Slides and Transcript
Slide 1 of 11
Colleagues, I’d like to suggest that no conversation about depression in older adults is really complete without a consideration of bereavement and terminal illness.
Slide 2 of 11
All of us know that the loss of a loved one is particularly likely to occur later in life and that attachment bereavements can become an occasion for the development of major depression just as patients who are confronting terminal illness very frequently experience some degree of depression.
In recent years, we’ve learned a good deal about the intersection of major depression in older adults with issues related to bereavement and with issues related to terminal illness and its management by palliative and supportive care physicians.
Just on a personal note, I would like to say that one of the most enjoyable and, for me, gratifying parts of my own clinical practice has been the collaborative care that I’ve undertaken with colleagues who specialize in Palliative and Supportive Care Medicine. There is indeed a profound intersection or interplay between Palliative and Supportive Care Medicine on the one hand and Geriatric Psychiatry, geriatric mental health on the other.
References:
- Reynolds, C. F. (2017). Evidence-Based Treatment and Prevention of Major Depressive Episodes in Later Life. In Halter, J. B., Ouslander, J. G., Studenski, S., High, K. P., Asthana, S., Supiano, M. A., Ritchie C. (Eds.), Hazzard's geriatric medicine and gerontology (7th ed., pp. 1071–1088). essay, McGraw-Hill Education Medical.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 11
I’d like to cut to the chase here and really emphasize I think where the science has been most impactful. We’ve learned a great deal about what has come to be called complicated grief or in the parlance of the International Classification of Disorders, the ICD-11, prolonged grief disorder. We know that about 10% of people across the life cycle but particularly in late life who have experienced the loss of a loved one develop prolonged grief.
It’s as if the work of grief is somehow sidetracked and they become stuck as it were in the throes of acute grief unable to come to terms with the loss of a loved one, unable to re-imagine and undertake a life without the loved one, to find meaning and pleasure and satisfaction in life without the loved one that they have lost.
References:
- Reynolds, C. F. (2017). Evidence-Based Treatment and Prevention of Major Depressive Episodes in Later Life. In Halter, J. B., Ouslander, J. G., Studenski, S., High, K. P., Asthana, S., Supiano, M. A., Ritchie C. (Eds.), Hazzard's geriatric medicine and gerontology (7th ed., pp. 1071–1088). essay, McGraw-Hill Education Medical.
Slide 4 of 11
I refer you particularly to DSM-5. You will find in the appendix in section 3, Provisional Criteria for Persistent Complex Bereavement Disorder, PCBD. And I would refer you also to ICD-11 where you will find diagnostic guidelines for the assessment of people living with prolonged grief disorder.
The essence of prolonged grief disorder is persistent yearning and longing for the person who has died and intense preoccupation with the circumstances of the death and intense emotional pain.
Of relevance to this series of talks is the fact that prolonged grief disorder frequently co-occurs with major depressive disorder but is not the same thing as major depressive disorder. It also frequently co-occurs with posttraumatic stress disorder.
References:
- Reynolds, C. F. (2017). Evidence-Based Treatment and Prevention of Major Depressive Episodes in Later Life. In Halter, J. B., Ouslander, J. G., Studenski, S., High, K. P., Asthana, S., Supiano, M. A., Ritchie C. (Eds.), Hazzard's geriatric medicine and gerontology (7th ed., pp. 1071–1088). essay, McGraw-Hill Education Medical.
