Slides and Transcript
Slide 1 of 19
So now, you're wondering, well, what is the scale the FDA is recommending? And it's Child-Pugh.
Slide 2 of 19
Where did this come from? Well, this scale which is now in every modern package insert was originally developed in 1964 to predict mortality during surgery in patients with advanced liver disease and was then modified in 1972 and it is used for prognostic information and necessity of liver transplantation. There are other scales which are also used on the liver transplant service such as MELD. But as FDA found out, Child-Pugh is perfect for our purposes in terms of assessing cirrhosis and the extent to which it alters drug metabolism.
References:
- Cholonguitas, E., Papatheodoridis, G. V., Vangeli, M., Terreni, N., Patch, D., & Burroughs, A. K. (2005). Systematic review: The model for end-stage liver disease – should it replace Child-Pugh's classification for assessing prognosis in cirrhosis? Alimentary Pharmacology and Therapeutics, 22(11-12), 1079-1089.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 19
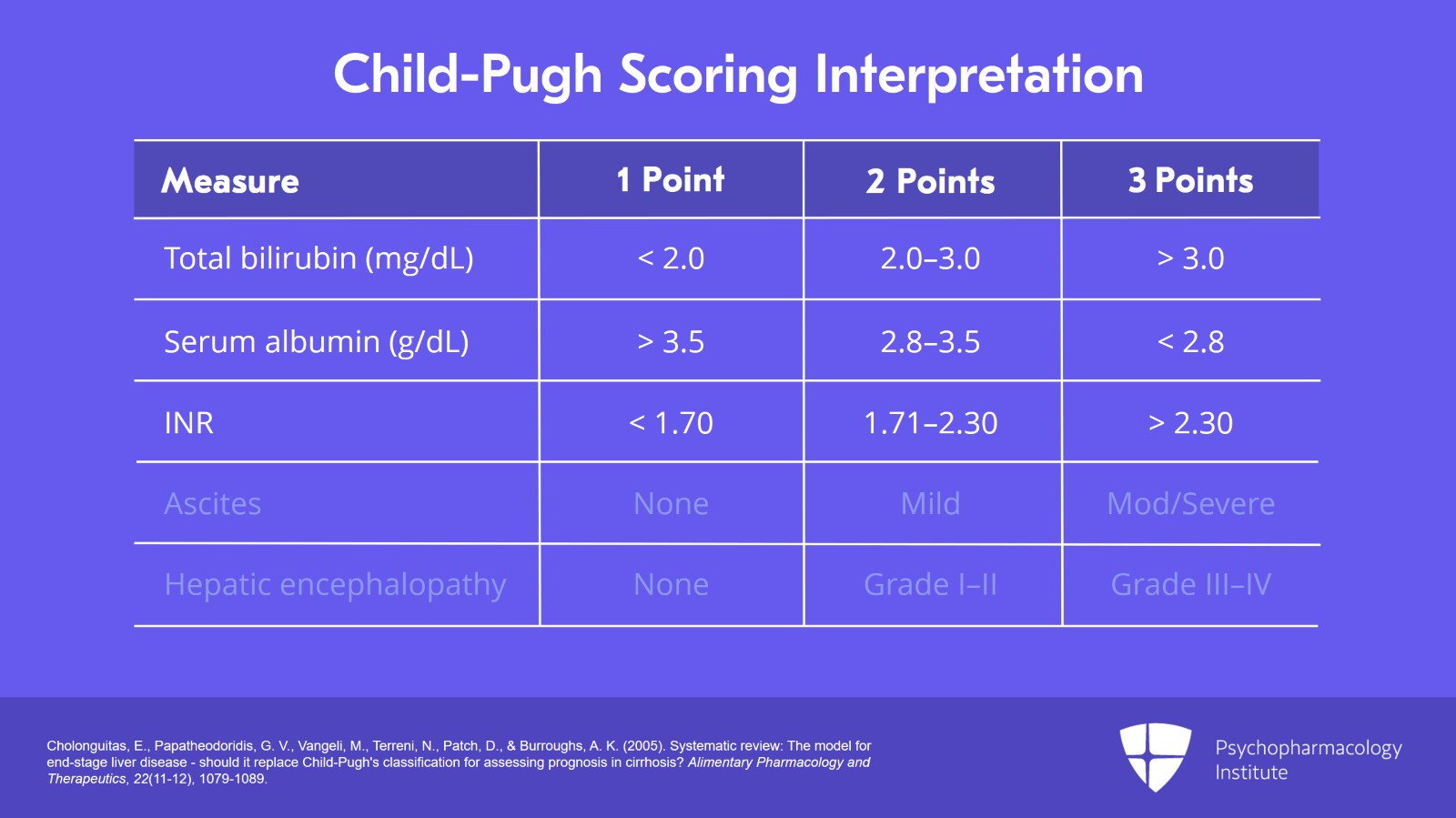
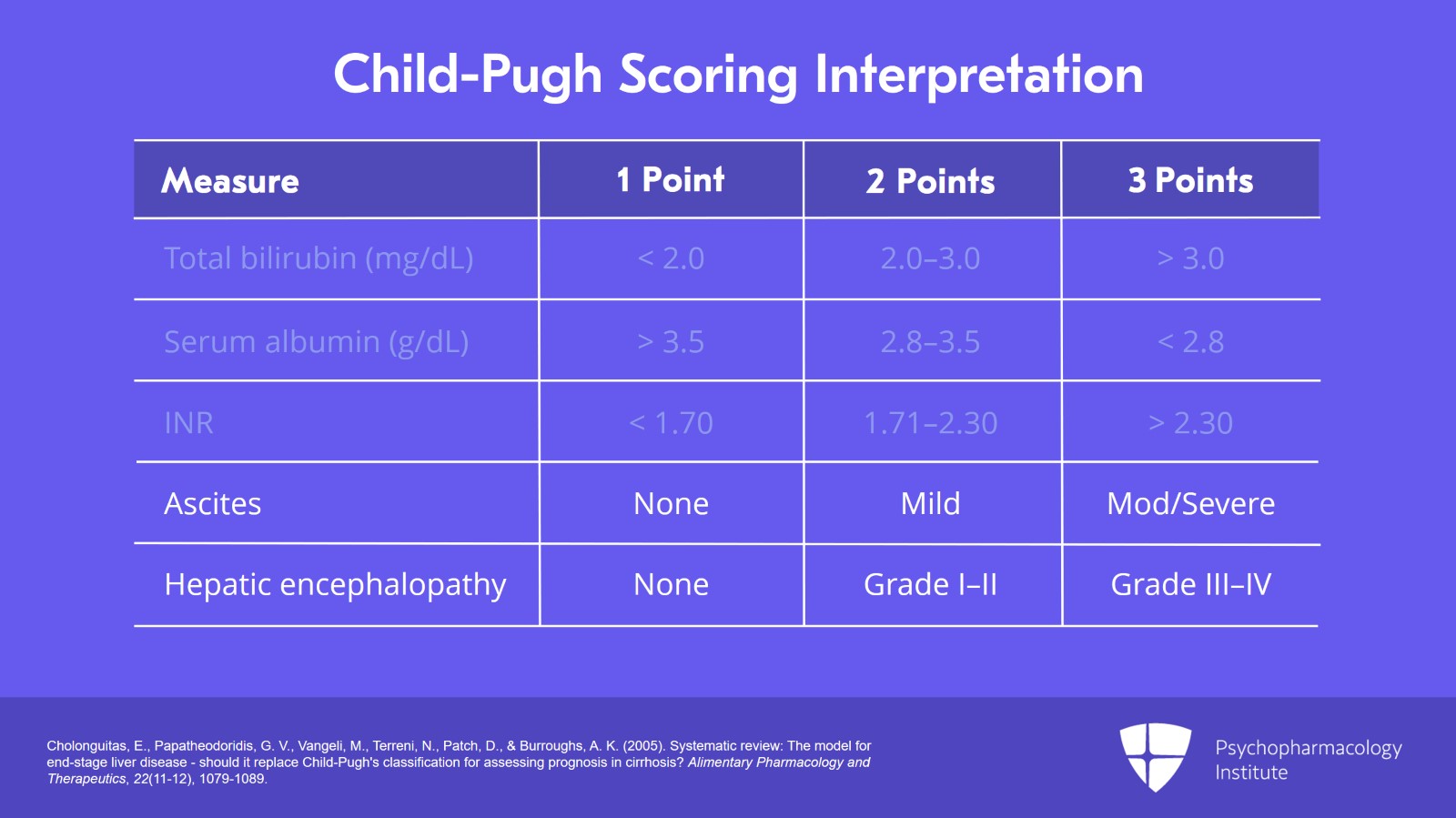
Here are the elements of the Child-Pugh rating scale. There are three labs: Bilirubin, albumin, and INR. INR is the international normalized ratio and that looks at your PT compared to standardized norms and converts it to a ratio. There are also two clinical criteria: Ascites and hepatic encephalopathy.
