Slides and Transcript
Slide 1 of 9
Our next section is we’re going to dig a little bit into a case study and see how what we have discussed might apply clinically.
Slide 2 of 9
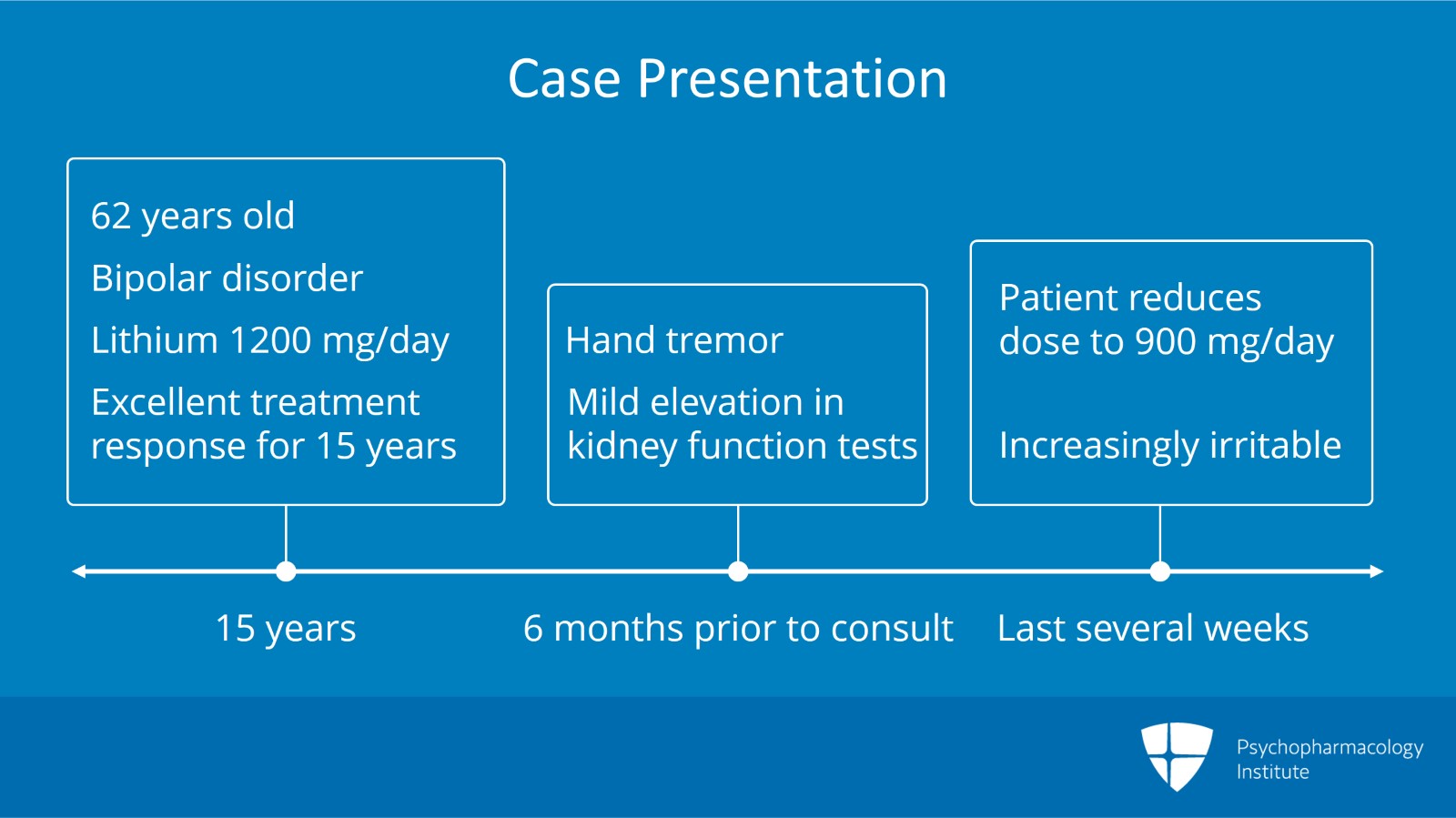
So our case example here is Marie. Marie is a 62-year-old woman with bipolar disorder who’s been maintained on lithium 1200 mg a day for 15 years. She’s done well with this including excellent performance at her job as an insurance company clerk. So she’s done well. Excellent response to lithium. Now, there’s a new problem. Six months ago, Marie noticed a mild hand tremor that caused embarrassment for her and interfered somewhat with her clerical work. Her clinician checked some basic laboratory testing and told her that everything looked okay except for “very mild elevation in kidney functioning.” But the clinician did not recommend further evaluation. However, Marie was worried about the ongoing tremor and the labs and she reduced her lithium on her own to 900 mg a day. The tremor resolved. In