- Shear, K., Frank, E., Houck, P. R., & Reynolds, C. F. (2005). Treatment of complicated grief. JAMA, 293(21), 2601.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 11
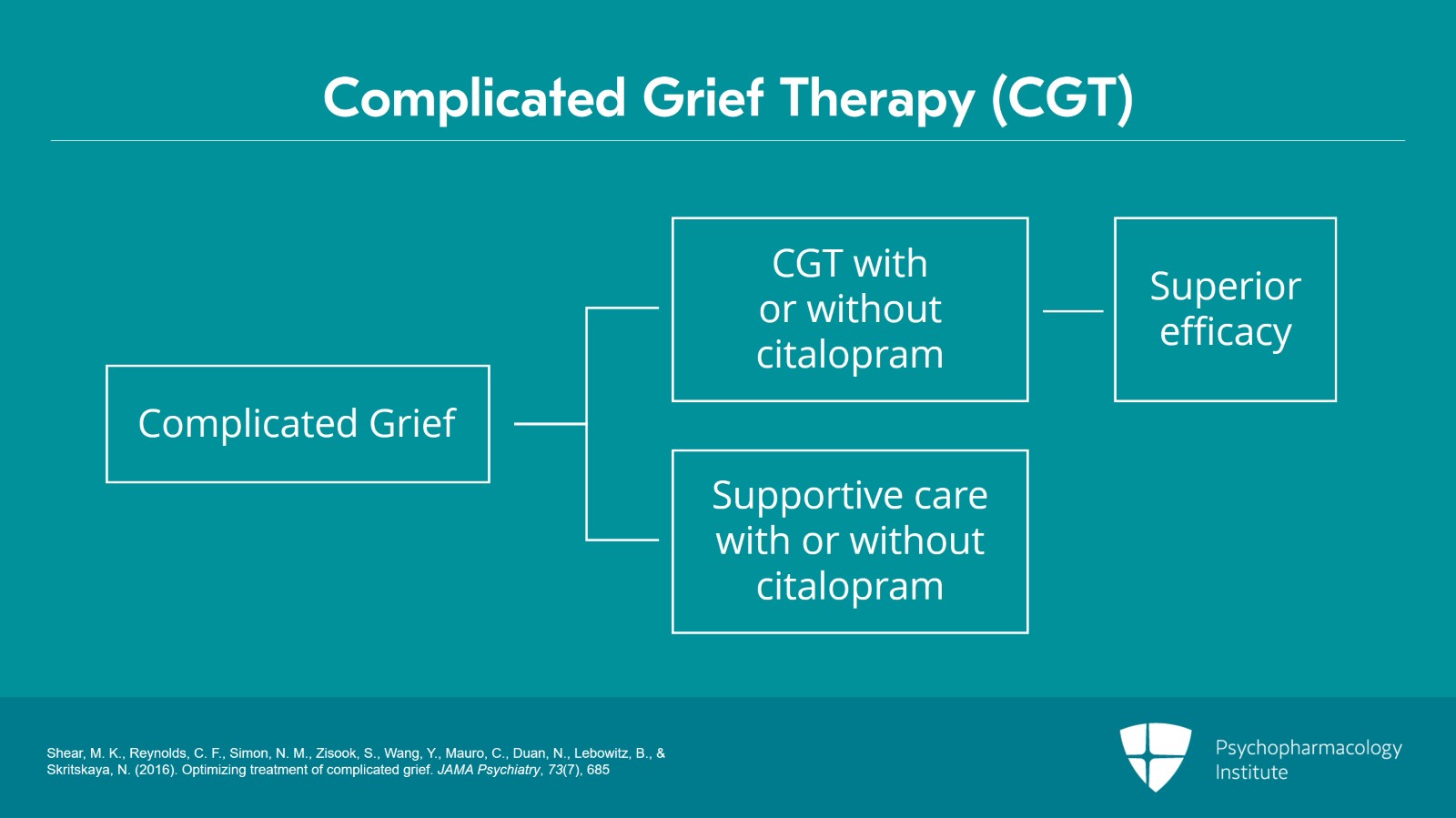
I’d like to refer you to what I think, if you’ll allow me, will be a landmark clinical trial, a multisite NIMH-sponsored clinical trial of complicated grief psychotherapy. That study was published in 2016 in JAMA Psychiatry and showed the superior efficacy of complicated grief psychotherapy with or without citalopram for the relief of the symptoms of complicated grief.