References:
- Cholonguitas, E., Papatheodoridis, G. V., Vangeli, M., Terreni, N., Patch, D., & Burroughs, A. K. (2005). Systematic review: The model for end-stage liver disease – should it replace Child-Pugh's classification for assessing prognosis in cirrhosis? Alimentary Pharmacology and Therapeutics, 22(11-12), 1079-1089.
Slide 4 of 19
It's important to notice that ALT, AST, GGT, alk phos are not part of the scoring system. And again, this is really the take-home message more than anything. The inflammatory markers have nothing to do with cirrhosis. It's the ability to make proteins, it's the clearance of bilirubin which best correlate with the extent of cirrhosis.
References:
- Cholonguitas, E., Papatheodoridis, G. V., Vangeli, M., Terreni, N., Patch, D., & Burroughs, A. K. (2005). Systematic review: The model for end-stage liver disease – should it replace Child-Pugh's classification for assessing prognosis in cirrhosis? Alimentary Pharmacology and Therapeutics, 22(11-12), 1079-1089.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 19
And here is the scoring system. You can see for the five elements, they are given 1, 2, or 3 points depending on severity. So, for total bilirubin, if you're less than 2, meaning a normal bilirubin, you get 1 point. If you're 2 to 3, you get 2 points. And if your bilirubin is greater than 3, you get 3 points. If your serum albumin is greater than 3.5 which is normal, you get 1 point. If it's from 2.8 to 3.5, you get 2 points. And if it's really low, less than 2.8, you get 3 points. INR, if it's less than 1.7, you get 1 point. If it's 1.71 to 2.30, you get 2 points. And if it's really elevated, greater than 2.3, you get 3 points.
