Slides and Transcript
Slide 1 of 14
Okay. So, in section 6, we are going to drill down a bit further into improving psychotropic adherence, targeting reasons for nonadherence, and a 3-tiered approach to enhancing medication adherence.
Slide 2 of 14
So, as we’ve touched on already, it is important for clinicians to try to target the reasons for poor adherence, assessing why a person is poorly adherent so the intentional versus the unintentional, Can’t versus Won’t.
References:
- Crame. (1991). Patient compliance in medical practice and clinical trials. Lippincott Williams & Wilkins.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 14
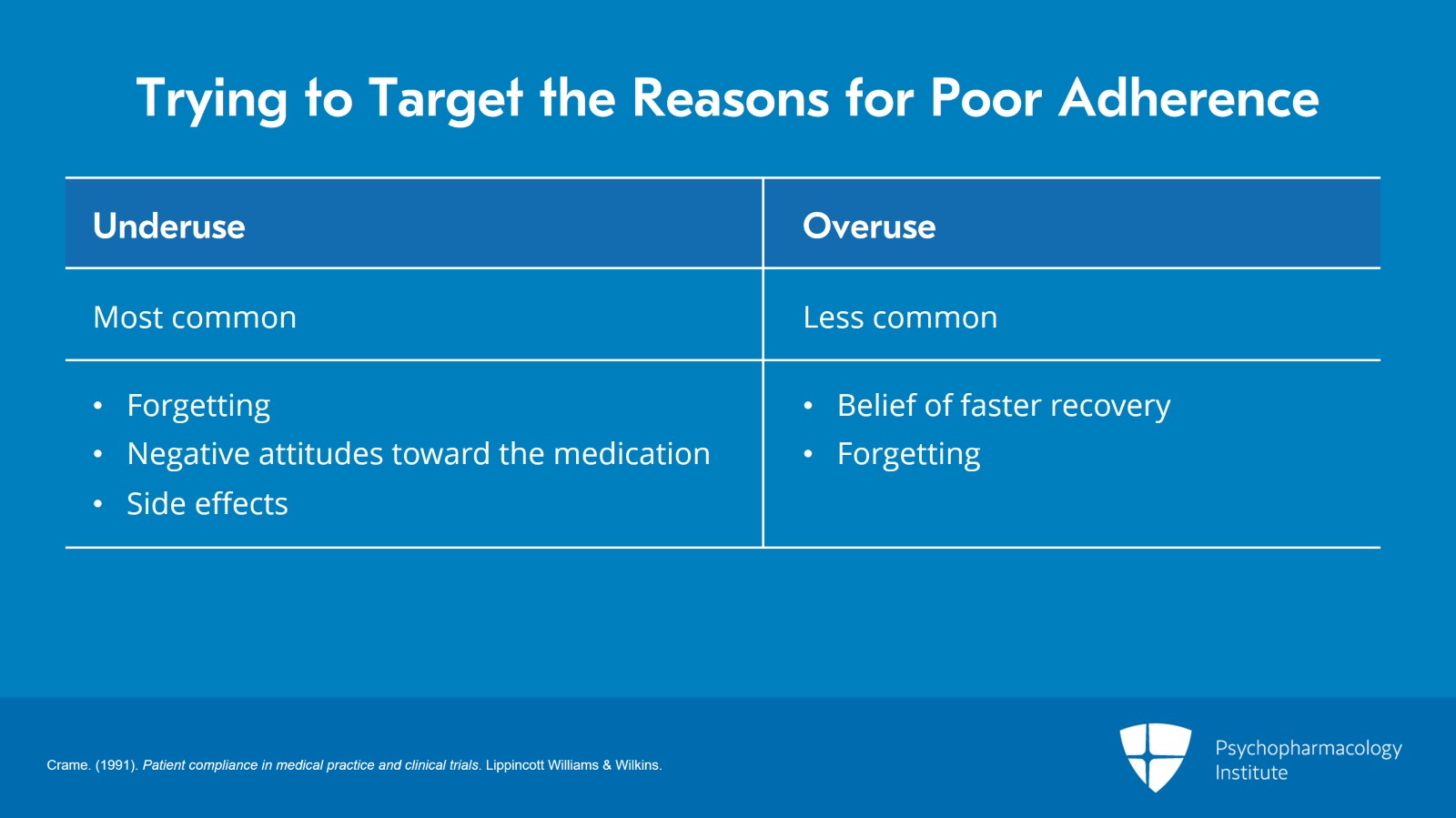
Underuse tends to be the most common and reasons can include forgetting, negative attitudes toward the treatment or medication, side effects or fear of side effects. Overuse is less common, but this definitely can occur, increased dose in the mistaken belief that if I take more, my recovery will be faster or forgetting if a person took a morning dose of medication, for example, and just forgot that they took it, they could potentially take it again.