the last several weeks, however, the patient has become increasingly irritable at home. She’s made a couple of inappropriate and uncharacteristic comments to a coworker in the employee lounge which is very unusual for her. Now, her concerned husband comes with her to her clinician’s office.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 3 of 9
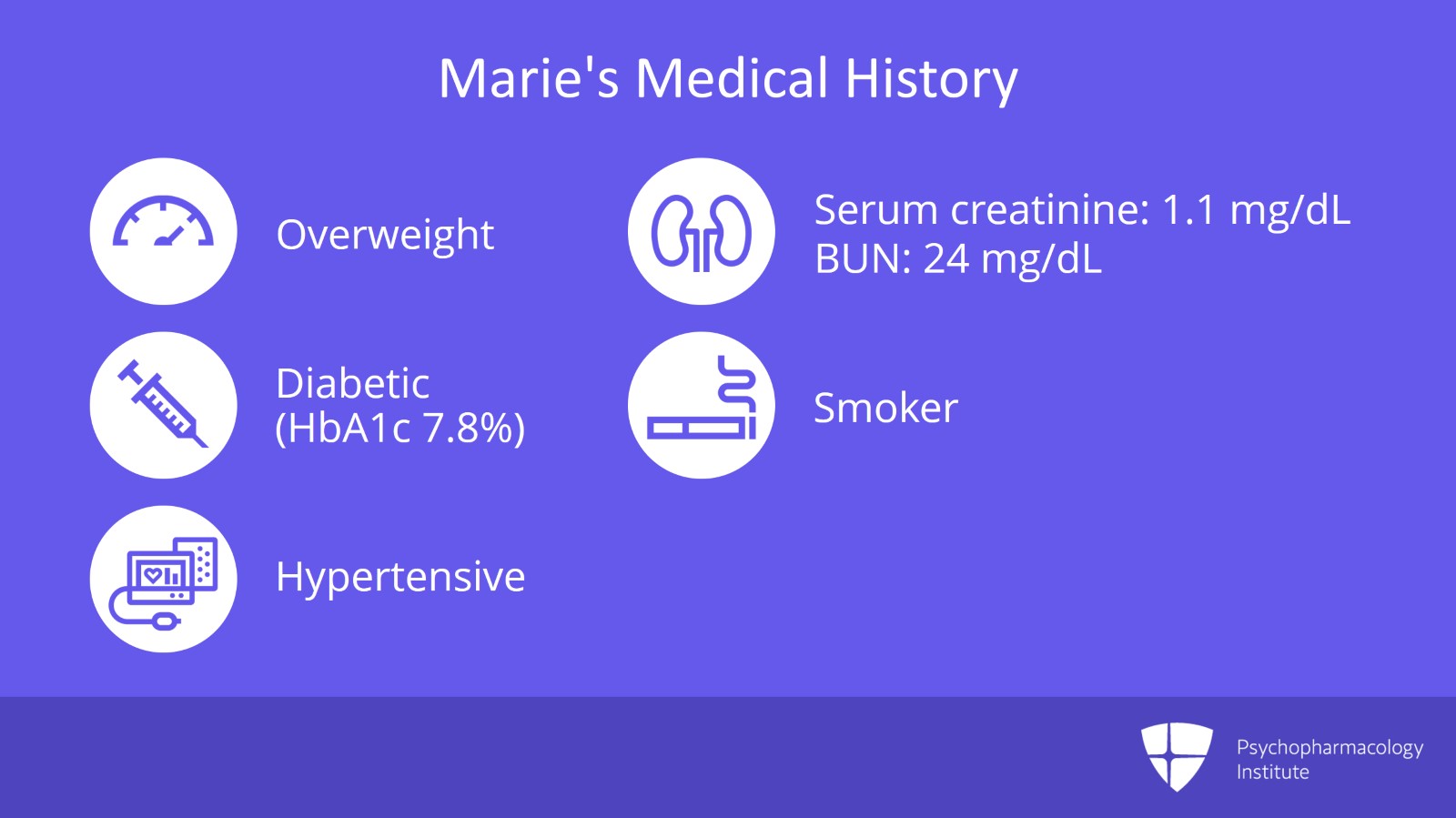
Just to give you a little background. Relevant medical history, Marie is 18 kilos overweight. Her last type 2 diabetes control evaluation of hemoglobin A1c or glycosylated hemoglobin was 7.8%. Generally, we’d like to see that below 7 but it’s not too bad. She has a history of hypertension. Last blood pressure check was 130/90. She is maintained on a beta blocker. Her serum creatinine was 1.1. Her BUN/blood urea nitrogen was 24. She smokes a half a pack of cigarettes per day.
Slide 4 of 9
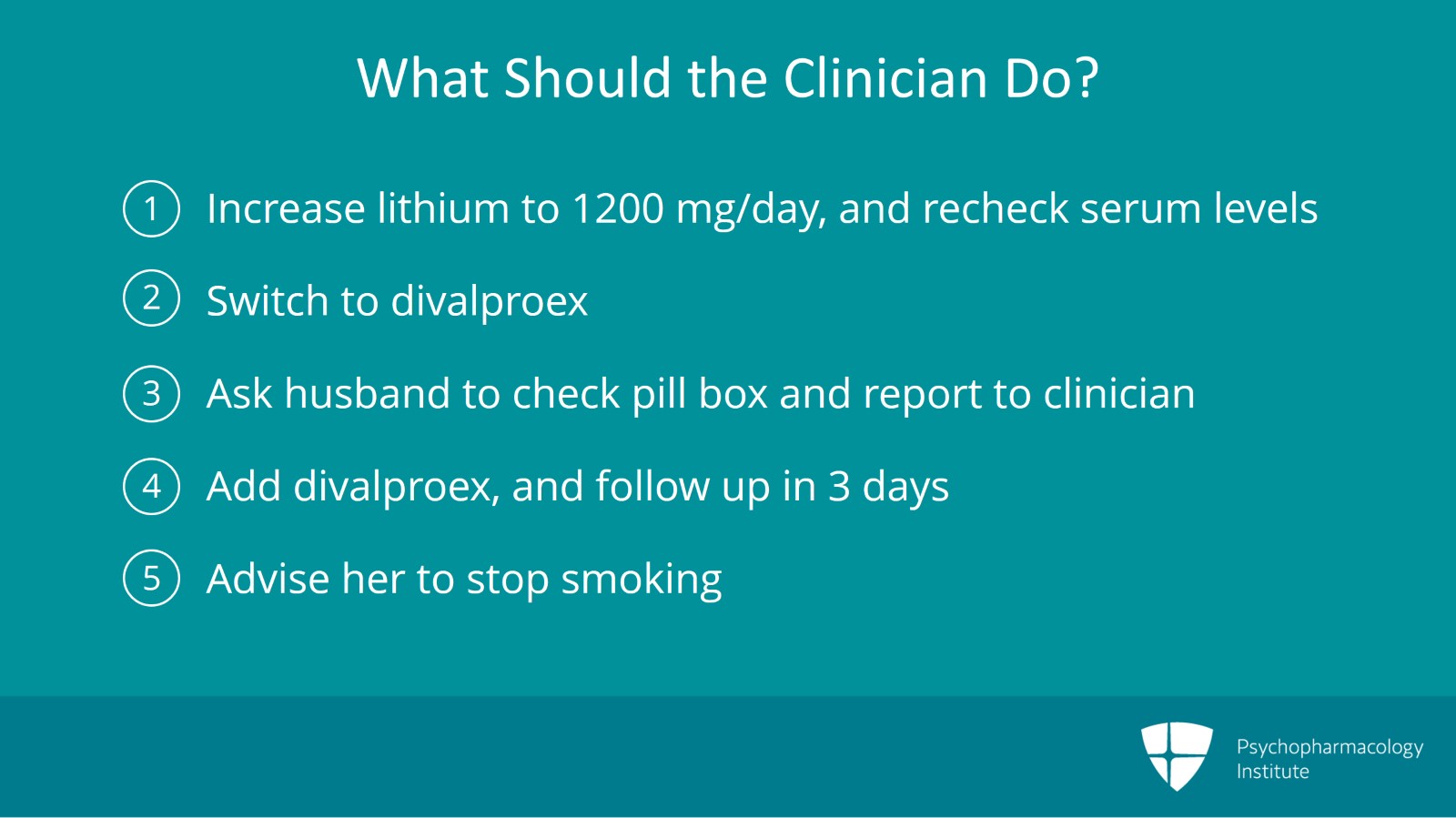