References:
- Cholonguitas, E., Papatheodoridis, G. V., Vangeli, M., Terreni, N., Patch, D., & Burroughs, A. K. (2005). Systematic review: The model for end-stage liver disease – should it replace Child-Pugh's classification for assessing prognosis in cirrhosis? Alimentary Pharmacology and Therapeutics, 22(11-12), 1079-1089.
Slide 6 of 19
Ascites is graded as none, mild or severe. That's 1, 2 or 3 points. And hepatic encephalopathy, if there's none, you get 1 point. If it's grade 1 to 2, you get 2 points. And grades 3 and 4, you get 3 points. So, all you do is simply just add up the points. I actually have this bookmarked on my phone. You can look it up on Wikipedia if you want. All you need is just a table with the points and those three labs, total bilirubin, serum albumin and INR, as well as some appreciation of the clinical presence of ascites or hepatic encephalopathy.
References:
- Cholonguitas, E., Papatheodoridis, G. V., Vangeli, M., Terreni, N., Patch, D., & Burroughs, A. K. (2005). Systematic review: The model for end-stage liver disease – should it replace Child-Pugh's classification for assessing prognosis in cirrhosis? Alimentary Pharmacology and Therapeutics, 22(11-12), 1079-1089.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 19
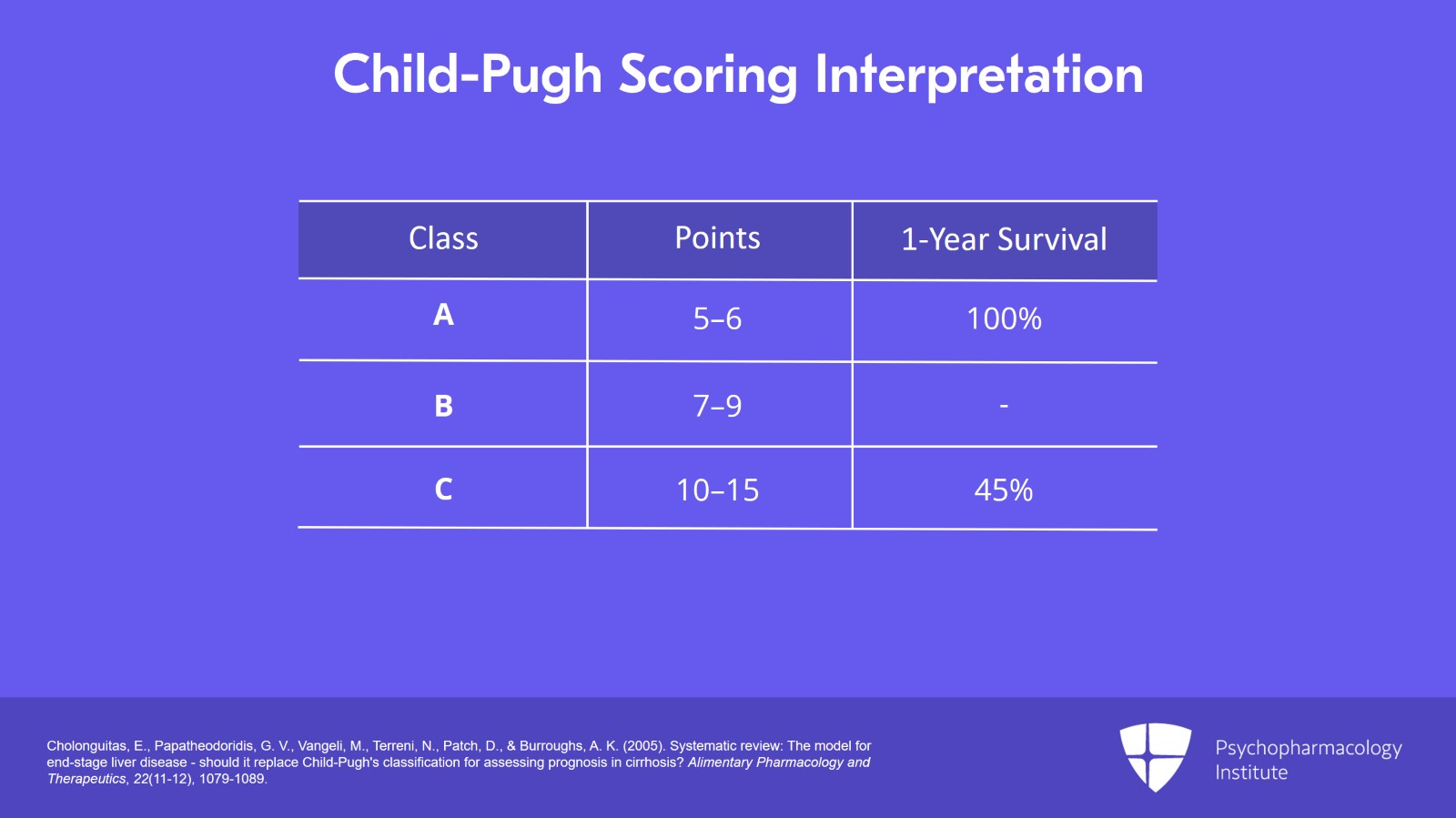
The Child-Pugh scoring interpretation adds up the points and says you're class A, B, or C. Class A is 5 to 6 points. Class B is 7 to 9 points. And class C is 10 to 15 points. Now, surprisingly, your survival goes down as you have more and more liver disease. And so, if