Slides and Transcript
Slide 1 of 12
Hi again everyone. This is Dr. David Osser continuing the series of video presentations on major depression with psychotic features or psychotic depression. We've had 4 previous videos.
Slide 2 of 12
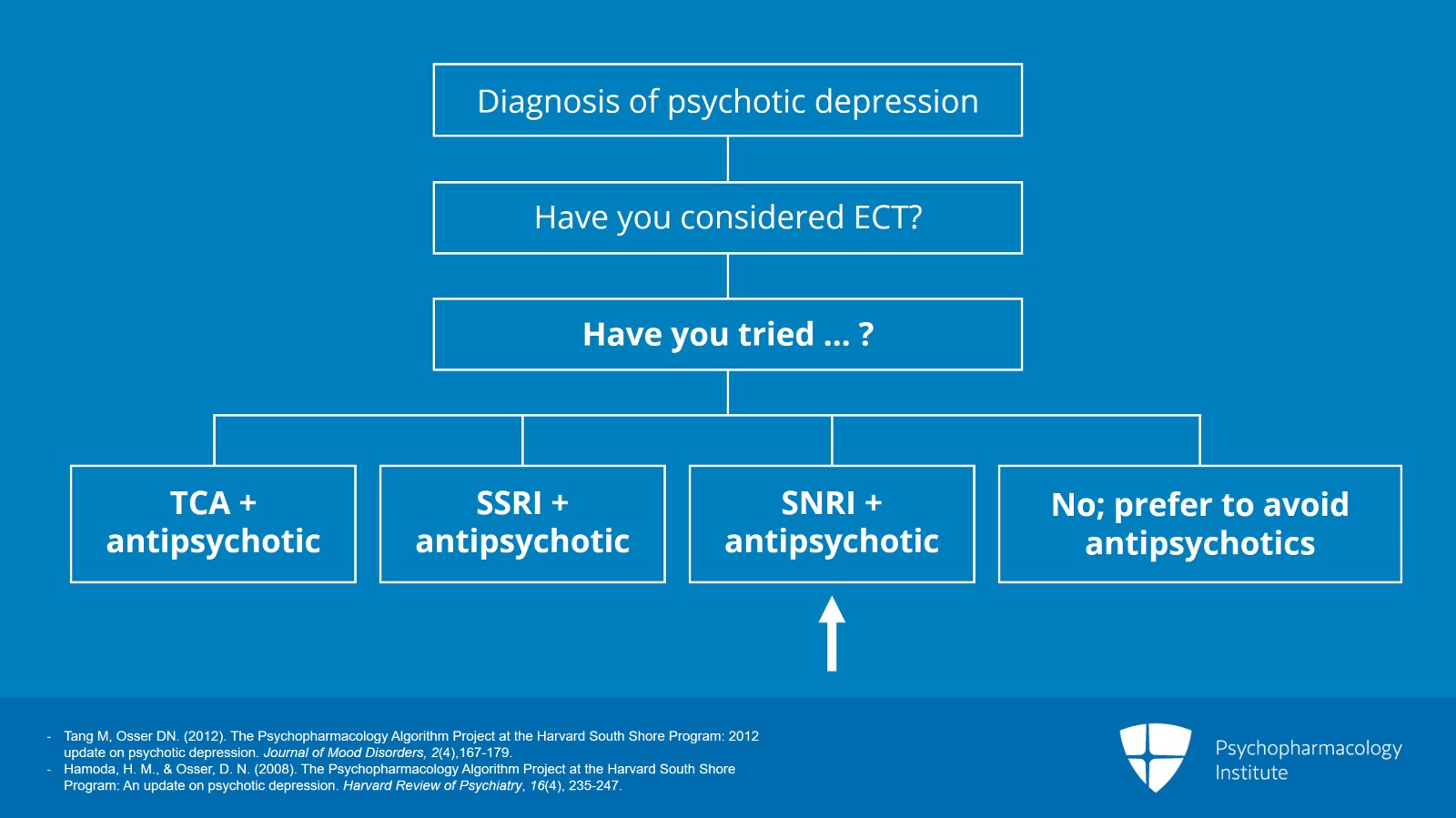
We're on video 5 in which we continue to discuss combination therapies for psychotic depression leading up to the conclusion we're going to reach soon on which combination we would prefer and in what order to try them. But I'm presenting you the data rather thoroughly and systematically so that you can see the reasoning how it emerges from the evidence. So last time, we considered the combination of an SSRI with an antipsychotic of the second-generation type, mostly olanzapine. And today, we're going to consider combination therapy with an SNRI, a serotonin-norepinephrine reuptake inhibitor, and a second-generation antipsychotic.