What are the best things for Marie’s clinician to do here? Choice one might be to increase her lithium back to 1200 mg a day and recheck serum levels. Two, stop lithium and switch to divalproex. Three, have her husband check her medication pill box daily and report missing doses to you. Four, add divalproex and see her in three days’ followup. Or five, tell her to stop smoking.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 9
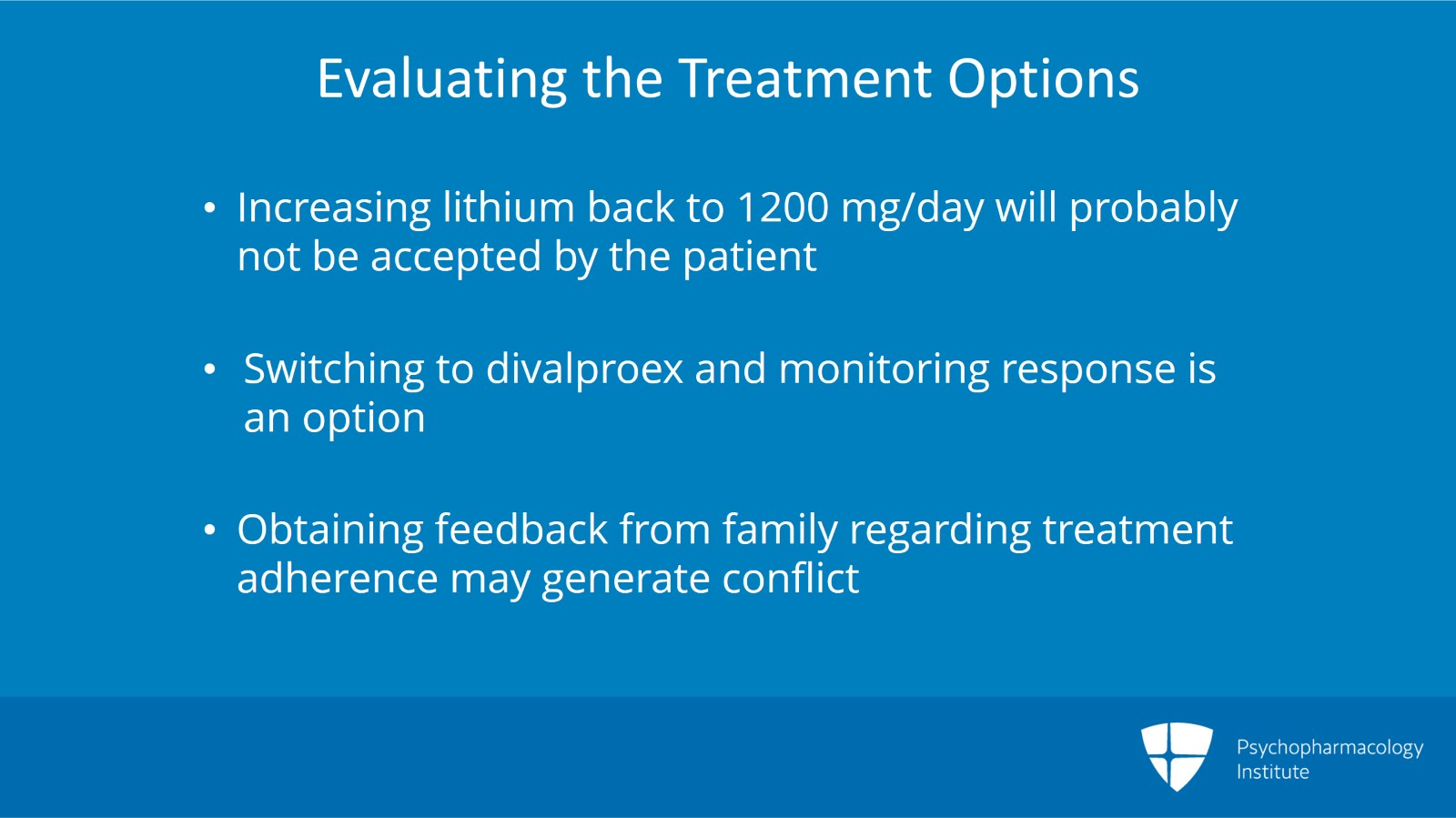
So if I were thinking about each of those, you know, in its sort of relative usefulness, I might say that increasing her lithium back to 1200 mg per day probably would treat this, what looks like emerging mania or hypomania with Marie. However, I would be concerned that that will not be something that the patient is going to be willing to sustain. So if you get lithium levels and it looks okay, that may just not augur well for continued adherence.
Choice number 2, stopping lithium and switching to divalproex certainly is an option. However, we don’t know how well she’s going to do with divalproex. Based on the data with