Patients who were randomly assigned to supportive care with or without antidepressant medication with citalopram did not do nearly as well as those who received complicated grief psychotherapy.
References:
- Shear, M. K., Reynolds, C. F., Simon, N. M., Zisook, S., Wang, Y., Mauro, C., Duan, N., Lebowitz, B., & Skritskaya, N. (2016). Optimizing treatment of complicated grief. JAMA Psychiatry, 73(7), 685
Slide 6 of 11
What was particularly interesting to me as someone interested in the diagnosis and I’ve been involved with the DSM process for many years at this point is that depression-specific treatments such as IPT or antidepressant medication simply do not do nearly as well in the setting of complicated grief as does the depression-specific psychotherapy developed by Kathy Shear for this condition, complicated grief therapy or CGT as it is sometimes called.
References:
- Shear, K., Frank, E., Houck, P. R., & Reynolds, C. F. (2005). Treatment of complicated grief. JAMA, 293(21), 2601.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 11
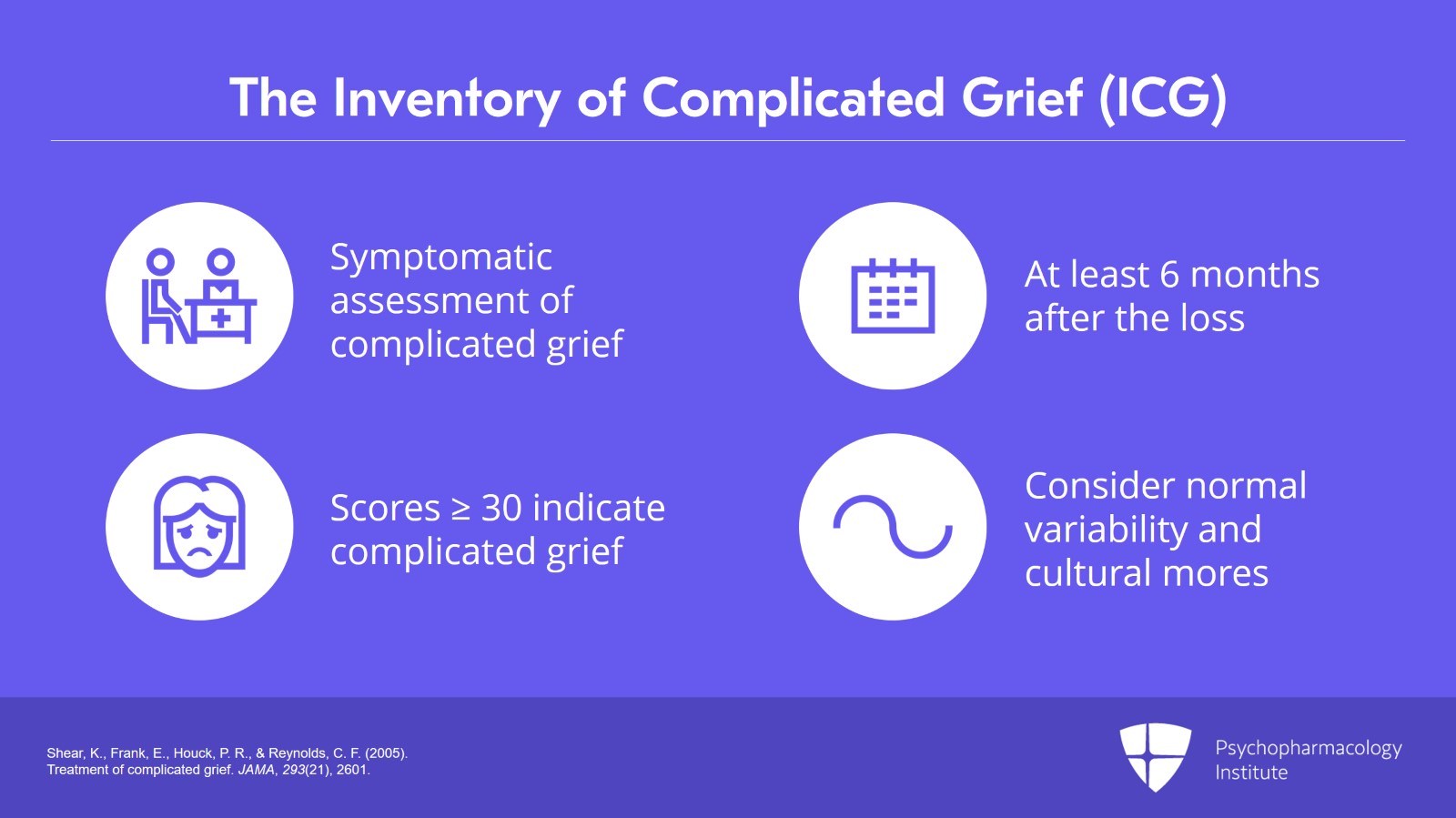
I’d like also to give a shoutout here to my colleague, Holly Prigerson, who developed the Inventory of Complicated Grief, the ICG.
The Inventory of Complicated Grief remains the industry standard, if you will allow me to use that phrase, for symptomatic assessment of complicated grief as long as the symptoms are assessed six months or longer after the death of the loved person.
Scores typically of 30 or above indicate its presence particularly or I should say only in someone who is at least six months after the loss of the loved one.
The DSM and the ICD do not support the diagnosis of complicated or prolonged grief until at least six months after the loss and in keeping with normal variability in the course of grief as well as with the cultural mores that determine the expression of grief.
References:
- Shear, K., Frank, E., Houck, P. R., & Reynolds, C. F. (2005). Treatment of complicated grief. JAMA, 293(21), 2601.
Slide 8 of 11
The point that I would like to make before closing out this section with respect to depression in the context of terminal illness is that there has been I think an increasing interest in the use of psychostimulant medications such as methylphenidate to promptly relieve the symptoms of depression in patients who are dying or whose death is imminent allowing them to have a more comfortable passage and perhaps thereby as well to engage with loved ones in the process of saying goodbye.