you're class A, your one-year survival is 100%. If you're class C, it's 45%. So again, it's very important that you use this terminology, and it is now in the package inserts. Often, they'll say Child-Pugh moderate or Child-Pugh B, Child-Pugh C, or Child-Pugh severe. And very commonly, they actually will provide the points. They'll say if your Child-Pugh score is 10 to 15, this is what you should do. If it's 7 to 9, this is what you should do for that particular medication.
References:
- Cholonguitas, E., Papatheodoridis, G. V., Vangeli, M., Terreni, N., Patch, D., & Burroughs, A. K. (2005). Systematic review: The model for end-stage liver disease – should it replace Child-Pugh's classification for assessing prognosis in cirrhosis? Alimentary Pharmacology and Therapeutics, 22(11-12), 1079-1089.
Slide 8 of 19
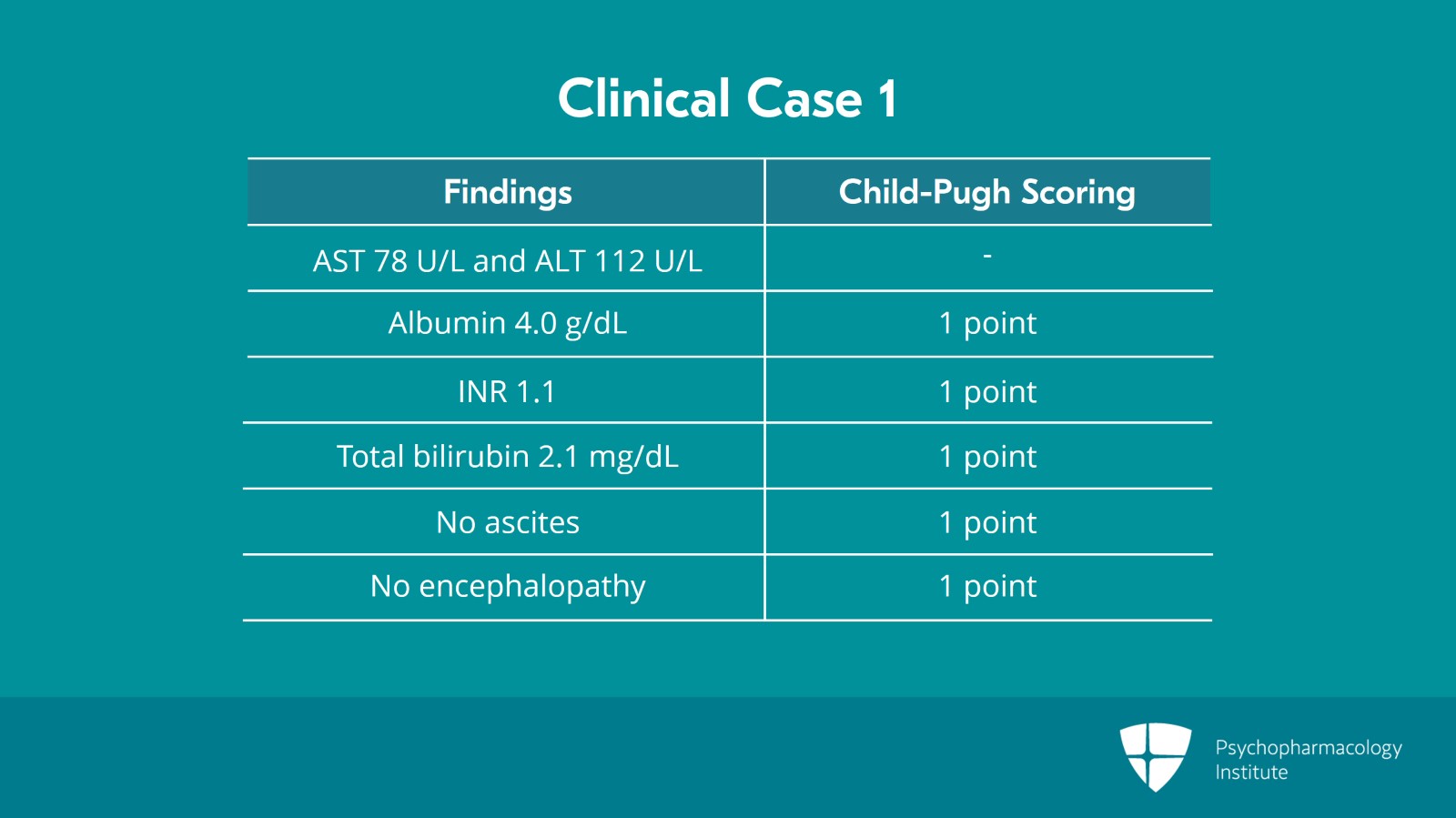
So, here's a couple of examples on how to use this in clinical practice. So here, we have an individual who is obese. You think they may have nonalcoholic fatty liver disease. You would like to put them on cariprazine for this particular person because she has bipolar depression.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 19
You get some labs. And you say, wow, that AST is high at 78 and the ALT is high at 112. There's a lot of inflammation there. But again, we go to Child-Pugh for determining whether or not we have to address drug dosages. Her albumin is normal at 4.0. She gets only 1 point for that. Her INR is normal at 1.1. She only gets 1 point for that. Her total bilirubin is 2.1. She only gets 1 point for that. She does not have ascites and she does not have hepatic encephalopathy.
