Slides and Transcript
Slide 1 of 12
In this section, I’m going to focus on depressive disturbances in Parkinson’s disease. Depression in Parkinson’s disease has a larger impact on quality of life than even the motor symptoms that define the disease.
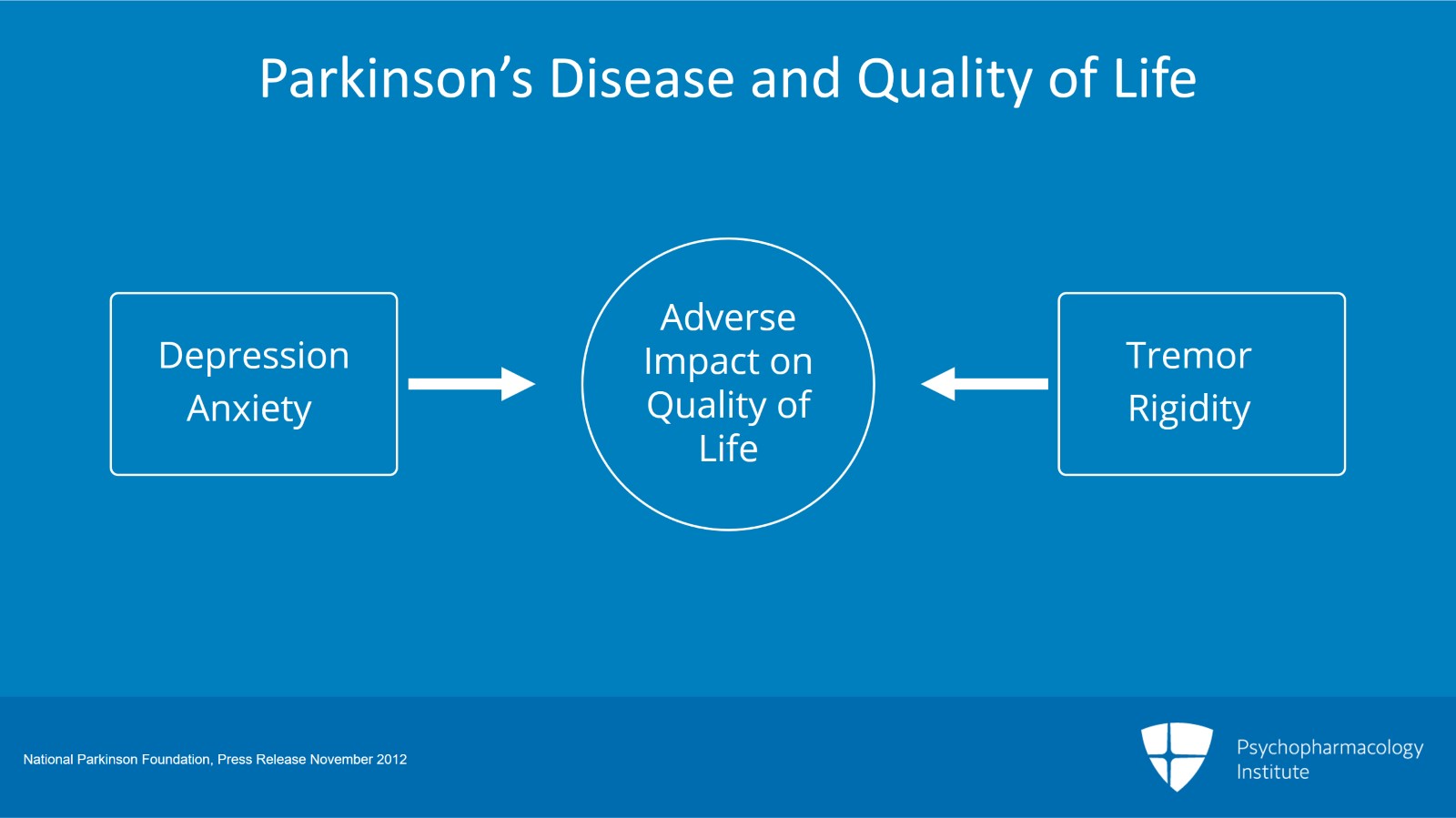
Slide 2 of 12
The largest ongoing study of people with Parkinson’s disease and outcomes on quality of life that was initially started by the National Parkinson Foundation has shown that when you look at symptoms longitudinally the depression and anxiety contribute at least as much of an adverse impact on quality of life as tremor, rigidity and the other symptoms. And so this makes it a very important clinical symptom to target when you’re trying to treat the person with Parkinson’s disease.
