Slides and Transcript
Slide 1 of 6
Our next section is going to talk about longer term treatment issues in older age bipolar disorder specifically the issues of maintenance and adherence.
Slide 2 of 6
Now, if you remember from the slide I showed you a little ways earlier in the lecture, there are a variety of medications that are FDA approved for either longer term or maintenance treatment with bipolar disorder. None of them to the best of my knowledge have specifically been tested in older people where the focus is on outcomes in older people.
And so I think at this point we just sort of have to extrapolate. But one big issue that we have to be concerned about is adherence with medications. So in the old days, we used to call that compliance. Compliance is no longer the preferred term. Adherence is a term that applies a little more sort of shared decision making hopefully.
That’s our goal between clinicians who prescribe medications and patients who take medications that we would make those treatment decisions together and buy in with taking medications will just be better. So if we think about our previous case with Marie, I suggested that just simply telling Marie she needs to go back to a higher dose of medication even if she has burdensome side effects is probably not going to go over super well and will not promote adherence.
References:
- Sajatovic, M., Blow, F. C., Kales, H. C., Valenstein, M., Ganoczy, D., & Ignacio, R. V. (2007). Age comparison of treatment adherence with antipsychotic medications among individuals with bipolar disorder. International Journal of Geriatric Psychiatry: A journal of the psychiatry of late life and allied sciences, 22(10), 992-998.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 6
This next slide is a study that we did a number of years ago looking at the VA database and determining people’s level of adherence based on pharmacy refills.
So this was looking at people that were older and either fully adherent, taking 80% or more of their medications; partially adherent, so 50% to 80%; or nonadherent, less than 50%.
And you see that there are some clinical indicators that suggest risk factors for poor adherence including substance use, homelessness. In this sample, we did not see a difference for ethnicity. Now, again, this was a VA sample so is predominantly a male sample. So that does cause some limitations in data interpretation.
References:
- Sajatovic, M., Blow, F. C., Kales, H. C., Valenstein, M., Ganoczy, D., & Ignacio, R. V. (2007). Age comparison of treatment adherence with antipsychotic medications among individuals with bipolar disorder. International Journal of Geriatric Psychiatry: A journal of the psychiatry of late life and allied sciences, 22(10), 992-998.
Slide 4 of 6
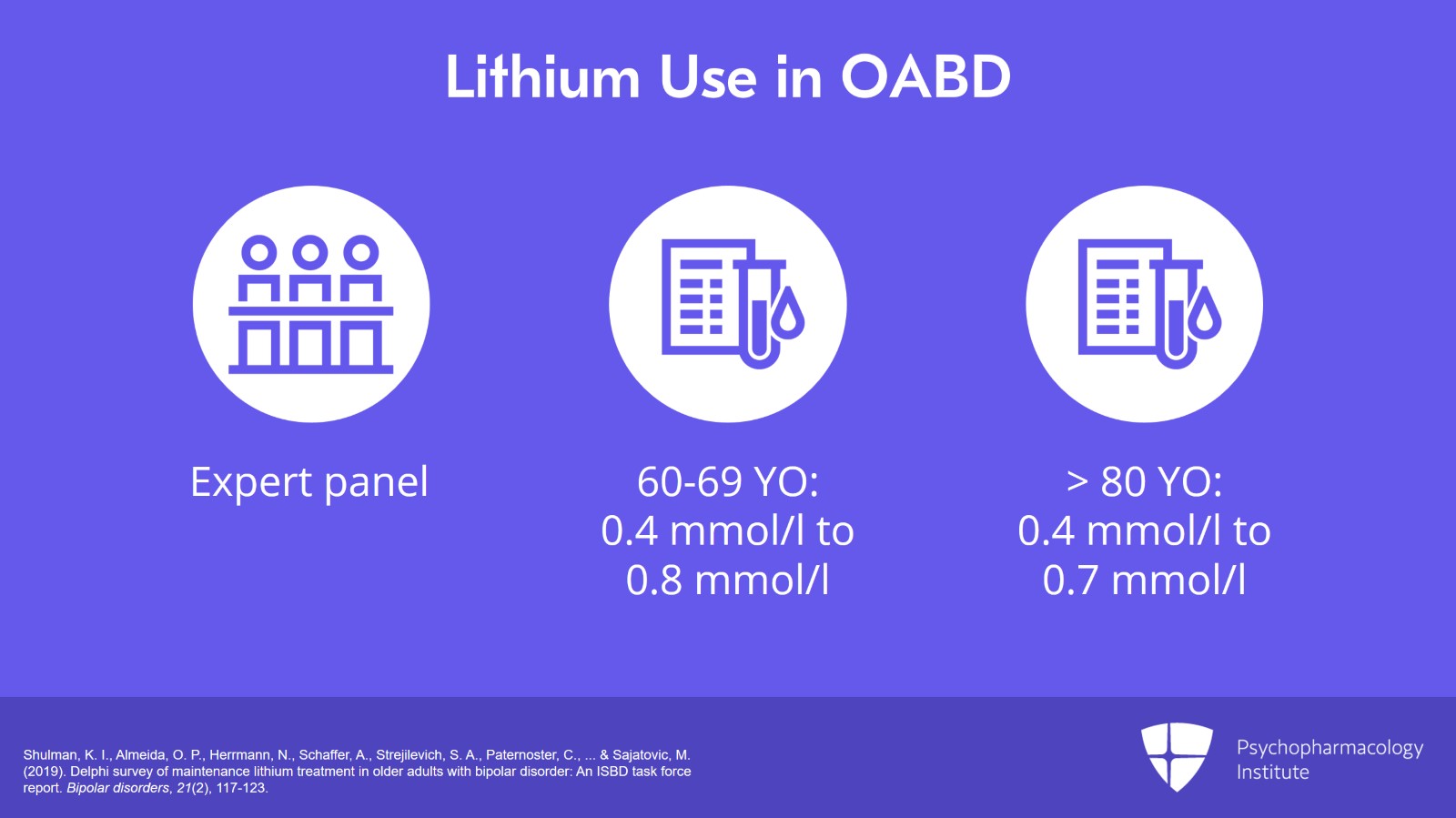
