Slides and Transcript
Slide 1 of 18
Hi everybody. This is Dr. David Osser and I'm presenting video 6 of major depression with psychotic features psychopharmacology algorithm.
Slide 2 of 18
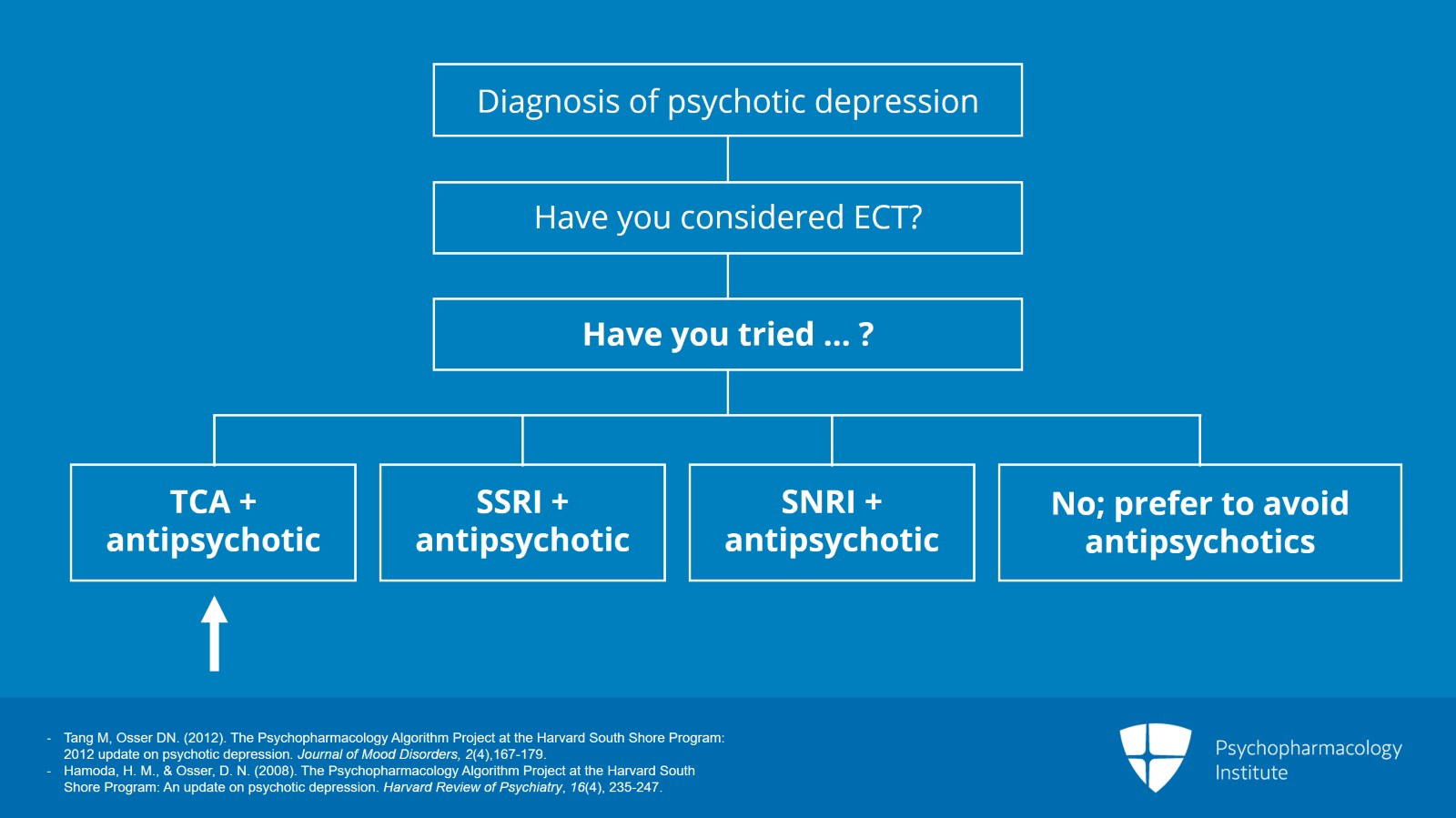
And in the first 5 videos, you have heard about diagnosis of psychotic depression, considering ECT for the first treatment and then considering our first medication choice for treating it which involves an antidepressant and an antipsychotic. And we've spent a lot of time discussing which antidepressant you might prefer and we settled on an SNRI. But now, we're going to talk about what antipsychotic to choose in this video.