There’s also a large literature on the use of other types of specific counseling particularly those that address life’s meaning, issues of gratitude and the life that one has led and other spiritual types of issues.
References:
- Reynolds, C. F. (2017). Evidence-Based Treatment and Prevention of Major Depressive Episodes in Later Life. In Halter, J. B., Ouslander, J. G., Studenski, S., High, K. P., Asthana, S., Supiano, M. A., Ritchie C. (Eds.), Hazzard's geriatric medicine and gerontology (7th ed., pp. 1071–1088). essay, McGraw-Hill Education Medical.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 11
So to summarize key points, I think in what is a very interesting and frankly very complex area in psychiatric research we have learned that prolonged or complicated grief is distinct from depression, very much distinct from depression in terms of the types of interventions that it responds to.
It frequently is accompanied by major depression in older adults as well as earlier in the life cycle and occurs in about 10% of persons who have lost a loved one whether it be a spouse or a child, an off-time loss and it is a particularly difficult issue in patients who have lost a loved one to suicide or to homicide.
Slide 10 of 11
Prolonged grief can be assessed well with the Inventory of Complicated Grief, the ICG, at least six months after the loss of the loved one. The ICD-11 allows flexibility on this point in different countries and in different cultural settings because in some countries and settings it may be inappropriate to diagnose a complicated or prolonged grief until at least 12 months have passed.
Prolonged grief disorder responds well to a specific type of CBT-based treatment called complicated grief therapy.
And finally, depression in the setting of terminal illness may be alleviated by the use of psychostimulant medication allowing the passage to be kinder and gentler, allowing the patient to say goodbye or to engage briefly in more spiritually oriented forms of counseling.
Thank you.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.