Slides and Transcript
Slide 1 of 10
In this video, we’re going to talk about cognitive impairment and sexual problems with lithium, two important areas that involve the issues of dosing, of managing and dealing with people’s willingness to take it.
Slide 2 of 10
So let’s start with cognitive impairment. First of all, lithium has many advantages for cognition and brain function. And I mentioned it in a previous video but I would refer you to an article that I currently have out in the Psychiatric Times which many of you may get, the February 2020 issue. I have a whole article on the neuroprotective effects of lithium and how lithium improves brain functioning and cognition rather impressively and is a strong argument for why people should take it. It does things that are positive in terms of brain functioning and even cell volumes improve that are diminished by the disease by lithium that none of the other anti-manic and bipolar medications do. So it’s a big argument actually for taking lithium. But still, many patients complain of cognitive impairment. So what’s the evidence on that?
References:
- Gerhard, T., Devanand, D. P., Huang, C., Crystal, S., & Olfson, M. (2015). Lithium treatment and risk for dementia in adults with bipolar disorder: population-based cohort study. The British Journal of Psychiatry, 207(1), 46-51.
- https://www.psychiatrictimes.com/bipolar-disorder/neuroprotective-effects-lithium
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 10
Well, there have been neuropsychological testing done. And actually, the testing shows only minor and probably clinically insignificant cognitive impairment from lithium. So why are the complaints so strong? Well, we think it’s things like the loss of that highly creative thinking associated with their manias. They’re not having those highs where they really feel very brilliant, on top of the world, that they can do anything, that their ideas are better than anybody else’s. Now, they may be getting opposition from some others for these supposedly great ideas and they just try to run roughshod over those people or have big arguments with them about it and it’s got to be my way, not the other way. But they think they’re having brilliant ideas. And suddenly, that’s not happening after lithium. So it feels like their brain is not working. They feel they’ve been zombified, turned into an even-keel personality that to them is not the self that they want to be.