Slide 10 of 19
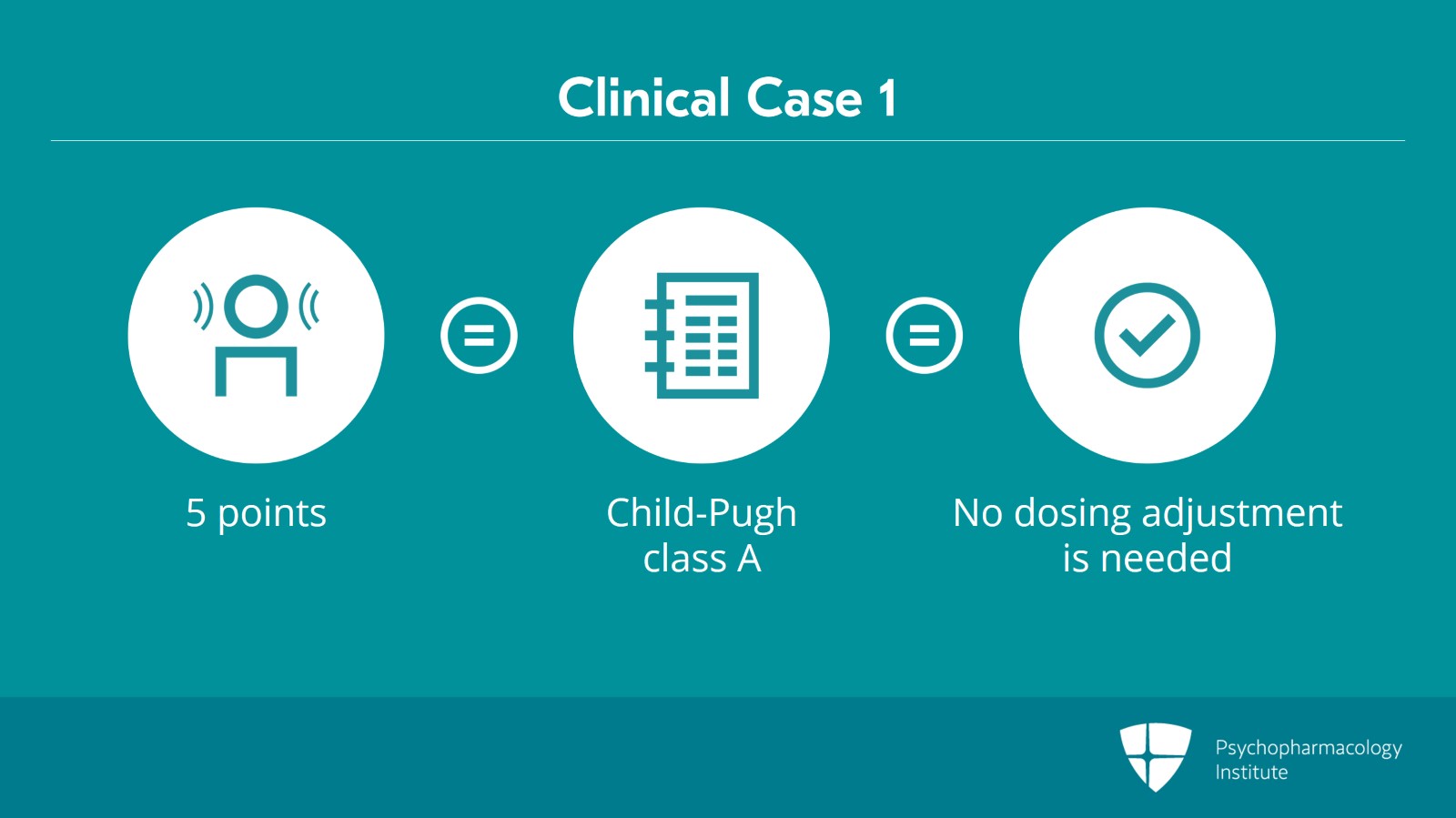
So, we add these all together. This patient has 5 total points. She very clearly is Child-Pugh A. Child-Pugh A means no dosing adjustment is needed and you can treat her the way you would treat any other patient with that antipsychotic.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 19
Here's a second example. An individual with schizophrenia who also has an untreated and ongoing alcohol use disorder comes in with psychosis to the inpatient unit and is still drinking. So, you have heard from your colleagues that because this person has some kind of liver disease that oral paliperidone should be used because it is "safe" for people with liver disease. So, somebody asks you about this and you say, you know, let's confirm this because I've heard a lecture about how to use Child-Pugh to determine whether medications can be used and what the appropriate dosage requirement is for people who have liver disease.
Slide 12 of 19
So, here's the labs for this gentleman. His AST and ALT are mildly abnormal at 56 and 66. But again, we add up the Child-Pugh points. His albumin is low at 3.0. He gets 3 points. His INR is elevated. He gets 2 points. His total bilirubin is normal, only 1 point. But he has ascites that's mild. He gets 2 points. And he has grade 1 hepatic encephalopathy, 2 points.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 13 of 19
So, we add up all of these points and it turns out that This patient has 10 total points. This gentleman is Child-Pugh C. He has advanced cirrhosis. He has severe hepatic impairment.