The other interesting recent study and actually we do have a publication now published in Bipolar Disorder by Dr. Shulman and colleagues. So this was a lithium use in OABD Delphi exercise done by our International Society for Bipolar Disorder Task Force. So the Delphi method is used when you don’t have other evidence like clinical trials or case registry studies. We convened an expert panel on OABD, aging and psychopharmacology and you ask the Delphi panel key questions. What we were interested in is: What is the place of lithium in the bipolar disorder medication armamentarium? What is the appropriate dosing and frequency? What types of biological monitoring is needed? What are your target levels? And what are the drug interactions and comorbidity that you have to be concerned about? So the Delphi process uses iterative surveys. So we would send the question out to the panel. The panel would independently answer them and then would come together to establish consensus and ask the questions in a sort of finer and finer grain way.
One of the important findings is that the recommendations of the panel is that serum level for lithium should be in the order of 0.4 to 0.8 for people between the ages of 60 and 69 and a little lower, 0.4 to 0.7, for people that were aged 80 and older. So as I said, that paper is actually published now in Bipolar Disorder. And for those who are interested in this topic, you can certainly go and read some of the additional recommendations of the panel. But it is a good way using the Delphi process to get information where there is a little less research data.
References:
- Kibble, A. (2015). American Psychiatric Association-168th Annual Meeting (May 16-20, 2015-Toronto, Canada). Drugs of today (Barcelona, Spain: 1998), 51(6), 375-382.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 6
The key points in this section are that perhaps not surprisingly given the methodological changes in studying maintenance or long-term treatment in older age bipolar disorder there is limited evidence to informed treatment decisions. A default option in this case is to continue the treatment that was helpful in the acute treatment during the maintenance phase. An exception of course is antidepressants that might be used to treat acute bipolar depression. And generally, most of the treatment guidelines in bipolar disorder generally recommend that one might try to minimize exposure to antidepressant drugs as they may help propel people into manic switching.
A key consideration with maintenance treatment is medication adherence. Existing data suggest that poor adherence is nearly as much of a problem in older people as it is in younger. A good rule of thumb is to consider that about half the people with bipolar disorder have suboptimal adherence. And then we touched lastly on the Delphi process with some emerging research in OABD. So the Delphi process is a technique that uses a panel of experts to guide decision making and recommendations where there is limited research. A Delphi panel of experts in OABD suggested that lithium is the preferred maintenance treatment in OABD but the target serum level should be slightly lower in the old-old, so those people that are age 80 and older, versus the young-old, those between 60 and below 80.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.