References:
- Crame. (1991). Patient compliance in medical practice and clinical trials. Lippincott Williams & Wilkins.
Slide 4 of 14
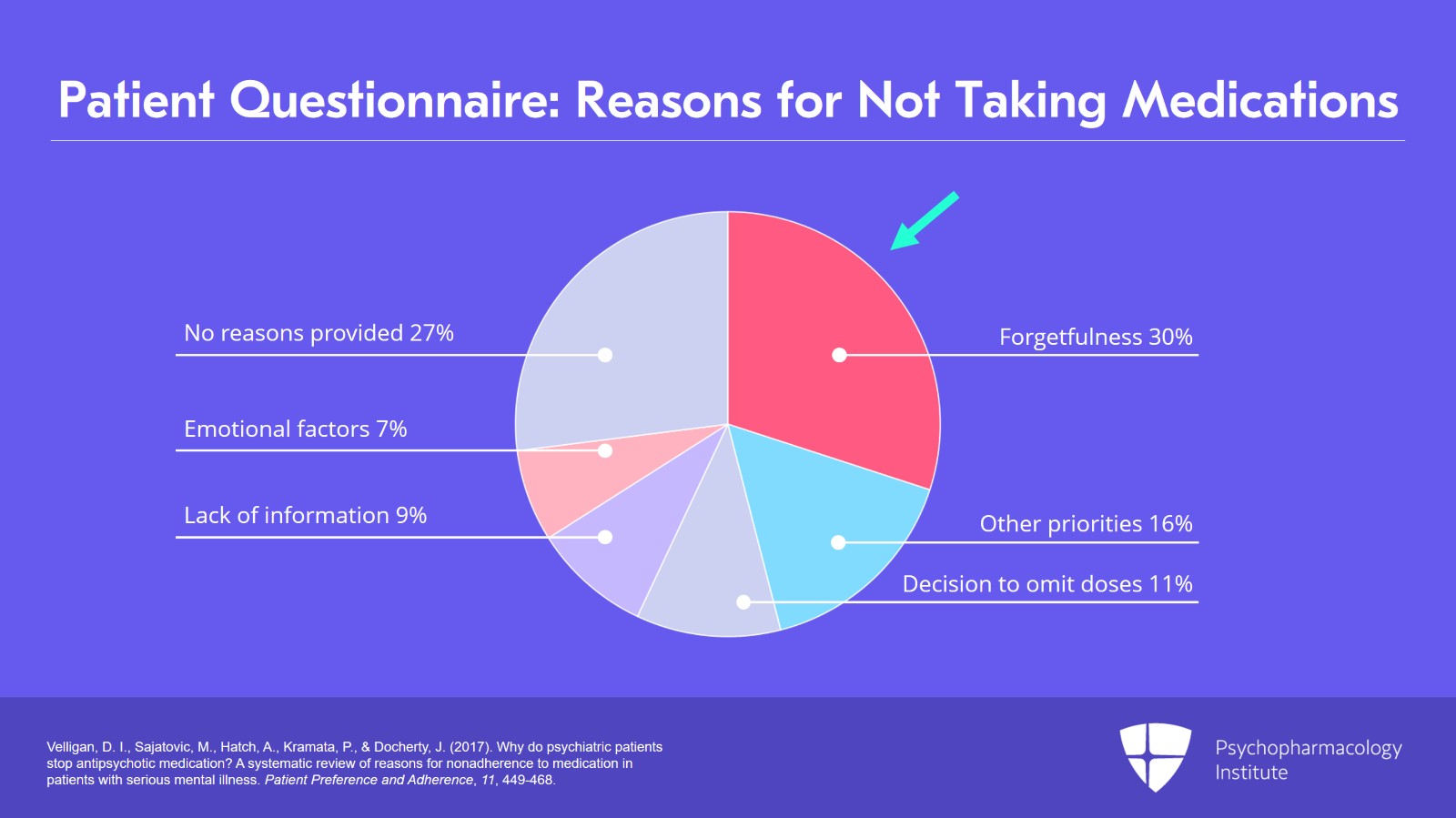
This slide here based on a patient questionnaire looked at reasons for not taking medications and you can see that forgetfulness was the biggest reason. And so, knowing that, you can think about ways to prompt remembering. And then there are a variety of other reasons that include lack of information, other priorities, and emotional factors.