References:
- Tang M, Osser DN. (2012). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: 2012 update on psychotic depression. Journal of Mood Disorders, 2(4),167-179.
- Hamoda, H. M., & Osser, D. N. (2008). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: An update on psychotic depression. Harvard Review of Psychiatry, 16(4), 235-247.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 12
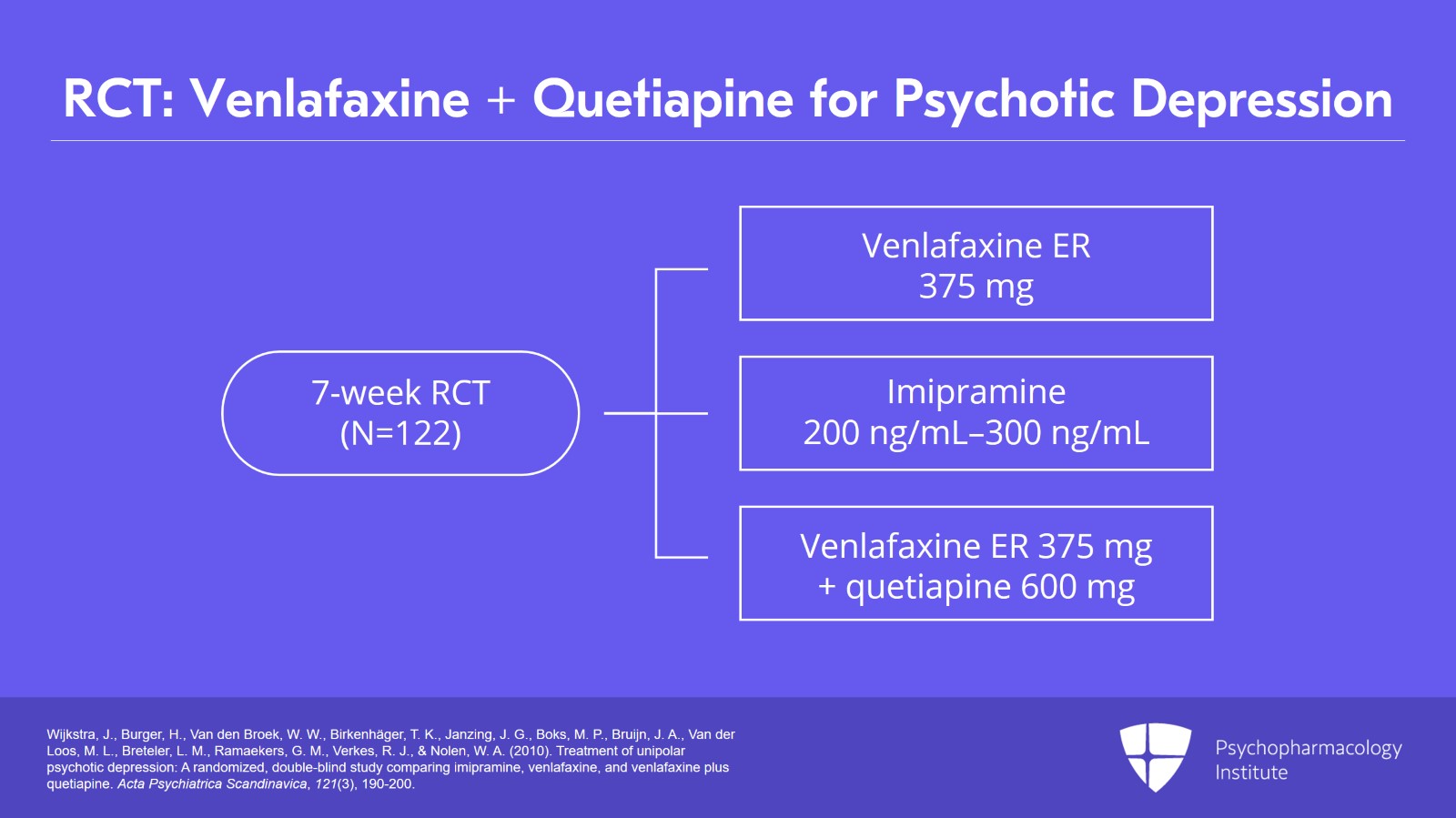
We have a study by Wijkstra in 2010. So there were 122 patients in this study and they were treated for 7 weeks, and it was a double-blind, randomized controlled trial involving 3 treatment arms, venlafaxine extended-release version, imipramine, or a combination of venlafaxine and quetiapine. The venlafaxine alone group got 375 mg. The imipramine group, they were dosed to produce a plasma level of 200 to 300 ng/ml of imipramine and desipramine, its