience, 269(1), 107-120.
- National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Population Health and Public Health Practice, & Committee on the Health Effects of Marijuana: An Evidence Review and Research Agenda. (2017). The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. National Academies Press (US).
- Walsh, Z., Gonzalez, R., Crosby, K., S. Thiessen, M., Carroll, C., & Bonn-Miller, M. O. (2017). Medical cannabis and mental health: A guided systematic review. Clinical Psychology Review, 51, 15-29.
Slide 4 of 16
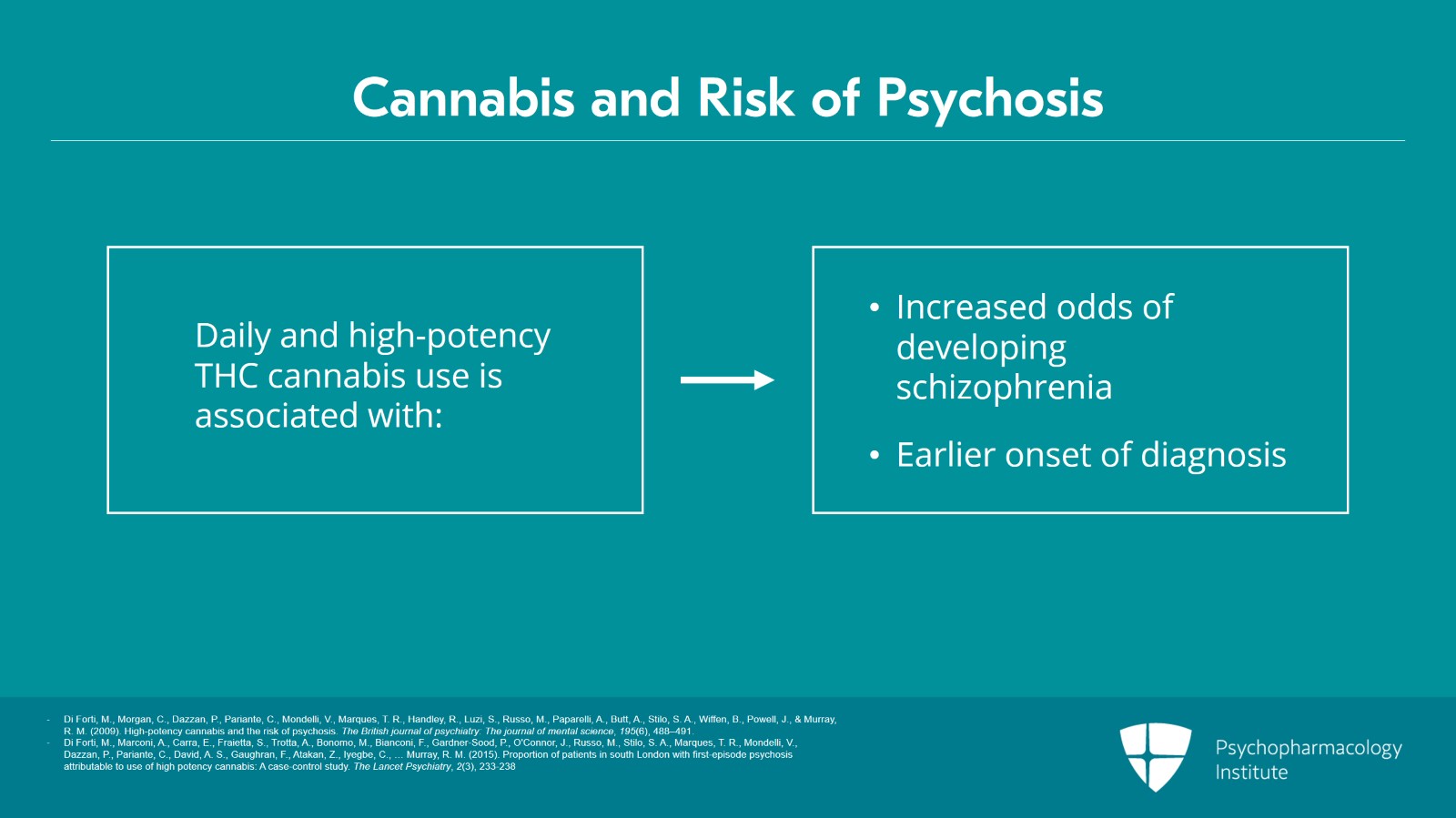
Now when it comes to cannabis and psychosis studies show that daily and/or high potency THC cannabis use, especially in adolescents, is associated with increased odds of developing schizophrenia. Additional studies have shown that daily and high-potency cannabis use increases the risk of an earlier onset of diagnosis.
References:
- Di Forti, M., Morgan, C., Dazzan, P., Pariante, C., Mondelli, V., Marques, T. R., Handley, R., Luzi, S., Russo, M., Paparelli, A., Butt, A., Stilo, S. A., Wiffen, B., Powell, J., & Murray, R. M. (2009). High-potency cannabis and the risk of psychosis. The British journal of psychiatry: The journal of mental science, 195(6), 488–491.