References:
- Velligan, D. I., Sajatovic, M., Hatch, A., Kramata, P., & Docherty, J. (2017). Why do psychiatric patients stop antipsychotic medication? A systematic review of reasons for nonadherence to medication in patients with serious mental illness. Patient Preference and Adherence, 11, 449-468.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 14
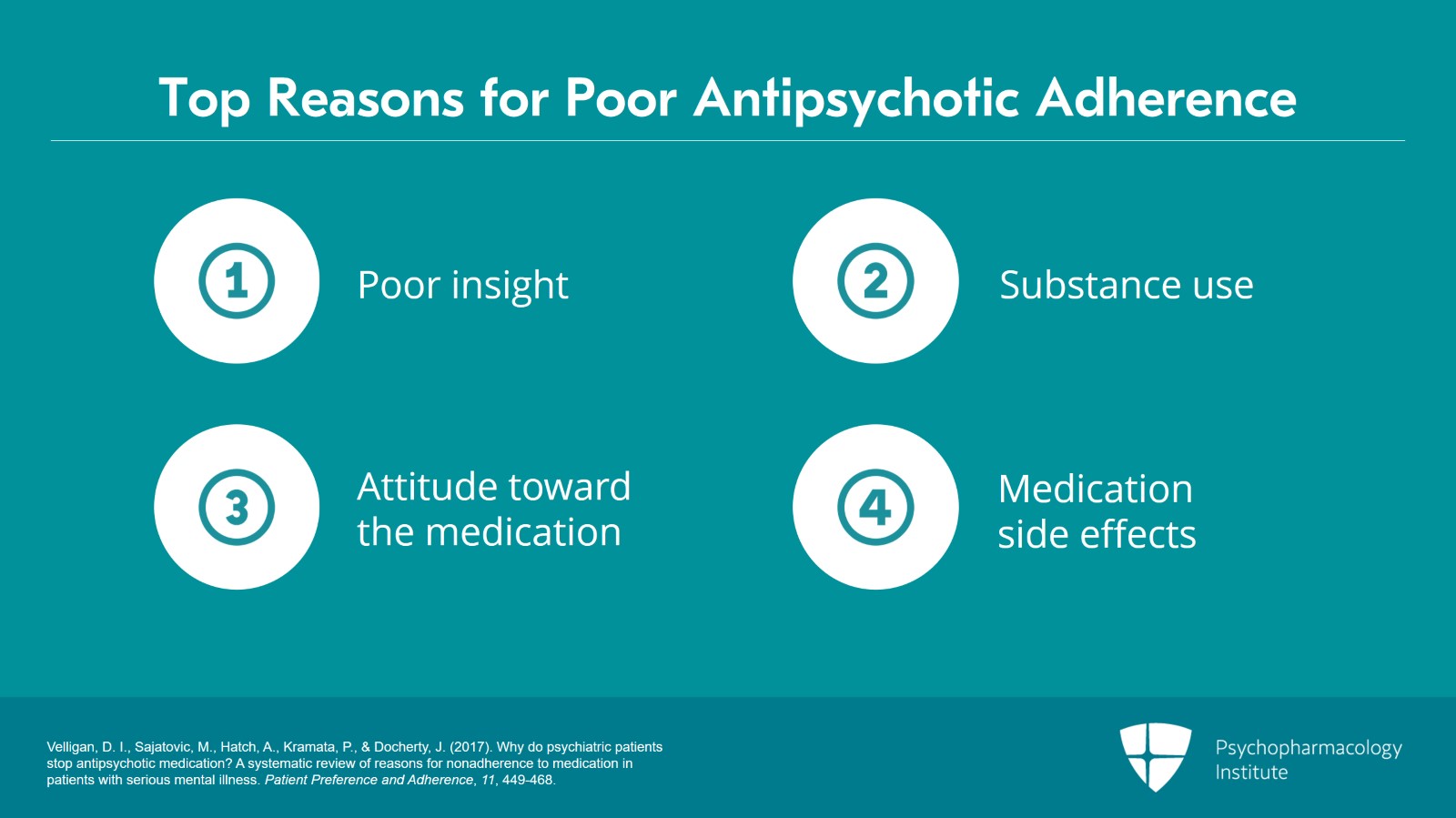
The next slide shows us top reasons for poor antipsychotic adherence and the top reason was poor insight, substance use, attitude toward the medication, all being the top three.