References:
- Tang M, Osser DN. (2012). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: 2012 update on psychotic depression. Journal of Mood Disorders, 2(4),167-179.
- Hamoda, H. M., & Osser, D. N. (2008). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: An update on psychotic depression. Harvard Review of Psychiatry, 16(4), 235-247.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 18
Well, it turns out that the evidence base is just not very informative. There have been no direct comparisons to test the relative efficacy and safety of different antipsychotics. We have extensive study with olanzapine as the antipsychotic and a fair amount with quetiapine. In relatively recent randomized trials, they both are effective choices for combination therapy, but they have issues with side effects.
References:
- Tang M, Osser DN. (2012). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: 2012 update on psychotic depression. Journal of Mood Disorders, 2(4),167-179.
- Hamoda, H. M., & Osser, D. N. (2008). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: An update on psychotic depression. Harvard Review of Psychiatry, 16(4), 235-247.
Slide 4 of 18
But as far as their results in the studies, quetiapine had more efficacy than olanzapine and other atypical antipsychotics for some other delusional or other depressive disorders like bipolar depression. And aripiprazole augments SSRIs in major nonpsychotic depression. So given those facts about quetiapine and aripiprazole, we think that you should consider favoring quetiapine because of possible broader spectrum of benefit and possibly aripiprazole as well.
References:
- Tang M, Osser DN. (2012). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: 2012 update on psychotic depression. Journal of Mood Disorders, 2(4),167-179.
- Hamoda, H. M., & Osser, D. N. (2008). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: An update on psychotic depression. Harvard Review of Psychiatry, 16(4), 235-247.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 18
Now, the first-generation or typical antipsychotics that were used in the earlier studies, we don't favor them because they have an increased risk of tardive dyskinesia and all of those EPS to be concerned with. Now, among the SGAs, the second-generation or atypical antipsychotics, many of them do produce weight gain and related metabolic problems particularly olanzapine. And there's actually been some study of that in the psychotic depression population.
References:
- Tang M, Osser DN. (2012). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: 2012 update on psychotic depression. Journal of Mood Disorders, 2(4),167-179.
- Hamoda, H. M., & Osser, D. N. (2008). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: An update on psychotic depression. Harvard Review of Psychiatry, 16(4), 235-247.
Slide 6 of 18
Rothschild and his group evaluated the weight gain of 118 patients from their STOP-PD study involving olanzapine and sertraline. They did find that age had a significant negative association with weight gain. The negative association is the older you were, you gained less weight on olanzapine. So for the younger patients, it's particularly a problem. And this is even after controlling for differences in total olanzapine dose and baseline body mass index of the patients. Other studies in schizophrenia have found that the weight gain from olanzapine is dose related. So they did need to control for that and did so and yet they found this age association which is kind of interesting. I did already point out in one of the previous presentations of this series that in the STOP-PD trial published last year the maintenance trial, continuing treatment after initial treatment gave additional weight gain beyond the acute phase.
References:
- Tang M, Osser DN. (2012). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: 2012 update on psychotic depression. Journal of Mood Disorders, 2(4),167-179.
- Meyers, B. S., Flint, A. J., Rothschild, A. J., Mulsant, B. H., Whyte, E. M., Peasley-Miklus, C., Papademetriou, E., Leon, A. C., Heo, M., & STOP-PD Group (2009). A double-blind randomized controlled trial of olanzapine plus sertraline vs olanzapine plus placebo for psychotic depression: the study of pharmacotherapy of psychotic depression (STOP-PD). Archives of General Psychiatry, 66(8), 838–847.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 18
Now, quetiapine causes weight gain as well in a study of antipsychotic-naive young patients being treated with an antipsychotic for schizophrenia. It was second only to olanzapine for causing weight gain. It has some other disadvantages like QTc prolongation, a package insert warning was added in 2011 regarding that, with quetiapine although some clinicians may not know about it.
References:
- Tang M, Osser DN. (2012). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: 2012 update on psychotic depression. Journal of Mood Disorders, 2(4),167-179.