So this is a very important area for discussion with patients. It should be brought up right when you begin to prescribe. I do it routinely. I tell them that this is going to happen, that they’re going to have a loss of some of that great feeling that they get especially about their thinking. And I ask them, are they ready for that, so that they can anticipate it, so it wouldn’t come as a shock and surprise when suddenly this happens. And they on their own decide not to take it and come back here and say, no way, that’ll turn me into a zombie. I’m not taking it. That may go on for 10 or 15 years while clinicians go through the whole gamut of everything we have in our repertoire without any great success. And that’s often when a consult gets put in and I see them and I think it’s time to reconsider lithium. And then we can often persuade them. But meanwhile, they’ve lost 10 or 15 years of trying all these other things that didn’t work. Anyway, so that highly creative thinking.
References:
- Wingo, A. P., Wingo, T. S., Harvey, P. D., & Baldessarini, R. J. (2009). Effects of lithium on cognitive performance: a meta-analysis. In Database of Abstracts of Reviews of Effects (DARE): Quality-assessed Reviews [Internet]. Centre for Reviews and Dissemination (UK).
Slide 4 of 10
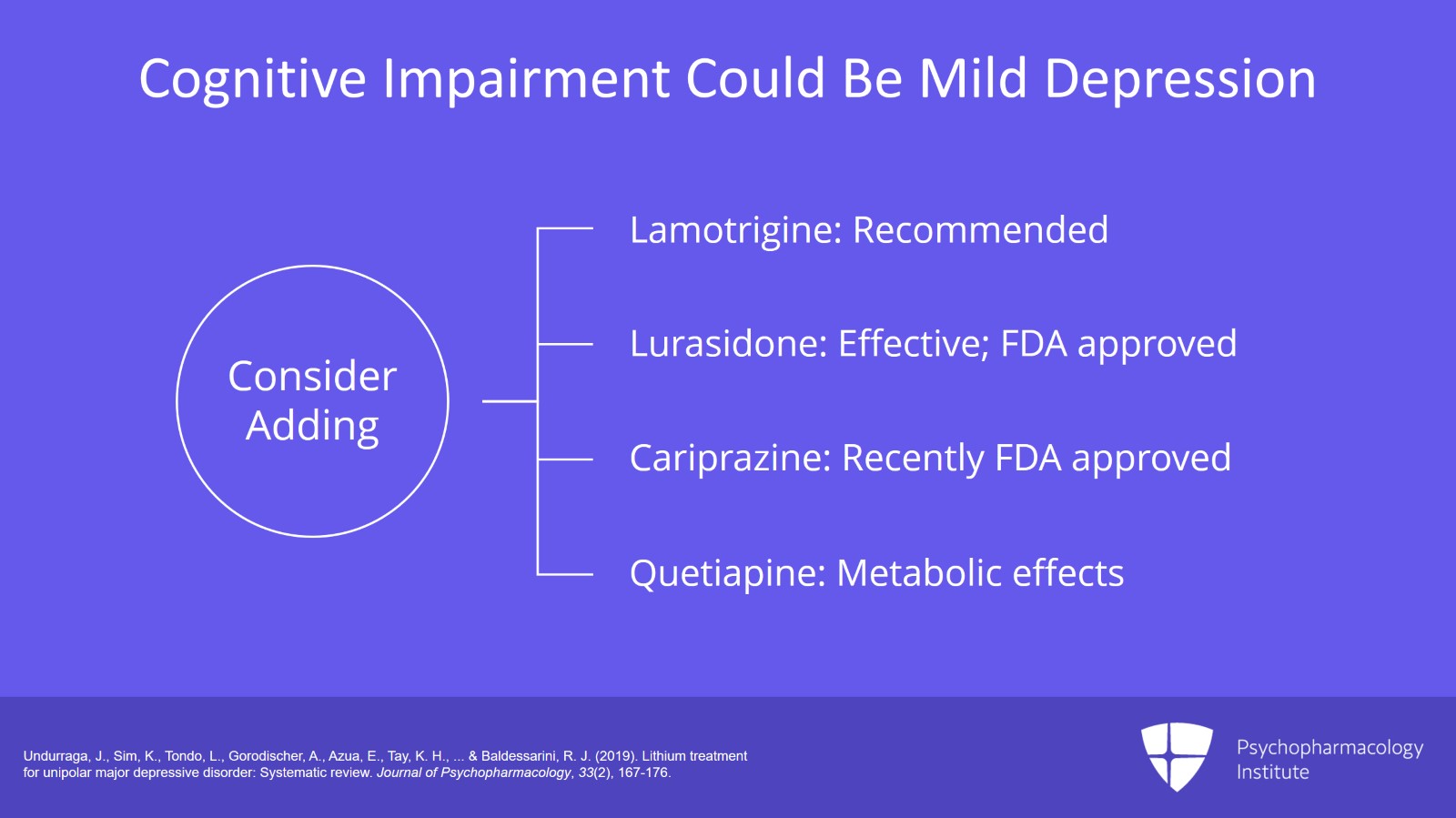
Now, for others, the cognitive problem is that they actually get stuck in a mild depression. It’s not euthymia. It’s actually mild depression. Lithium is not as good for managing the depressed phase of bipolar. And they may get stuck in something a little below par for that. They’re sleeping a little longer than usual. Their brain is indeed slower than their median or best optimal brain. And you may have to add a supplemental treatment for the depressed phase of covering that to add to the lithium.
We usually recommend lamotrigine, maybe lurasidone. Cariprazine is recently approved by the FDA, our newest treatment for bipolar depression. Quetiapine is also good. That’s been around for a while. Quetiapine has more metabolic side effects. I don’t usually turn to it first because they’re usually getting at least some of that from lithium and then they may have more compounding of that with quetiapine. So it does work for bipolar depression but I might try those other things first.
Lurasidone has an FDA approval and good studies showing that adding it to lithium is better than adding placebo as well as monotherapy studies showing that lurasidone is effective for mild depression. So you should be ready with your options. So this is going to be a major cause of nonadherence though. People not liking this cognitive impairment and you need to be ready with your education about it and your options for treatment of the various possible causes.