Medication side effects were a fourth reason here. Often, clinicians think that side effects are the top driver. Our data didn’t suggest that that was the case although it was still an important reason. And as we’ve discussed earlier, side effects should definitely be part of the discussion with patients.
References:
- Velligan, D. I., Sajatovic, M., Hatch, A., Kramata, P., & Docherty, J. (2017). Why do psychiatric patients stop antipsychotic medication? A systematic review of reasons for nonadherence to medication in patients with serious mental illness. Patient Preference and Adherence, 11, 449-468.
Slide 6 of 14
In some qualitative research that we’ve done in people with bipolar disorder where we wanted to focus on the positive aspects.
We asked patients with bipolar disorder, “what do you think medications are doing for you?” the most common positive response was balancing or stabilizing my mood than decreasing my anxiety or depression and improving sleep and mainly focusing on the depressive aspect.
References:
- Sajatovic, M., Jenkins, J. H., Cassidy, K. A., & Muzina, D. J. (2009). Medication treatment perceptions, concerns and expectations among depressed individuals with type I bipolar disorder. Journal of Affective Disorders, 115(3), 360-366.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 14
So, in order to partner with patients, not only is it a good idea to find out what their barriers are, so why are they not adherent, but also what do they believe the medications do for them, so both the positive and the negative. Both of those should be part of the discussion.
References:
- Sajatovic, M., Jenkins, J. H., Cassidy, K. A., & Muzina, D. J. (2009). Medication treatment perceptions, concerns and expectations among depressed individuals with type I bipolar disorder. Journal of Affective Disorders, 115(3), 360-366.
Slide 8 of 14
The 3-tiered approach to enhancing psychotropic medication.
This is adapted from an Institute of Medicine recommendation. So, we can think about adherence enhancement approaches or adherence enhancement interventions. We can think about them as universal, selected and indicated.