- Di Forti, M., Marconi, A., Carra, E., Fraietta, S., Trotta, A., Bonomo, M., Bianconi, F., Gardner-Sood, P., O'Connor, J., Russo, M., Stilo, S. A., Marques, T. R., Mondelli, V., Dazzan, P., Pariante, C., David, A. S., Gaughran, F., Atakan, Z., Iyegbe, C., … Murray, R. M. (2015). Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: A case-control study. The Lancet Psychiatry, 2(3), 233-238
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 16
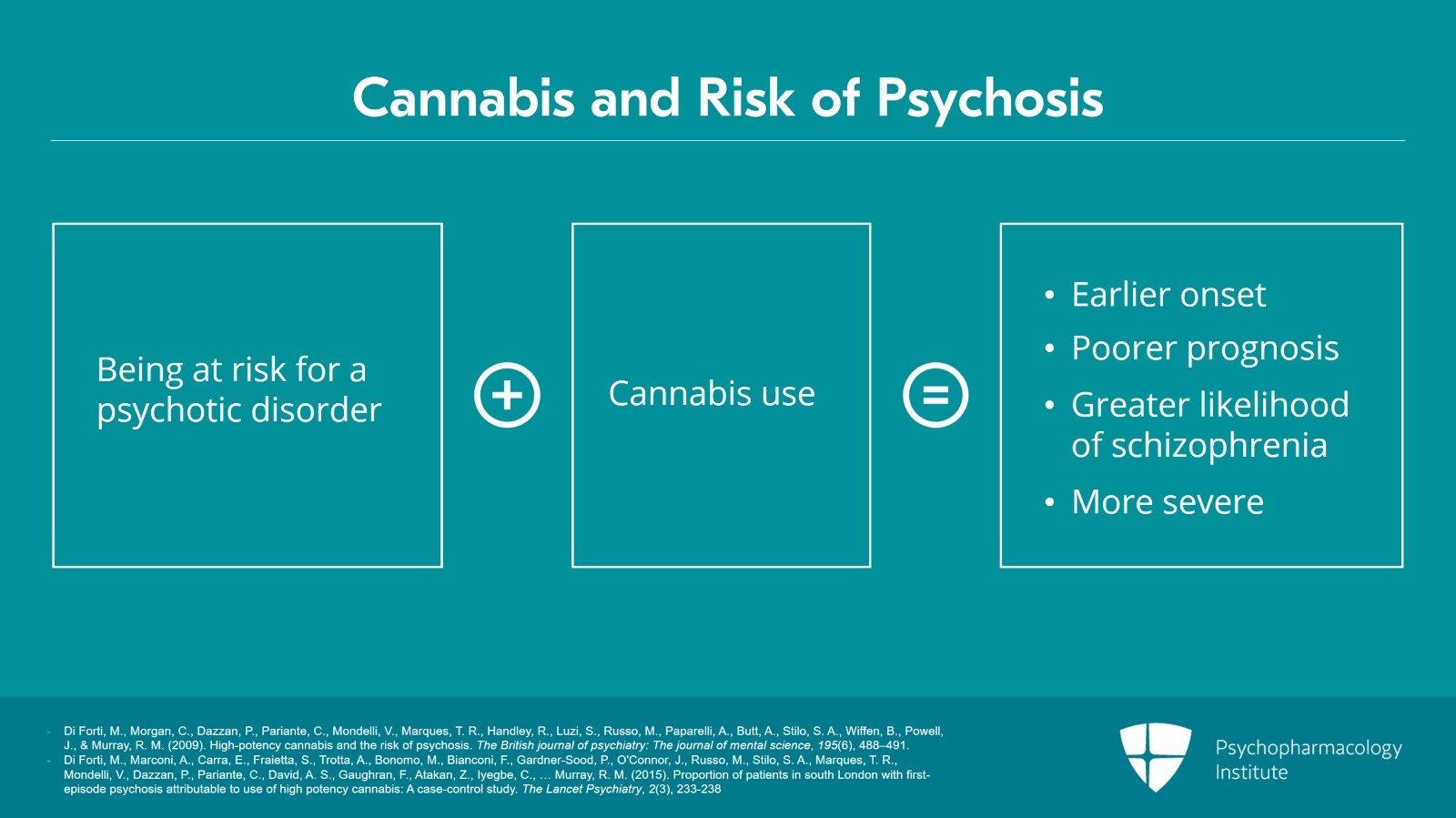
Overall, these studies show that being at risk for a psychotic disorder combined with cannabis use is more likely to be associated with an earlier onset of psychosis, a poorer prognosis and a greater likelihood of being diagnosed with schizophrenia. It's possible that persons with a vulnerability to psychosis who use high-potency cannabis on a regular basis are more likely to develop a more severe psychotic disease.
References:
- Di Forti, M., Morgan, C., Dazzan, P., Pariante, C., Mondelli, V., Marques, T. R., Handley, R., Luzi, S., Russo, M., Paparelli, A., Butt, A., Stilo, S. A., Wiffen, B., Powell, J., & Murray, R. M. (2009). High-potency cannabis and the risk of psychosis. The British journal of psychiatry: The journal of mental science, 195(6), 488–491.