metabolite. The third combination group got venlafaxine extended release also at 375 mg daily and they got the quetiapine at 600 mg daily, pretty robust dosing.
References:
- Wijkstra, J., Burger, H., Van den Broek, W. W., Birkenhäger, T. K., Janzing, J. G., Boks, M. P., Bruijn, J. A., Van der Loos, M. L., Breteler, L. M., Ramaekers, G. M., Verkes, R. J., & Nolen, W. A. (2010). Treatment of unipolar psychotic depression: A randomized, double-blind study comparing imipramine, venlafaxine, and venlafaxine plus quetiapine. Acta Psychiatrica Scandinavica, 121(3), 190-200.
Slide 4 of 12
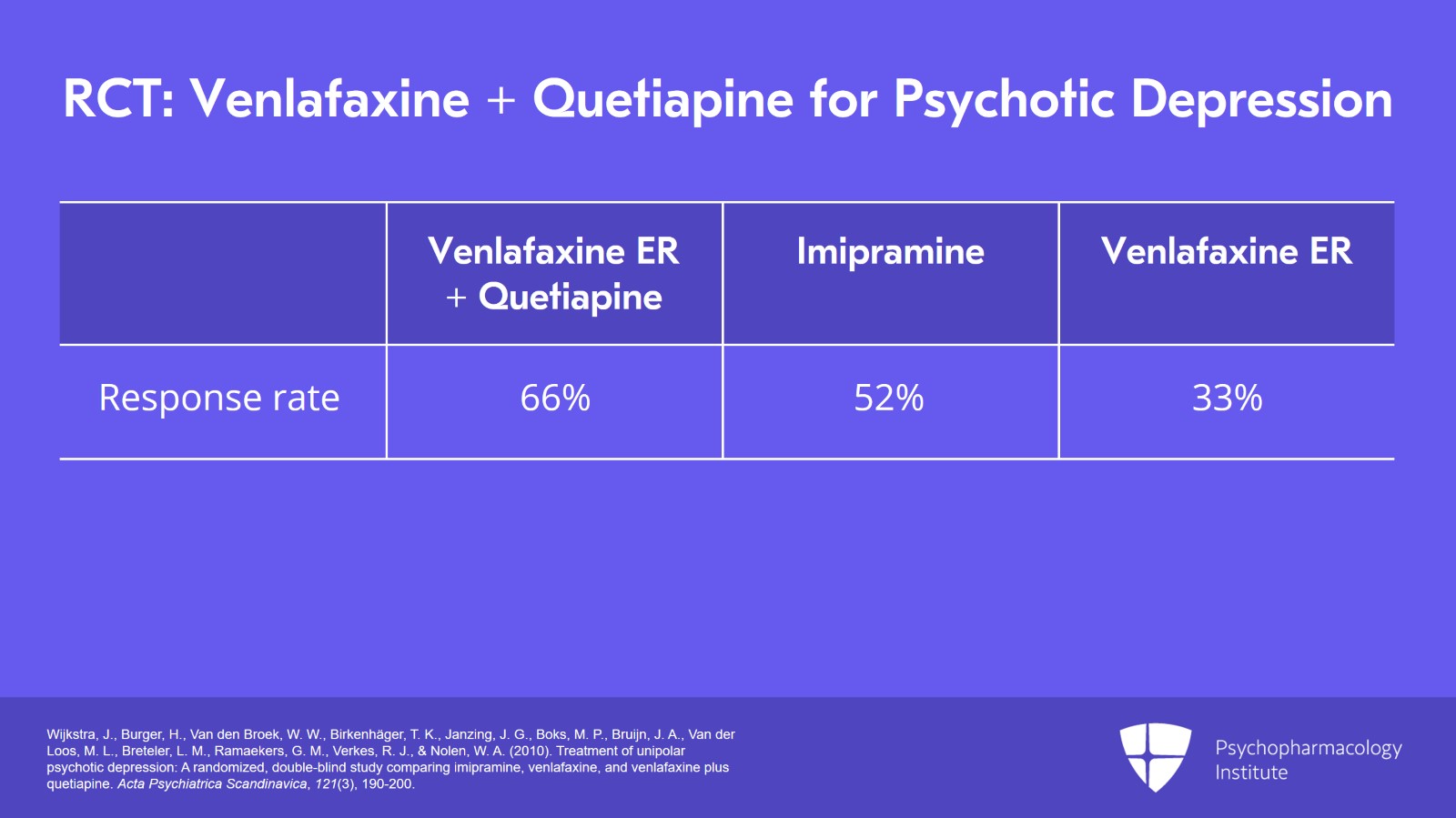
And what were the results? Sixty-six percent of the combination group responded, 27 out of 41, versus 52% on the imipramine alone group and 33% on the venlafaxine alone group. So it seems that the combination therapy is more effective than venlafaxine alone. The