References:
- Riley W, Velligan D, Sajotovic M, Valenstein M, Safren S, Fernandez RL, Weiden P, Ogedegbe G. (2009). Adherence to psychiatric treatments. Current Medical Literature: Psychiatry, 20, 89-96.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 14
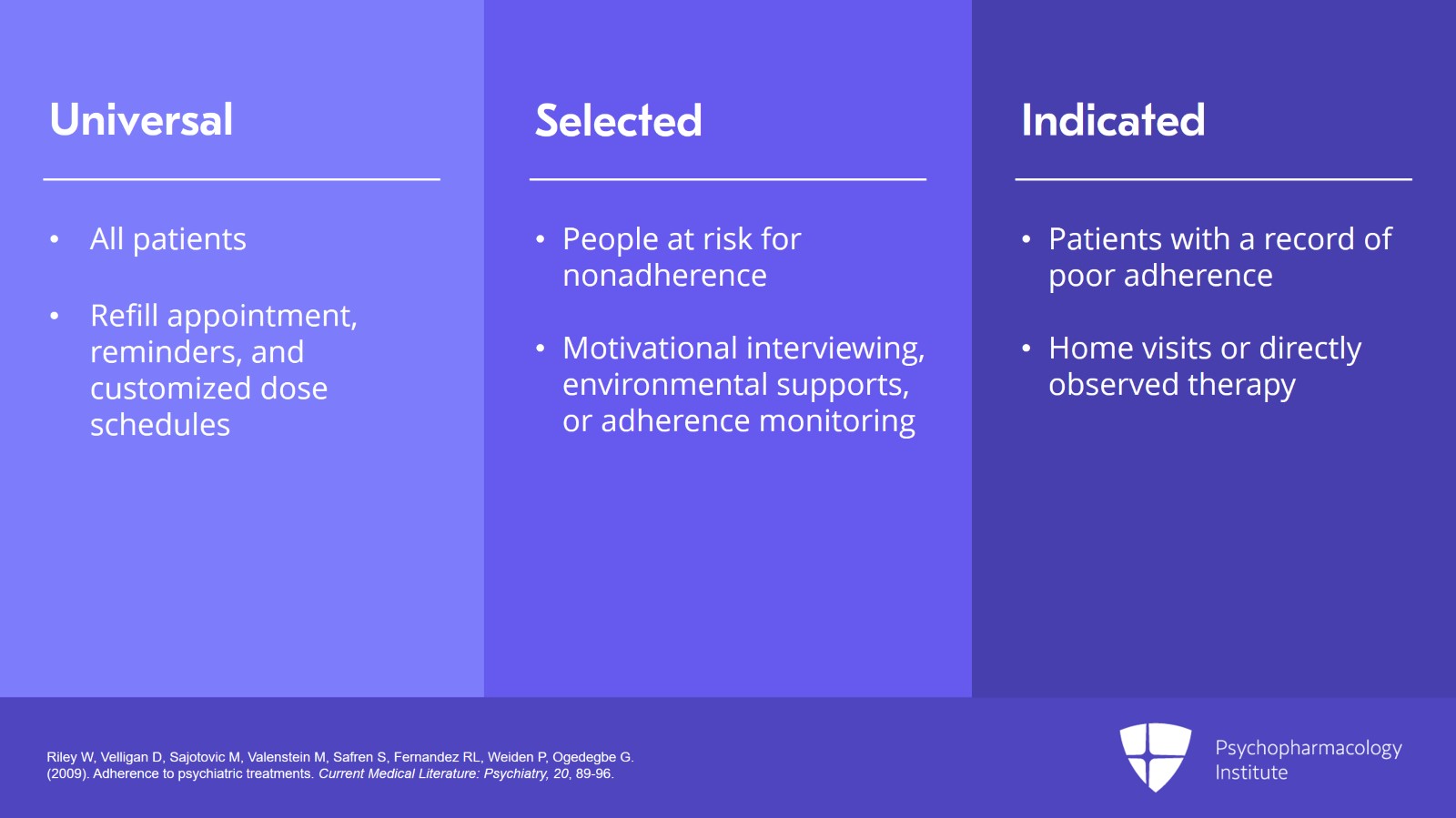
So universal are things that are easy. They are administered to all patients. This tends to be low burden that include refill appointment, reminders, customized dose schedules.
Selected AEs are a little bit higher burden. They’re administered to people at risk for nonadherence that might include things like motivational interviewing or environmental supports, adherence monitoring.
And then indicated AEIs are of the highest burden. These are highly customized interventions and administered to patients with a record of poor adherence in the past that could include home visits, directly observed therapy where you watch people take medications.
References:
- Riley W, Velligan D, Sajotovic M, Valenstein M, Safren S, Fernandez RL, Weiden P, Ogedegbe G. (2009). Adherence to psychiatric treatments. Current Medical Literature: Psychiatry, 20, 89-96.
Slide 10 of 14
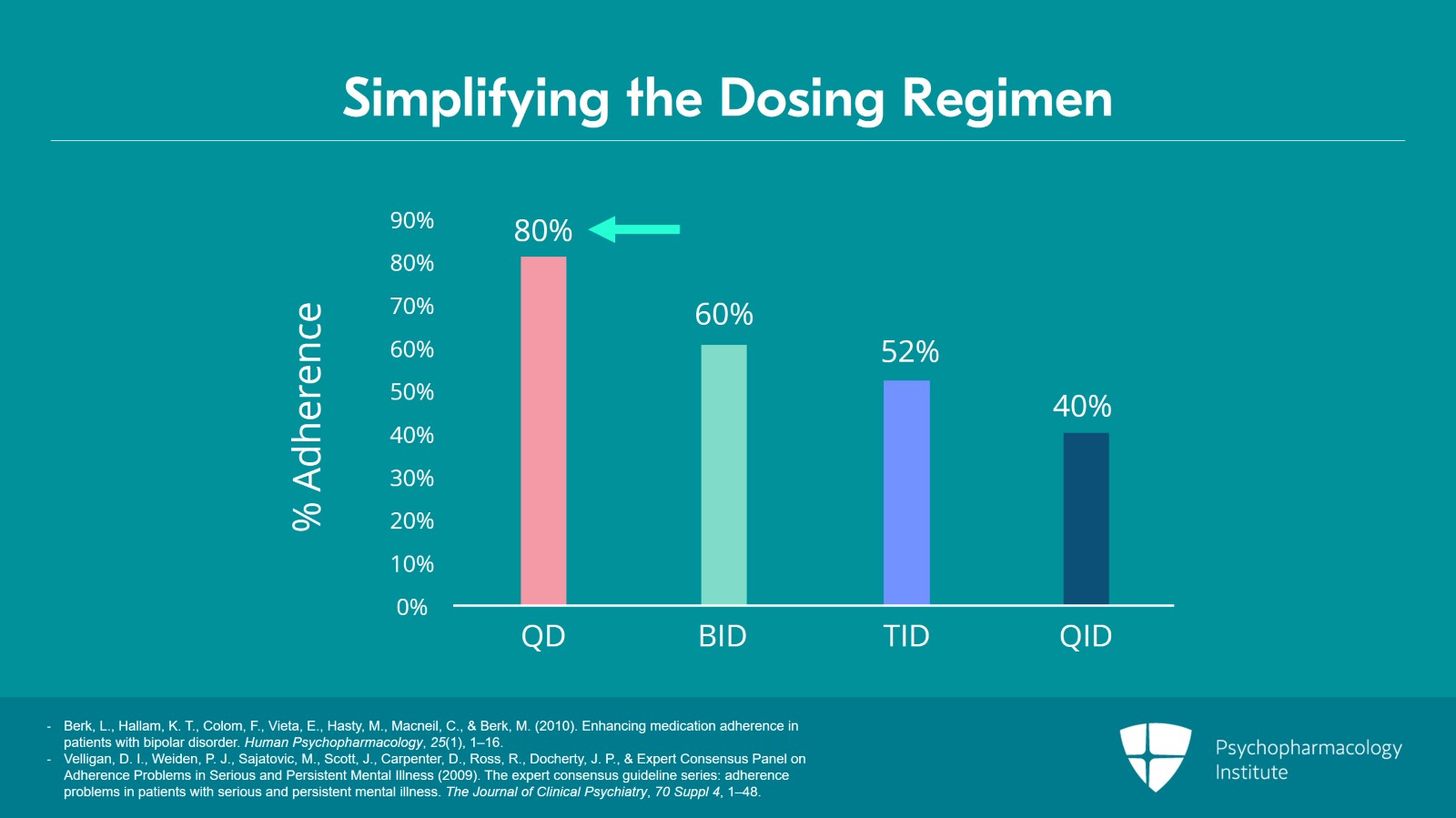
Other things that we can do are to simplify the dosing regimen.
So, this is an oldie but goodie slide that shows that percent adherence is higher with once daily or q. day dosing and goes down the more times a day a person has to remember to take the medication.
One way to think about it is every time a person is supposed to take a medication, that’s a decision point.
Take it or not take it, forget it or not forget it. And you want to minimize those opportunities.
References:
- Berk, L., Hallam, K. T., Colom, F., Vieta, E., Hasty, M., Macneil, C., & Berk, M. (2010). Enhancing medication adherence in patients with bipolar disorder. Human Psychopharmacology, 25(1), 1–16.