References:
- Undurraga, J., Sim, K., Tondo, L., Gorodischer, A., Azua, E., Tay, K. H., … & Baldessarini, R. J. (2019). Lithium treatment for unipolar major depressive disorder: Systematic review. Journal of Psychopharmacology, 33(2), 167-176.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 10
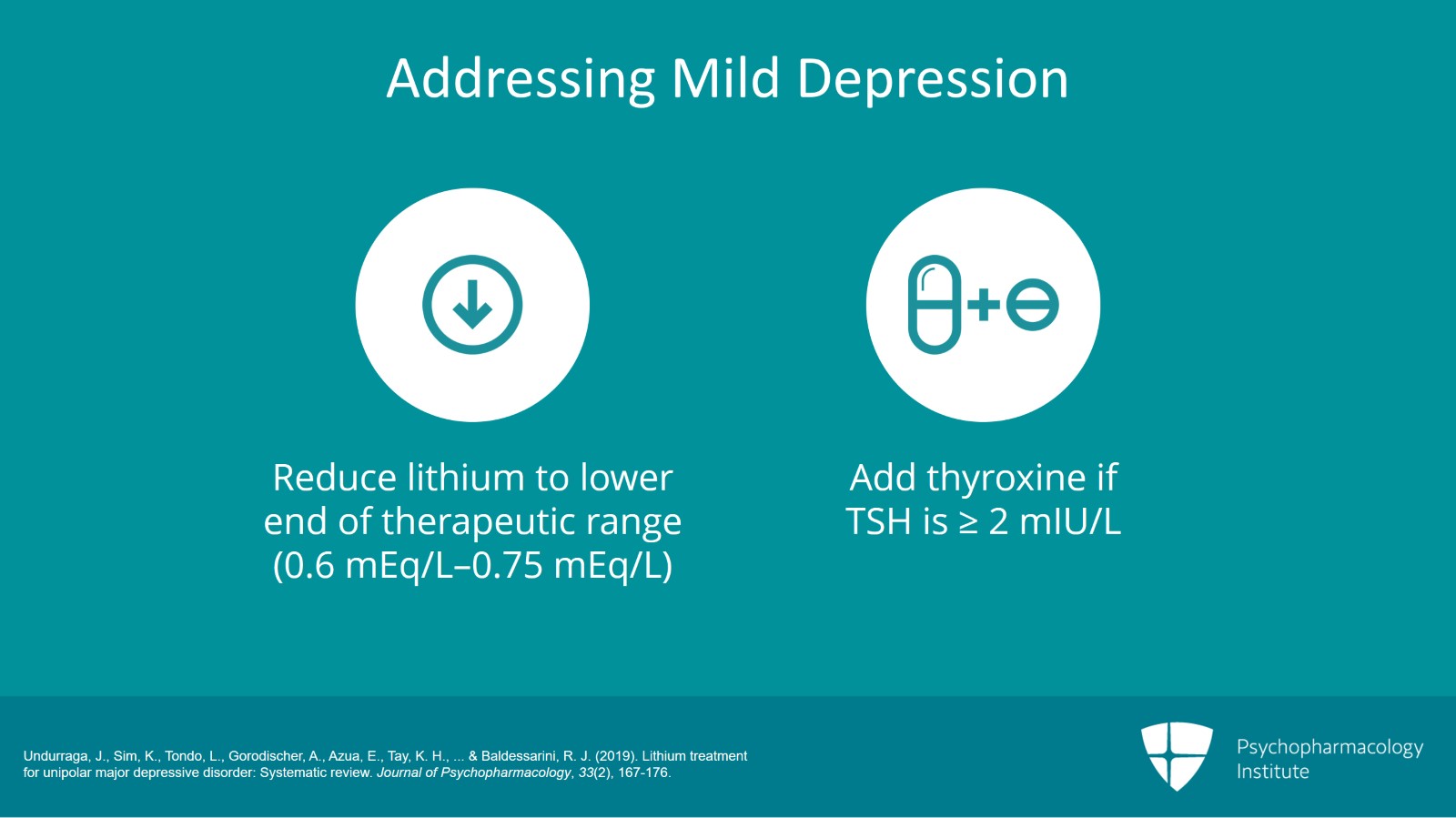
Now, you can try reducing the dose to the lower end of the therapeutic range if needed if you aren’t there already; 0.6 to 0.75 is the optimal maintenance dosage range for lithium as I’ve indicated in all the previous videos. I keep repeating that key preferred blood level range at 12-hour trough for lithium.
Now, you also can add thyroid if their thyroid function is not optimal. Let’s say that your TSH is 2 or higher. As we’ve discussed in previous videos, if it’s 2 or higher, they may need some T4 added in to help with this mild depression.
References:
- Undurraga, J., Sim, K., Tondo, L., Gorodischer, A., Azua, E., Tay, K. H., … & Baldessarini, R. J. (2019). Lithium treatment for unipolar major depressive disorder: Systematic review. Journal of Psychopharmacology, 33(2), 167-176.
Slide 6 of 10
I do not use antidepressants though. You’ll have to refer to our bipolar depression algorithm if you need to but antidepressants for the most part do not work in bipolar depression and they cause more cycling. Indeed, the STEP-BD study, NIMH-sponsored large-scale study monitoring a group of several thousand bipolar patients over years, in one of their studies, they found that adding an antidepressant for depression in bipolar depression triples the number of depressions they’re going to have going forward from that compared to if they weren’t given an antidepressant. I know there’s a lot of antidepressants still being used out there but it’s not where the evidence is. So yes, you’ll be in this position where patients are saying that they have cognitive impairment. You determined that it’s mild depression. So you need to be ready with your algorithm for managing. According to the evidence base, best treatments we have for those mild depressions are with add-ons to the lithium. And many of those treatments by the way actually have studies for evidence of add-on to lithium.