- AstraZeneca Pharmaceuticals Corp. (2010). Seroquel [package insert]. Wilmington, DE: AstraZeneca Pharmaceuticals Corp.
Slide 8 of 18
And the package insert warning specifies that you have to do extra safety monitoring if you combine quetiapine with 12 specified medications that are noted in the package insert now. SSRIs are not mentioned but we do have concern now about some SSRIs and their possible QTc prolongation like escitalopram and citalopram. So probably one should do the extra safety monitoring if you are combining with some SSRIs and also with tricyclics if you wind up combining with them.
References:
- Tang M, Osser DN. (2012). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: 2012 update on psychotic depression. Journal of Mood Disorders, 2(4),167-179.
- AstraZeneca Pharmaceuticals Corp. (2010). Seroquel [package insert]. Wilmington, DE: AstraZeneca Pharmaceuticals Corp.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 18
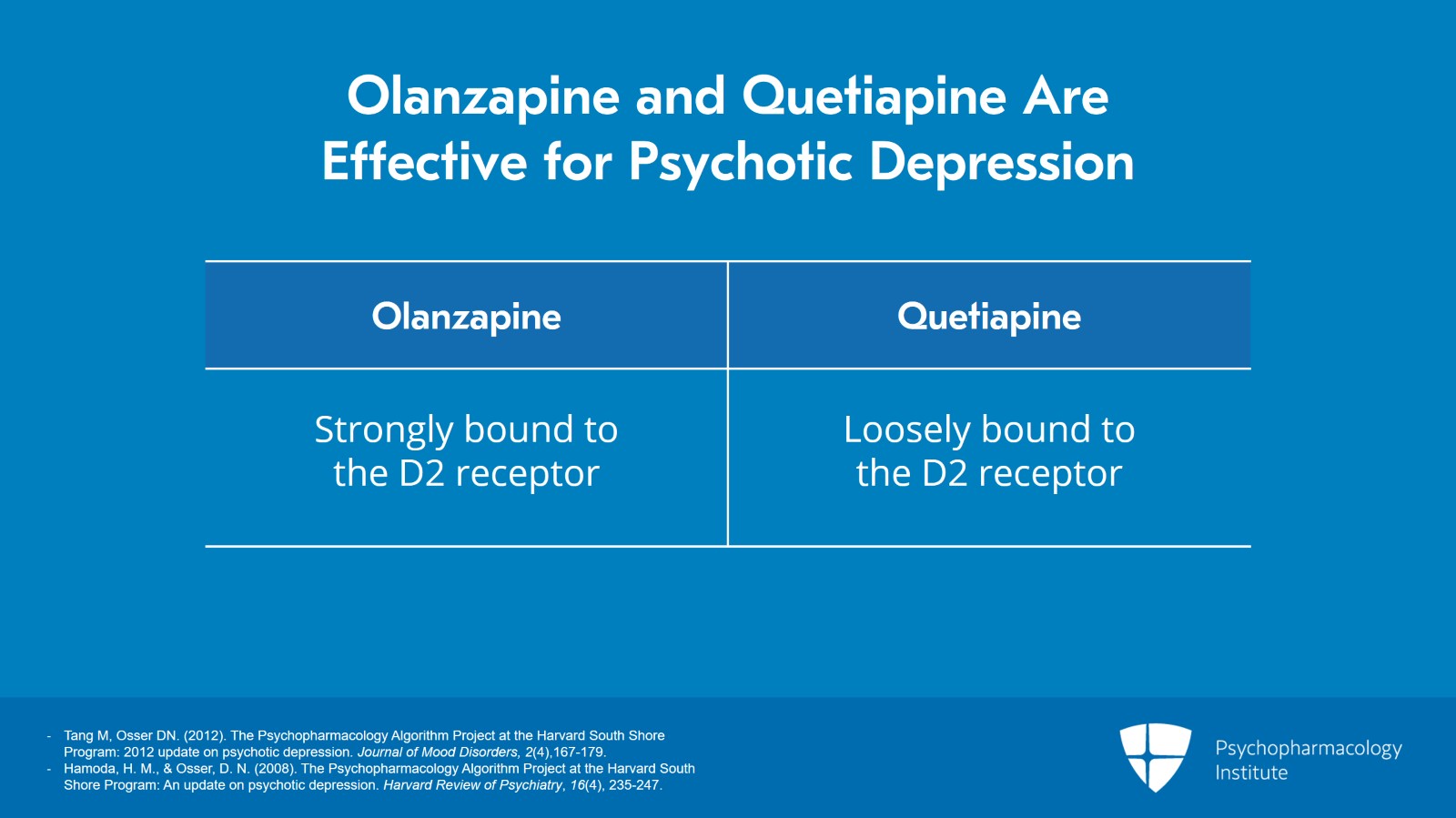
However, olanzapine and quetiapine are effective in psychotic depression combinations and despite having quite different pharmacodynamic properties. For example, olanzapine is strongly bound to the dopamine type 2 receptor and quetiapine is loosely bound. So these are different chemicals and yet both worked reasonably well as an antipsychotic to choose for effectiveness in psychotic depression.