Slide 14 of 19
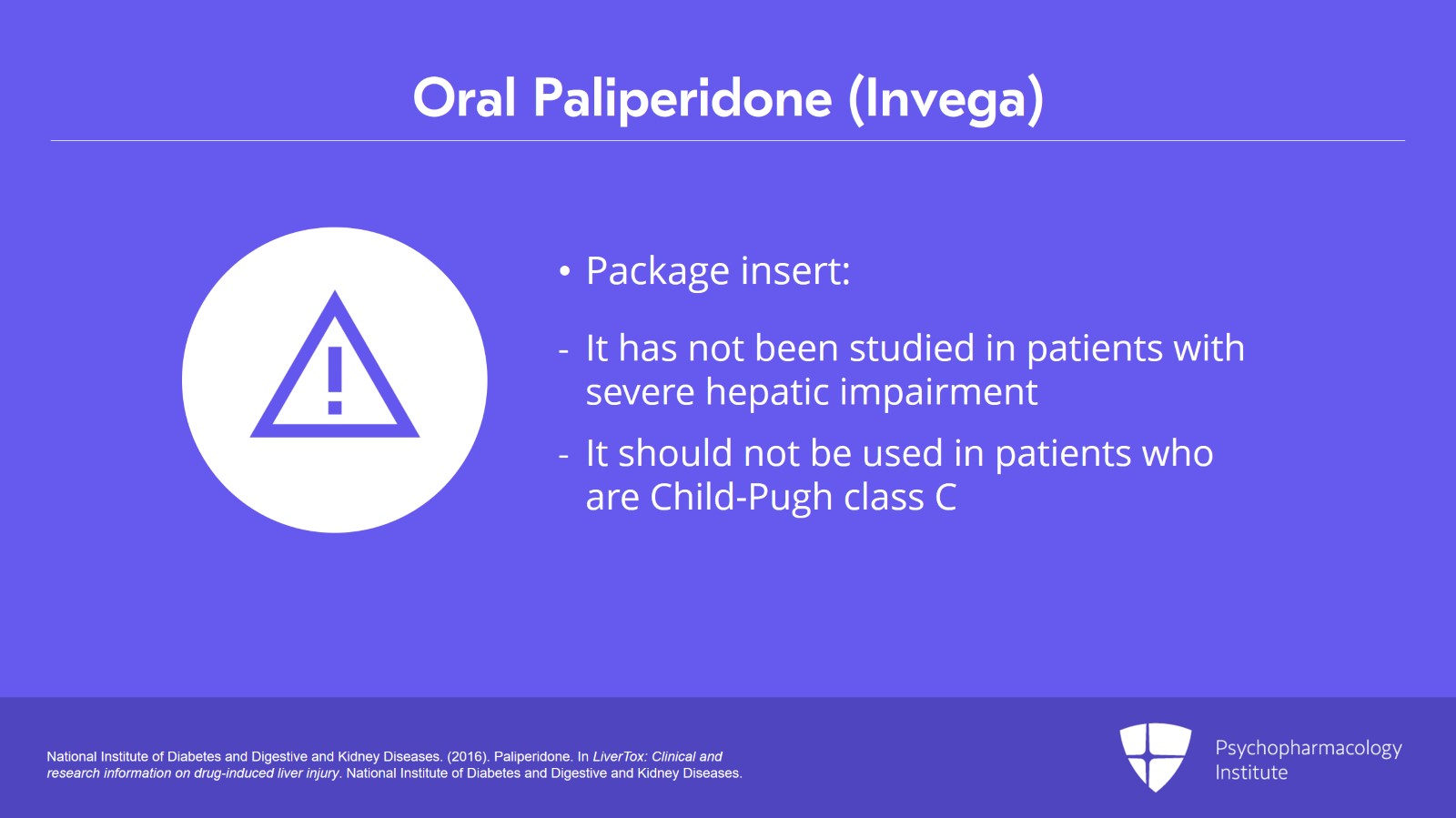
So, what shall we do? Can we use oral paliperidone? The best source of information for specific medications especially those which have been approved in the last 10 to 15 years is to go to the package insert. And the package insert for paliperidone clearly states that it has not been studied in patients with severe hepatic impairment. People with Child-Pugh class C have severe hepatic impairment. It has not been studied. And therefore, it should not be used.