- Velligan, D. I., Weiden, P. J., Sajatovic, M., Scott, J., Carpenter, D., Ross, R., Docherty, J. P., & Expert Consensus Panel on Adherence Problems in Serious and Persistent Mental Illness (2009). The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. The Journal of Clinical Psychiatry, 70 Suppl 4, 1–48.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 14
Other things we can think about is different formulations.
So, there are some long-acting injectable formulations available for antipsychotic drugs and that is a possibility for people that are poorly adherent and that will take that q.d. dosing directly out of the mix where maybe it could be administered monthly or even less frequently with some of the compounds that are available.
References:
- Berk, L., Hallam, K. T., Colom, F., Vieta, E., Hasty, M., Macneil, C., & Berk, M. (2010). Enhancing medication adherence in patients with bipolar disorder. Human Psychopharmacology, 25(1), 1–16.
- Velligan, D. I., Weiden, P. J., Sajatovic, M., Scott, J., Carpenter, D., Ross, R., Docherty, J. P., & Expert Consensus Panel on Adherence Problems in Serious and Persistent Mental Illness (2009). The expert consensus guideline series: adherence problems in patients with serious and persistent mental illness. The Journal of Clinical Psychiatry, 70 Suppl 4, 1–48.
Slide 12 of 14
Key points in this section are that understanding why individuals are suboptimally adherent can help guide effective strategies to promote adherence.
Just as there’s no one-size-fits-all reason for poor adherence, there’s no one-size-fits-all way to improve adherence.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 14
Using multiple drug approaches such as providing drug formulations that minimize having to remember to take medications and building in reminders or cues to tie medication taking into daily routines can all enhance adherence.
And patients may need approaches that are more or less intensive based on their personal circumstances, attitudes toward both medications and treatment, and their engagement in care.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.