References:
- Tang M, Osser DN. (2012). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: 2012 update on psychotic depression. Journal of Mood Disorders, 2(4),167-179.
- Hamoda, H. M., & Osser, D. N. (2008). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: An update on psychotic depression. Harvard Review of Psychiatry, 16(4), 235-247.
Slide 10 of 18
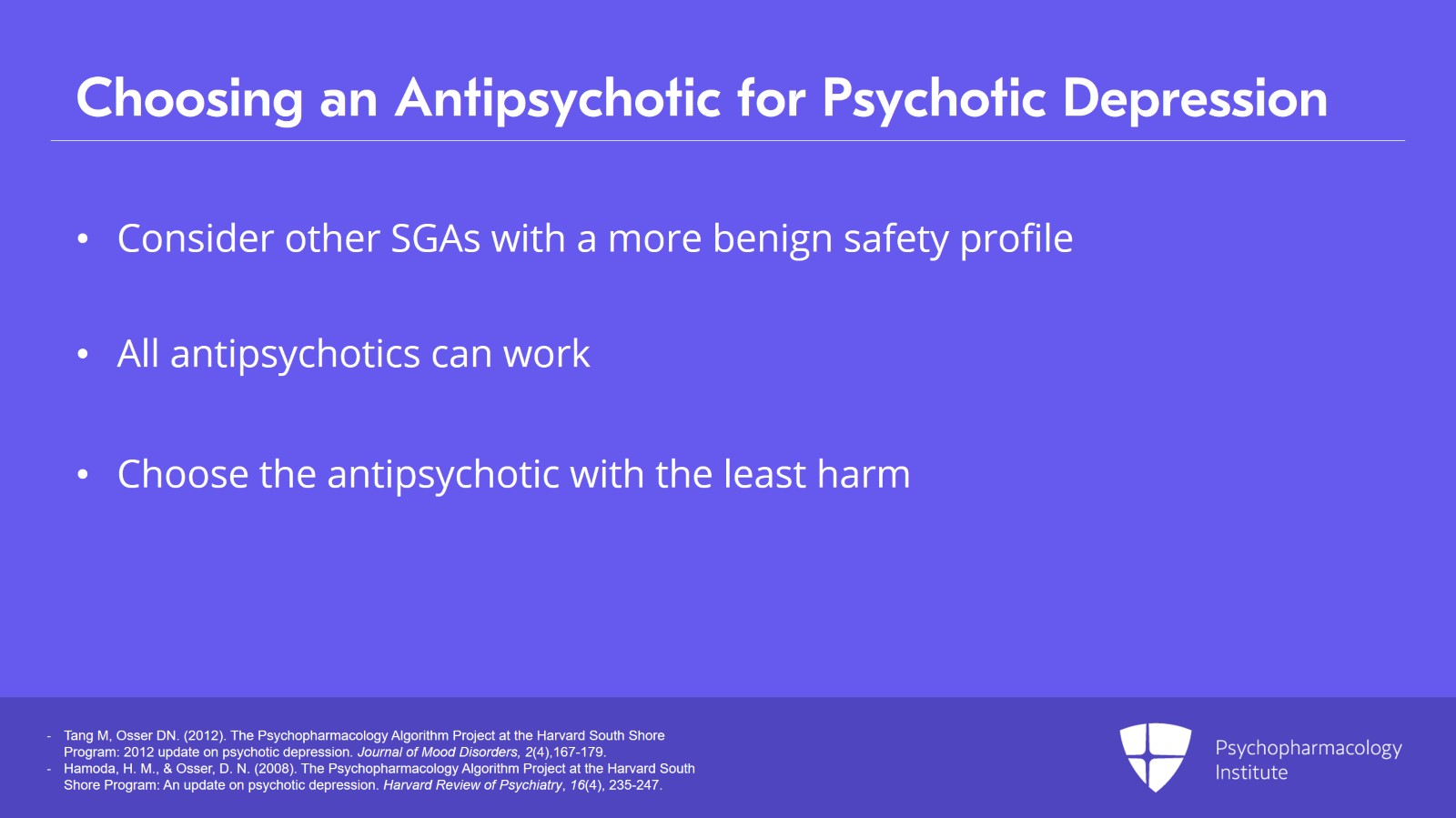
So because of this, we think it's reasonable to consider other atypical or second-generation antipsychotics that have a more benign safety profile even if their efficacy has not been well demonstrated. As best we can tell, all antipsychotics can work in short. So although we think there are differences in what antidepressant you pick, it doesn't seem to make a difference which antipsychotic you pick so you might as well pick the ones with the least harm side effect-wise.
References:
- Tang M, Osser DN. (2012). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: 2012 update on psychotic depression. Journal of Mood Disorders, 2(4),167-179.
- Hamoda, H. M., & Osser, D. N. (2008). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: An update on psychotic depression. Harvard Review of Psychiatry, 16(4), 235-247.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 18