References:
- National Institute of Diabetes and Digestive and Kidney Diseases. (2016). Paliperidone. In LiverTox: Clinical and research information on drug-induced liver injury. National Institute of Diabetes and Digestive and Kidney Diseases. 14
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 15 of 19
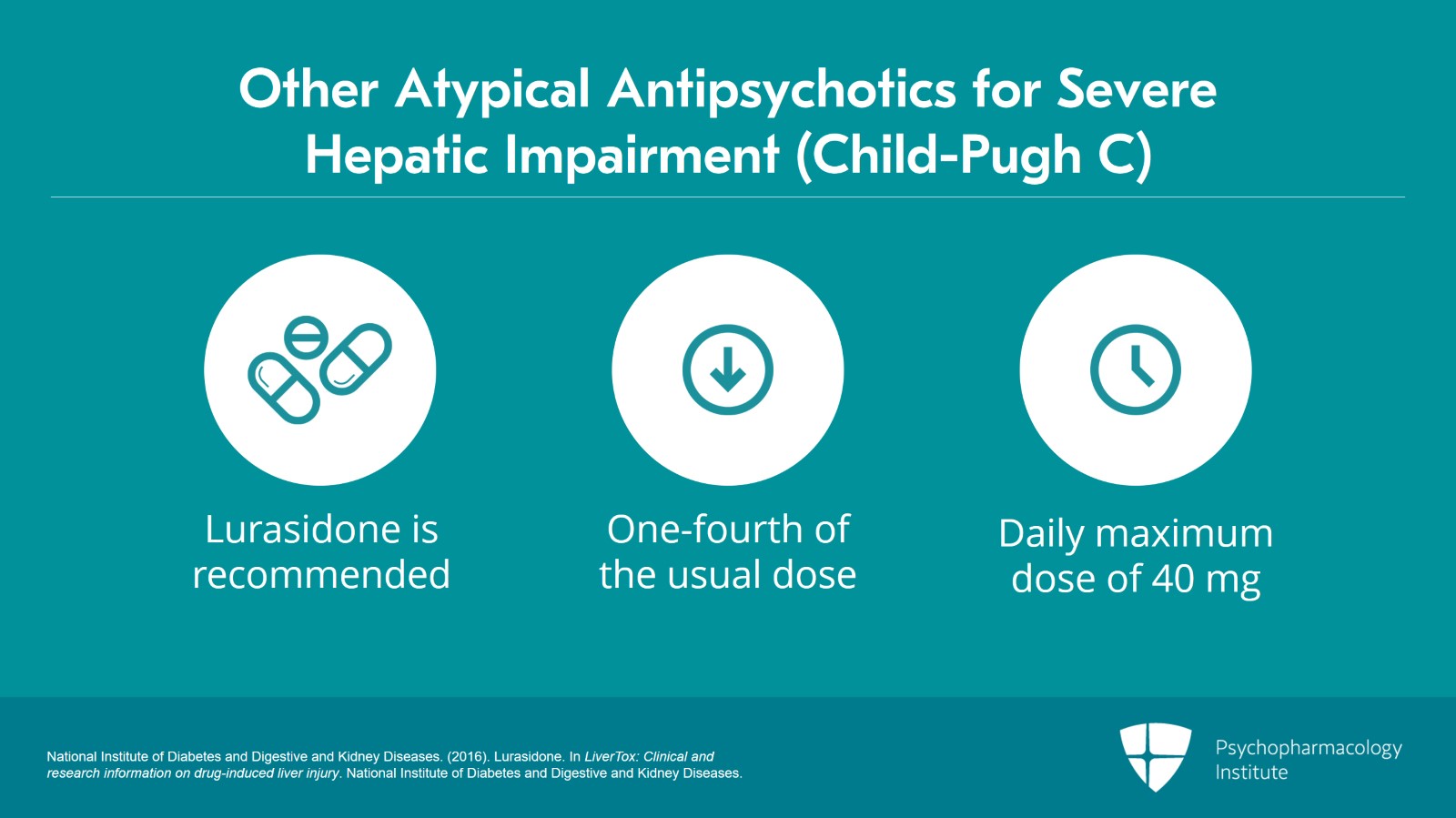
Are there other options? Well, you just have to go through the package inserts and see which medications provide guidance for initial dosing in patients who are Child-Pugh C. Lurasidone is one where they say very clearly if you're Child-Pugh C you can use lurasidone but the recommended doses are 1/4 of the usual dose with the daily maximum of 40 mg given with food.
References:
- National Institute of Diabetes and Digestive and Kidney Diseases. (2016). Lurasidone. In LiverTox: Clinical and research information on drug-induced liver injury. National Institute of Diabetes and Digestive and Kidney Diseases. 15
Slide 16 of 19
So again, it's the Child-Pugh scale, it's not AST or ALT, which determines whether a patient needs dose reduction or whether the medication can be given at all. Whether the medication can be given really will be determined primarily by what's also in the package insert.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 17 of 19
And the labs for Child-Pugh are bilirubin, serum albumin, and INR. AST and ALT have nothing to do with cirrhosis. They have to do with inflammation.
Slide 18 of 19
The other situation which might arise, this is an important point is that you have somebody who's already on a stable psychotropic dosage. No adverse effect. The question is: Do I need to adjust their dose now based upon their Child-Pugh stage? And generally, the answer is if the hepatic function has not deteriorated, you can leave them where they are at. But if there's clearly been a change, they're now Child-Pugh B and they used to be A or they're now Child-Pugh C and they used to be B, well, in those instances, it may be appropriate to reduce the drug exposure particularly if side effects are present. In those circumstances, getting drug levels may be your best guide to what would be an appropriate dose for that particular patient in the new context of the more advanced liver disease.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.