odds ratio was 4 for that difference. But there was no significant difference between the combination and imipramine alone in this trial with an odds ratio of 1.8 being nonsignificant. It looks numerically significant. That's 80% better response but still we're talking about hardly any difference statistically.
References:
- Wijkstra, J., Burger, H., Van den Broek, W. W., Birkenhäger, T. K., Janzing, J. G., Boks, M. P., Bruijn, J. A., Van der Loos, M. L., Breteler, L. M., Ramaekers, G. M., Verkes, R. J., & Nolen, W. A. (2010). Treatment of unipolar psychotic depression: A randomized, double-blind study comparing imipramine, venlafaxine, and venlafaxine plus quetiapine. Acta Psychiatrica Scandinavica, 121(3), 190-200.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 12
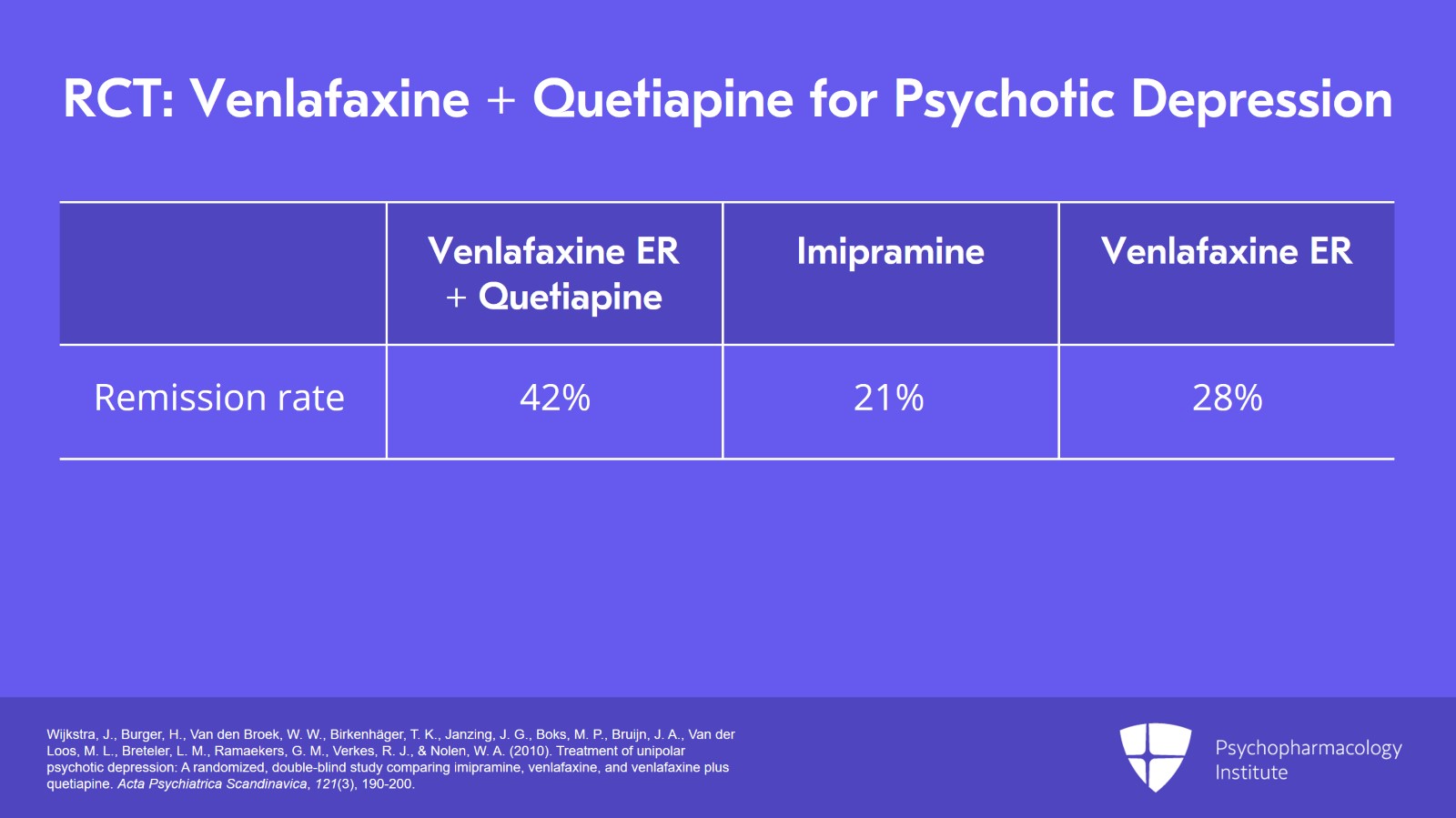
They also checked remission rates and they were a little bit contradictory. They did favor the combination with 42% remitting on the combination of venlafaxine and high-dose quetiapine. Twenty-one percent remitted on the imipramine. So, it looked better when you looked at remissions as opposed to merely improvement. And the venlafaxine monotherapy did better though, 28% responding with remission to the venlafaxine monotherapy. So, venlafaxine alone looked better when remission was your outcome but yet it was still inferior to the combination.
References:
- Wijkstra, J., Burger, H., Van den Broek, W. W., Birkenhäger, T. K., Janzing, J. G., Boks, M. P., Bruijn, J. A., Van der Loos, M. L., Breteler, L. M., Ramaekers, G. M., Verkes, R. J., & Nolen, W. A. (2010). Treatment of unipolar psychotic depression: A randomized, double-blind study comparing imipramine, venlafaxine, and venlafaxine plus quetiapine. Acta Psychiatrica Scandinavica, 121(3), 190-200.