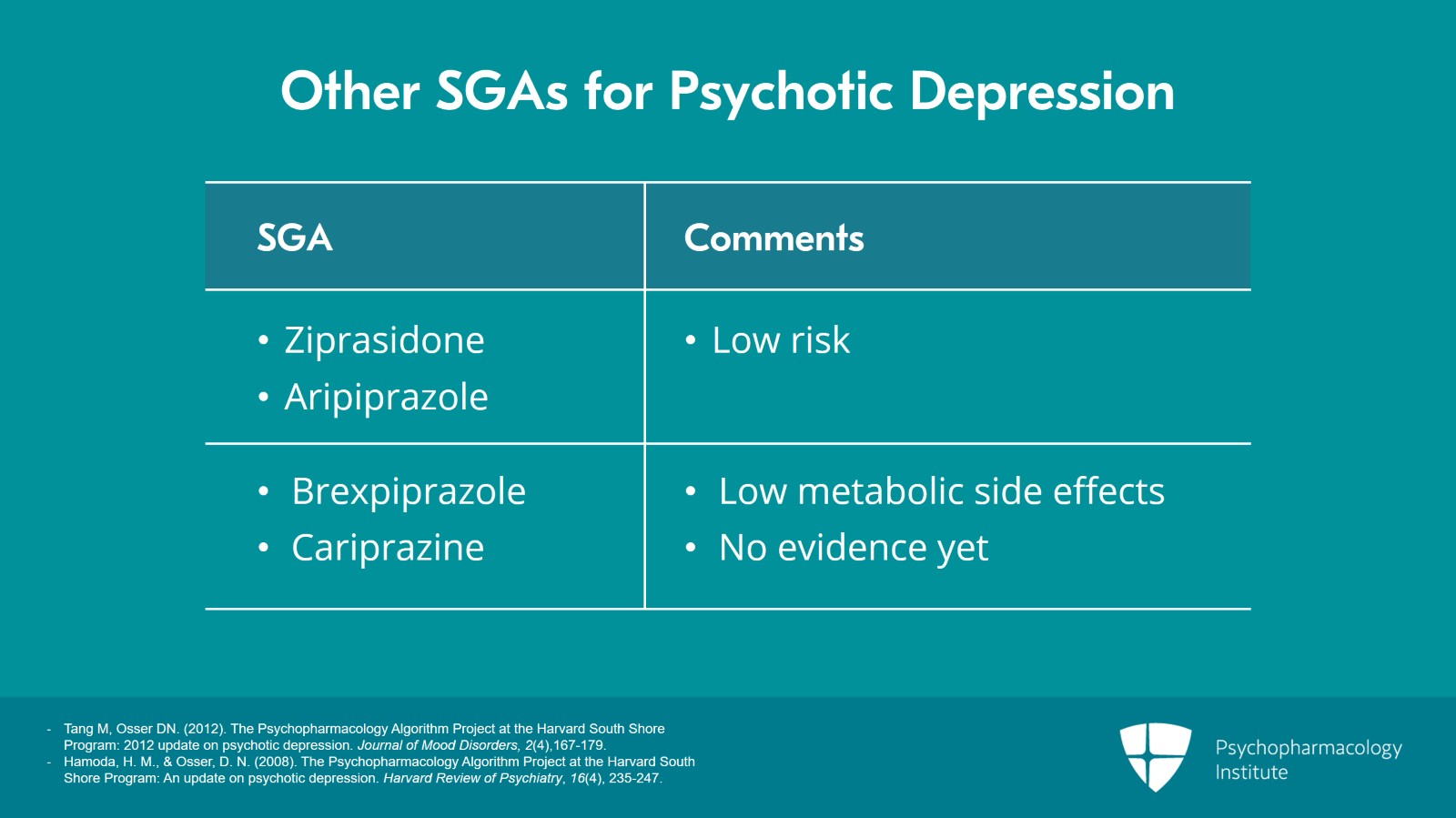
So there's a little evidence that we could look at on some of the low-risk options like ziprasidone and aripiprazole. Although we have nothing yet on the newer brand products that are very expensive but have low metabolic side effects like brexpiprazole and cariprazine, they have low weight gain but nothing we've found yet on them in psychotic depression but they might work.
References:
- Tang M, Osser DN. (2012). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: 2012 update on psychotic depression. Journal of Mood Disorders, 2(4),167-179.
- Hamoda, H. M., & Osser, D. N. (2008). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: An update on psychotic depression. Harvard Review of Psychiatry, 16(4), 235-247.
Slide 12 of 18
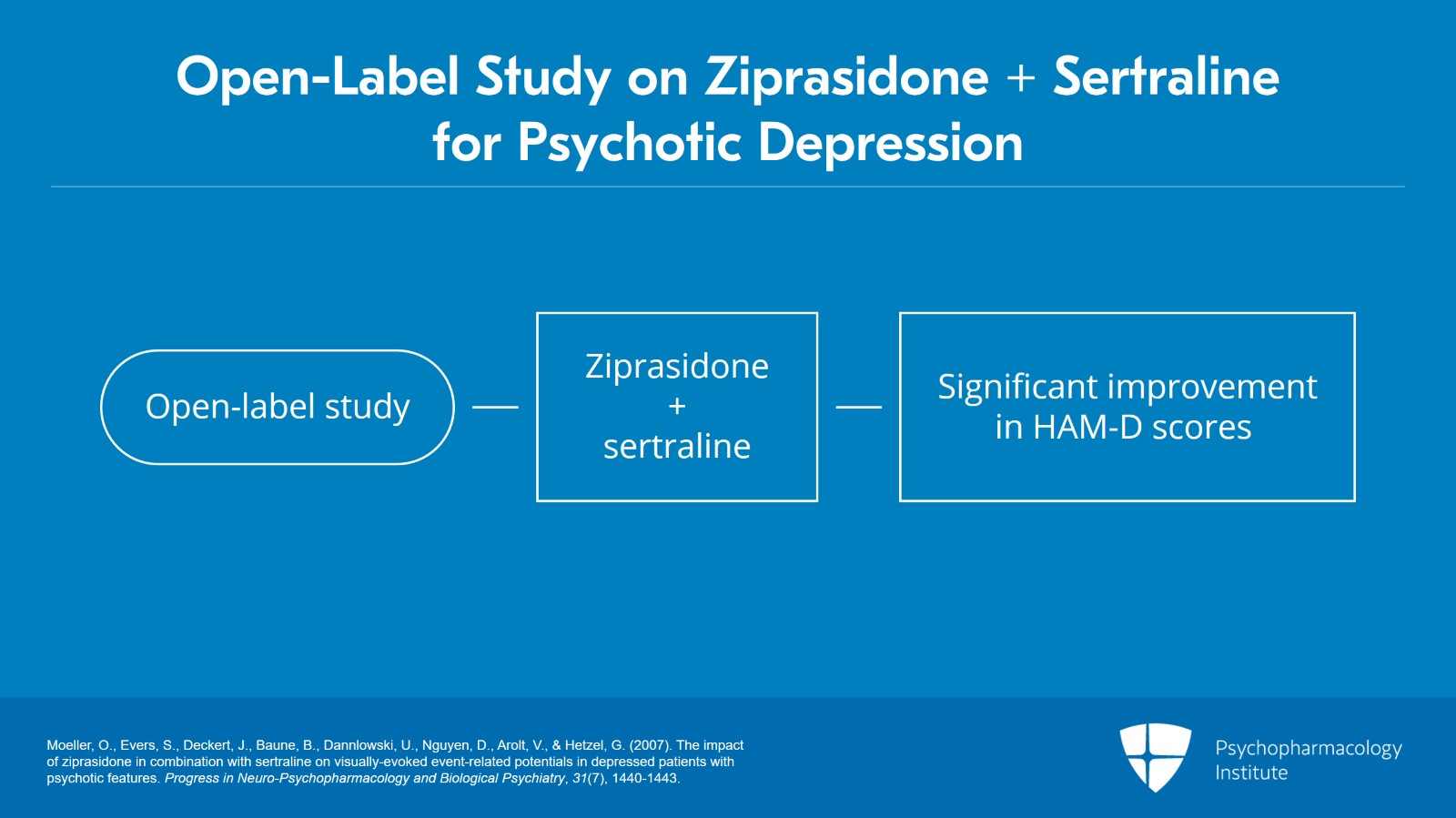
As far as what we do have some evidence on was an open-label study with ziprasidone in psychotic depression. They combined it with sertraline. The ziprasidone was 40 to 160 mg a day and the sertraline 100 to 200. It was in 19 patients for 4 weeks. Seventeen of the 19 completed the study and they improved significantly on the Hamilton.
References:
- Moeller, O., Evers, S., Deckert, J., Baune, B., Dannlowski, U., Nguyen, D., Arolt, V., & Hetzel, G. (2007). The impact of ziprasidone in combination with sertraline on visually-evoked event-related potentials in depressed patients with psychotic features. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 31(7), 1440-1443.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 18
There was no weight gain or prolactin increase on this combination. The QTc did increase by 15 msec though which was significant at the 0.04 level in this open-label trial. So that's what we have on ziprasidone, just that study.
References:
- Moeller, O., Evers, S., Deckert, J., Baune, B., Dannlowski, U., Nguyen, D., Arolt, V., & Hetzel, G. (2007). The impact of ziprasidone in combination with sertraline on visually-evoked event-related potentials in depressed patients with psychotic features. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 31(7), 1440-1443.
Slide 14 of 18
Now, we also have an open-label trial with aripiprazole as the antipsychotic and it was combined with escitalopram. This was a 7-week trial from 2009. And in this study, they used 30 mg of the aripiprazole as the maximum dose as tolerated and the escitalopram was stopped no higher than 20 mg per day. Response rate was 63% on the 13 completers of this trial, response being defined as a 50% drop and no psychosis. So that seems to be in the ballpark of other treatments with antipsychotics that we've talked about today.
References:
- Matthews, J. D., Siefert, C., Dording, C., Denninger, J. W., Park, L., Van Nieuwenhuizen, A. O., Sklarsky, K., Hilliker, S., Homberger, C., Rooney, K., & Fava, M. (2009). An open study of aripiprazole and escitalopram for psychotic major depressive disorder. Journal of Clinical Psychopharmacology, 29(1), 73-76.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 18
So therefore, to conclude the key points of today's presentation, though there are many studies with olanzapine and some with quetiapine in this diagnosis as the second-generation antipsychotic to use in treating psychotic depression, they both have undesirable metabolic and other side effects.
Slide 16 of 18
Ziprasidone and aripiprazole have had a little study, probably have comparable effectiveness and are better tolerated so we prefer them.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 18
Some newer antipsychotics have perhaps comparable safety but are unstudied and they're very expensive so we would suggest to avoid them for now at least until we get some evidence on them or maybe eventually their cost comes down.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.