GERI-BD study that I showed you earlier, it looks like both lithium and divalproex are good treatments for bipolar mania but it really is empiric to see which patient is going to respond. So that is one option.
Choice number 3 of having the husband check the medication pill box daily and report missing doses to you, that might be useful. I would potentially have a little concern with the kind of manic cycling patient getting monitored by the adherence police and that may be setting up some conflict that you don’t want to see. However, it would be prudent probably to have a discussion about adherence and get the husband’s input.
Slide 6 of 9
Option 4 might be to add divalproex and see her in three days’ followup. My preference probably would be for that option. We know she’s doing well with lithium. Could divalproex as an adjunct give her just a little bit better control of those mood symptoms?
And 5, telling her to stop smoking. Certainly, that’s never a bad idea but unlikely to have immediate effects.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 9
So just to summarize, our key points are the patient is exhibiting signs of hypomania that are likely a result of her self-reduced lithium dosing.
While increasing her lithium back to a higher dosage may help to manage the manic symptoms, it is likely not a sustainable option given Marie’s burdensome side effects.
Checking on medication adherence is not a bad option but be careful not to turn family into the compliance police as this may have problems in sustainment.
Slide 8 of 9
And again, I would never argue against stopping smoking but it’s unlikely to have immediate acute effects on her mania.
So given that we don’t know Marie’s potential response to divalproex, a reasonable approach might be to augment the lithium with divalproex. As always, assessing lithium and valproate levels as well as monitoring other relevant laboratory assessments and doing your clinical assessment is appropriate in OABD.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.