Slide 6 of 12
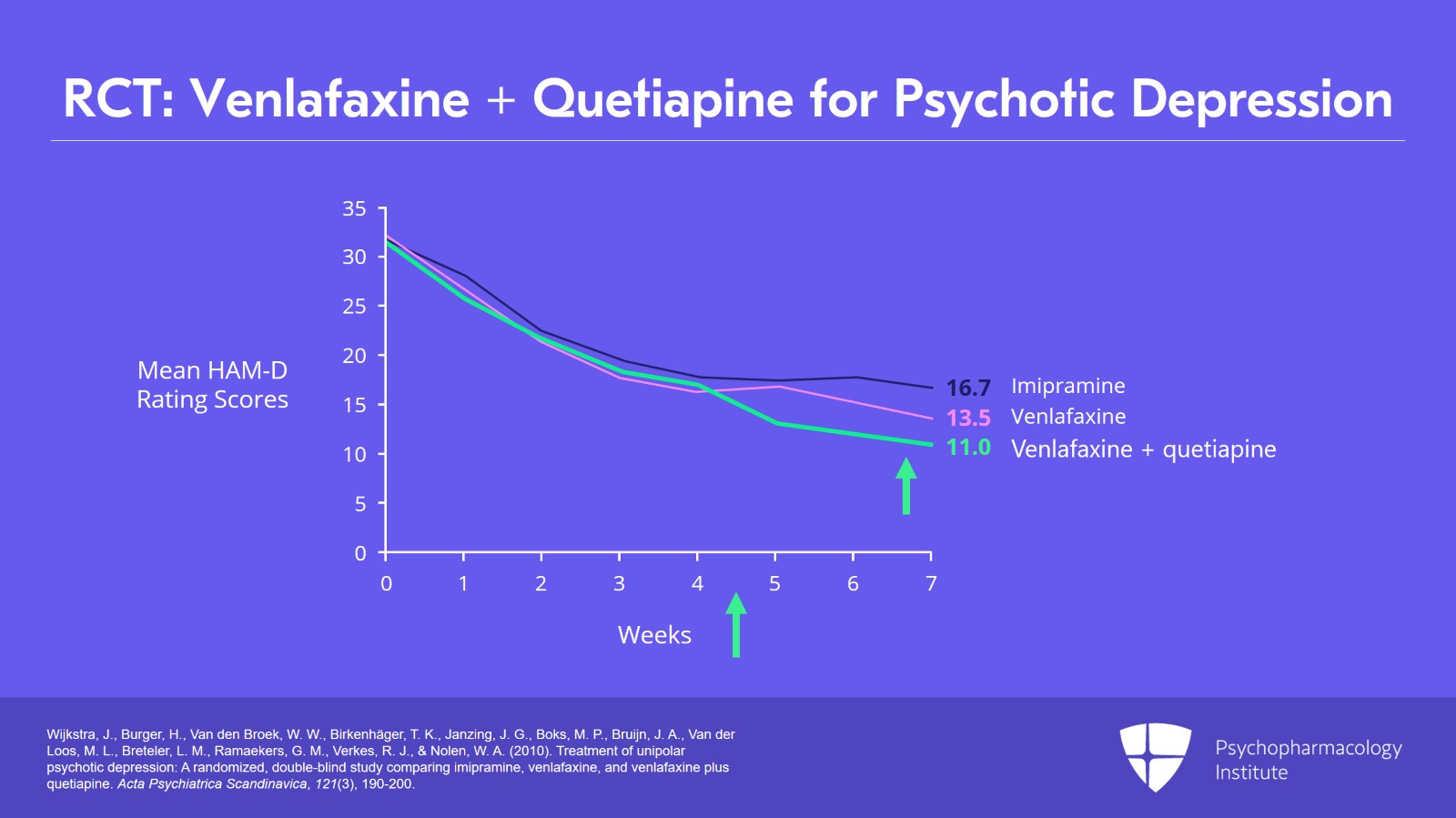
You can see the graph of these three groups showing the changes in the Hamilton scale and showing that beyond 3 to 4 weeks the venlafaxine and quetiapine group separates from the other two groups noticeably but not dramatically. And again, the percentage of people responding on the combination is still pretty small compared to those robust responses we used to see in those earlier tricyclic studies where they're using amitriptyline with a first-generation antipsychotic.
References:
- Wijkstra, J., Burger, H., Van den Broek, W. W., Birkenhäger, T. K., Janzing, J. G., Boks, M. P., Bruijn, J. A., Van der Loos, M. L., Breteler, L. M., Ramaekers, G. M., Verkes, R. J., & Nolen, W. A. (2010). Treatment of unipolar psychotic depression: A randomized, double-blind study comparing imipramine, venlafaxine, and venlafaxine plus quetiapine. Acta Psychiatrica Scandinavica, 121(3), 190-200.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 12
So, the implications of this study is that an SNRI plus an antipsychotic looks more effective than antidepressant alone. The outcomes seem a little more solid with the venlafaxine when you look at remission as opposed to looking at improvement.