References:
- Perlis, R. H., Dennehy, E. B., Miklowitz, D. J., DelBello, M. P., Ostacher, M., Calabrese, J. R., … & Nierenberg, A. A. (2009). Retrospective age at onset of bipolar disorder and outcome during two‐year follow‐up: results from the STEP‐BD study. Bipolar disorders, 11(4), 391-400.
- El-Mallakh RS, Vohringer PA, Ostracher MM et al. Antidepressants worsen rapid cycling course in bipolar depression: A STEP-BD randomized clinical trial. J Affect Disord 2015;184:318-321
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 10
All right. So moving to the second problem I’m discussing in this video and that is sexual problems.
Now, we think of some of the other treatments we give in Psychiatry as more likely to cause sexual problems. Certainly, the SSRIs and SNRIs are very well known for their erectile dysfunction, delayed ejaculation, loss of libido and so on. And some of the antipsychotics especially those that elevate prolactin, drugs like risperidone, first-generation antipsychotics, paliperidone, these all cause prolactin elevation which is associated with significant sexual dysfunction. So maybe we don’t have lithium on the top of our list of drugs that we will immediately wonder if it’s a cause.
So I would say that when you encounter this with your patients and it’s not explained by one of the other drugs that they’re on and it’s not due to a comorbid medical illness or an ongoing serious substance use disorder, if you’ve dealt with all of that and they still seem to have it from the lithium, then I think you could agree that it could be from the lithium. So what could we do about that? Well, actually, there is one small study using, get ready for this, acetylsalicylic acid. Acetylsalicylic acid at a dose of 240 mg a day, a little lower dose than one tablet was found useful in one controlled study in 2013 that I cite in the printed version of this lecture. So you could try that for the sexual side effects of lithium.
Now, what else could you do? You could certainly lower lithium within the maintenance range as we’ve discussed as a strategy for almost all the other side effects we’ve reviewed.
References:
- Saroukhani, S., Emami‐Parsa, M., Modabbernia, A., Ashrafi, M., Farokhnia, M., Hajiaghaee, R., & Akhondzadeh, S. (2013). Aspirin for treatment of lithium‐associated sexual dysfunction in men: randomized double‐blind placebo‐controlled study. Bipolar disorders, 15(6), 650-656.
Slide 8 of 10
You could eliminate other causes of sexual dysfunction. I didn’t talk about non-psychiatric drugs that could cause sexual dysfunction but there are the antihypertensives that are famous for that and they may need to be changed to different ones in consultation with their primary care. Another option for dealing with it is consider having sex at the time of the lowest lithium level. Like if they’re on their lithium once a day at night, their lithium level will be lowest just before they take that night dose so that would be perhaps a good time to see if the sexual function is perhaps better rather than taking the lithium and then having sex an hour or two later. So you want again to have them on that regular release formulation at night and taking it after the attempt at sexual function.
I suppose if the sex problem is not due to lithium or any of those drugs, it could be due to psychological issues and the relationship of course and whether they should be referred for appropriate evaluation of that including sex therapy would certainly be a consideration. And finally, last but not the least, we always have sildenafil. It seems to work for a wide variety of sex problems caused by drugs or not caused by drugs. It definitely works for sex problems caused by SSRIs and SNRIs. Whether it would help with sex problems from lithium I don’t know but it’s possible.
References:
- Elnazer, H. Y., Sampson, A., & Baldwin, D. (2015). Lithium and sexual dysfunction: an under‐researched area. Human Psychopharmacology: Clinical and Experimental, 30(2), 66-69.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 10
So the key points of this video are: Patients complain of cognitive impairment. This was assumed to be real by expert clinicians for years until relatively recent objective neuropsychological studies have failed to verify much impairment. So it may be that this impairment is coming from other causes like loss of the sharp thinking associated with the manias or mild persisting depressions. Education that patients should expect this possible effect can head off abrupt discontinuation impulses by patients later hopefully.
Second and perhaps underemphasized side effect from lithium is sexual dysfunction. We’re much more familiar with this side effect from many other of the drugs we give. But some evidence has emerged that lithium can cause it which I discussed in detail. Further research is needed. But for dealing with it, you could try eliminating the other drugs that are more likely to cause it, try lowering lithium dose. Time the sex to lithium before they take their 24-hour once-a-day immediate release formulation of lithium so that lithium is at its 24-hour lowest trough level. Or consider sildenafil or consider this one study where they tried acetylsalicylic acid 240, one small study that showed that. It needs replication of course.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.