- Di Forti, M., Marconi, A., Carra, E., Fraietta, S., Trotta, A., Bonomo, M., Bianconi, F., Gardner-Sood, P., O'Connor, J., Russo, M., Stilo, S. A., Marques, T. R., Mondelli, V., Dazzan, P., Pariante, C., David, A. S., Gaughran, F., Atakan, Z., Iyegbe, C., … Murray, R. M. (2015). Proportion of patients in south London with first-episode psychosis attributable to use of high potency cannabis: A case-control study. The Lancet Psychiatry, 2(3), 233-238
Slide 6 of 16
But can we say that cannabis use itself causes schizophrenia? While there is a strong association between cannabis use and the development of schizophrenia, it's difficult to show causal relationship. Certainly, the majority of people who use cannabis do not develop schizophrenia.
References:
- Haney, M., & Evins, A. E. (2015). Does cannabis cause, exacerbate or ameliorate psychiatric disorders? An oversimplified debate discussed. Neuropsychopharmacology, 41(2), 393-401.
- Dumas, P., Saoud, M., Bouafia, S., Gutknecht, C., Ecochard, R., Daléry, J., Rochet, T., & D'Amato, T. (2002). Cannabis use correlates with schizotypal personality traits in healthy students. Psychiatry Research, 109(1), 27-35.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 16
However, patients who are developing schizophrenia are more likely to start using cannabis to address symptoms like anxiety and social isolation. For example, studies also show that tobacco has a similar relationship to psychosis.
References:
- Haney, M., & Evins, A. E. (2015). Does cannabis cause, exacerbate or ameliorate psychiatric disorders? An oversimplified debate discussed. Neuropsychopharmacology, 41(2), 393-401.
- Dumas, P., Saoud, M., Bouafia, S., Gutknecht, C., Ecochard, R., Daléry, J., Rochet, T., & D'Amato, T. (2002). Cannabis use correlates with schizotypal personality traits in healthy students. Psychiatry Research, 109(1), 27-35.
Slide 8 of 16
Cannabis use in individuals who are at risk for psychotic disorder should be addressed clinically. This should include an understanding of the patient's reasons for using cannabis. It should not include judgment nor punishment.
References:
- Haney, M., & Evins, A. E. (2015). Does cannabis cause, exacerbate or ameliorate psychiatric disorders? An oversimplified debate discussed. Neuropsychopharmacology, 41(2), 393-401.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 16
So, in summary, cannabis use associated with the development of a psychiatric disorder? We can say that cannabis use might increase the risk of developing depression, anxiety, bipolar disorder and psychosis including schizophrenia. However, the data shows an association between use and the development of a psychiatric disorder, not a causal relationship.
References:
- Lowe, D. J., Sasiadek, J. D., Coles, A. S., & George, T. P. (2018). Cannabis and mental illness: A review. European Archives of Psychiatry and Clinical Neuroscience, 269(1), 107-120.
- National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Population Health and Public Health Practice, & Committee on the Health Effects of Marijuana: An Evidence Review and Research Agenda. (2017). The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. National Academies Press (US).
- Walsh, Z., Gonzalez, R., Crosby, K., S. Thiessen, M., Carroll, C., & Bonn-Miller, M. O. (2017). Medical cannabis and mental health: A guided systematic review. Clinical Psychology Review, 51, 15-29.
Slide 10 of 16
It's important to recognize that cannabis use, especially heavy use, is associated with an increased risk of suicide. However, this increased risk is not necessarily specific to cannabis over other types of drugs. In the United States, 22% of suicides involved alcohol, 20% involved opioids, 10% involved cannabis, 5% involved cocaine and 3% involved amphetamines.
References:
- Centers for Disease Control and Prevention. (n.d.). Injury Prevention and Control. http://www.cdc.gov/Features/PreventingSuicide/ index.html.
- National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Population Health and Public Health Practice, & Committee on the Health Effects of Marijuana: An Evidence Review and Research Agenda. (2017). The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. National Academies Press (US).
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 16
Thus, even though we don't often think about the association between cannabis and suicide, it should be considered in heavy users along with other types of drug use.
References:
- National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Population Health and Public Health Practice, & Committee on the Health Effects of Marijuana: An Evidence Review and Research Agenda. (2017). The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. National Academies Press (US).
Slide 12 of 16
So, the key points here are that cannabis use is prevalent among patients with psychiatric disorders raising the concern that cannabis use might lead to the development of a mental illness.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 16
Research indicates that the combination of heavy cannabis use and being at risk for having a psychotic disorder is more likely to be associated with an earlier onset of psychosis, a worse prognosis and a greater likelihood of being diagnosed with schizophrenia.
Slide 14 of 16
Studies show an association between cannabis use and social anxiety disorder. There is evidence of an association between heavy cannabis use and suicidal thoughts and suicide completion. However, it should be noted that these studies show an association and don't show that cannabis alone causes these disorders.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 16
While this is not specific to cannabis over other types of drugs, it shows that practitioners should be concerned about suicidal impulses in patients with heavy drug use.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.