References:
- Wijkstra, J., Burger, H., Van den Broek, W. W., Birkenhäger, T. K., Janzing, J. G., Boks, M. P., Bruijn, J. A., Van der Loos, M. L., Breteler, L. M., Ramaekers, G. M., Verkes, R. J., & Nolen, W. A. (2010). Treatment of unipolar psychotic depression: A randomized, double-blind study comparing imipramine, venlafaxine, and venlafaxine plus quetiapine. Acta Psychiatrica Scandinavica, 121(3), 190-200.
Slide 8 of 12
The limitations of this study are there is no placebo group and the remission comparisons were done in a posthoc secondary outcome measure with small n's involved.
References:
- Wijkstra, J., Burger, H., Van den Broek, W. W., Birkenhäger, T. K., Janzing, J. G., Boks, M. P., Bruijn, J. A., Van der Loos, M. L., Breteler, L. M., Ramaekers, G. M., Verkes, R. J., & Nolen, W. A. (2010). Treatment of unipolar psychotic depression: A randomized, double-blind study comparing imipramine, venlafaxine, and venlafaxine plus quetiapine. Acta Psychiatrica Scandinavica, 121(3), 190-200.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 12
We now are able to try to reach a conclusion about what antidepressant should you choose to combine with your antipsychotic in treating your case of psychotic depression with medication. There's a slight basis for preferring a tricyclic over an SSRI for effectiveness. But this has to be weighed against a stronger basis to prefer an SSRI for safety including overdose risk in this population that has higher suicide risk than other depression patients. Now, safety concerns would favor venlafaxine over a tricyclic as well.
References:
- Tang M, Osser DN. (2012). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: 2012 update on psychotic depression. Journal of Mood Disorders, 2(4),167-179.
- Wijkstra, J., Burger, H., Van den Broek, W. W., Birkenhäger, T. K., Janzing, J. G., Boks, M. P., Bruijn, J. A., Van der Loos, M. L., Breteler, L. M., Ramaekers, G. M., Verkes, R. J., & Nolen, W. A. (2010). Treatment of unipolar psychotic depression: A randomized, double-blind study comparing imipramine, venlafaxine, and venlafaxine plus quetiapine. Acta Psychiatrica Scandinavica, 121(3), 190-200.
Slide 10 of 12
We do have the SNRI venlafaxine that worked well in combination with an antipsychotic separating from monotherapy especially on remission. So we think of the 2 choices, an SSRI or an SNRI, we think the first-line antidepressant for the combination is venlafaxine. Now, you might ask, well, what about all those other antidepressants that are out there? Well, there's no evidence. We've got no evidence to support favoring other antidepressant types like bupropion, mirtazapine, MAOIs. They're just not studied in psychotic depression.
References:
- Tang M, Osser DN. (2012). The Psychopharmacology Algorithm Project at the Harvard South Shore Program: 2012 update on psychotic depression. Journal of Mood Disorders, 2(4),167-179.
- Wijkstra, J., Burger, H., Van den Broek, W. W., Birkenhäger, T. K., Janzing, J. G., Boks, M. P., Bruijn, J. A., Van der Loos, M. L., Breteler, L. M., Ramaekers, G. M., Verkes, R. J., & Nolen, W. A. (2010). Treatment of unipolar psychotic depression: A randomized, double-blind study comparing imipramine, venlafaxine, and venlafaxine plus quetiapine. Acta Psychiatrica Scandinavica, 121(3), 190-200.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 12
So to conclude, the key points of this talk, we have now finished reviewing the evidence for the various combination therapies for psychotic depression. Adding up the last 3 discussions, we think venlafaxine offers the best combination of reasonable effectiveness and reasonable safety as the first antidepressant to try in combination with an antipsychotic. In the next section, we're going to say more about what antipsychotic to use.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.