References:
- National Parkinson Foundation, Press Release November 2012
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
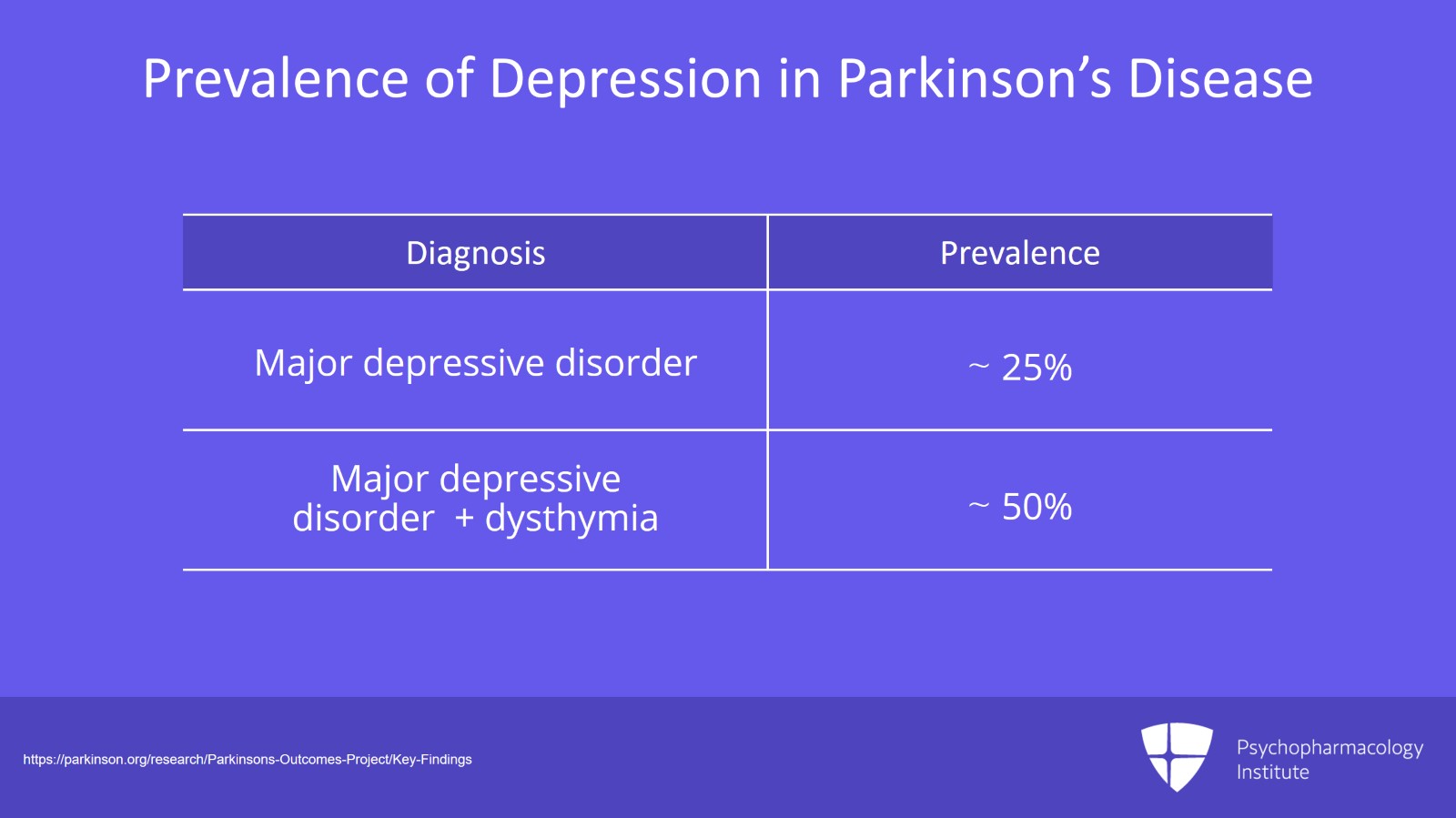
Slide 3 of 12
As I mentioned in the earlier videos, the prevalence rates of depressive disorders in Parkinson’s are higher than that in the general population and even other similarly disabling diseases with prevalence rates from about 25% for major depression up to 50% if you include both major and minor depressive disturbances like dysthymia.
References:
- https://parkinson.org/research/Parkinsons-Outcomes-Project/Key-Findings
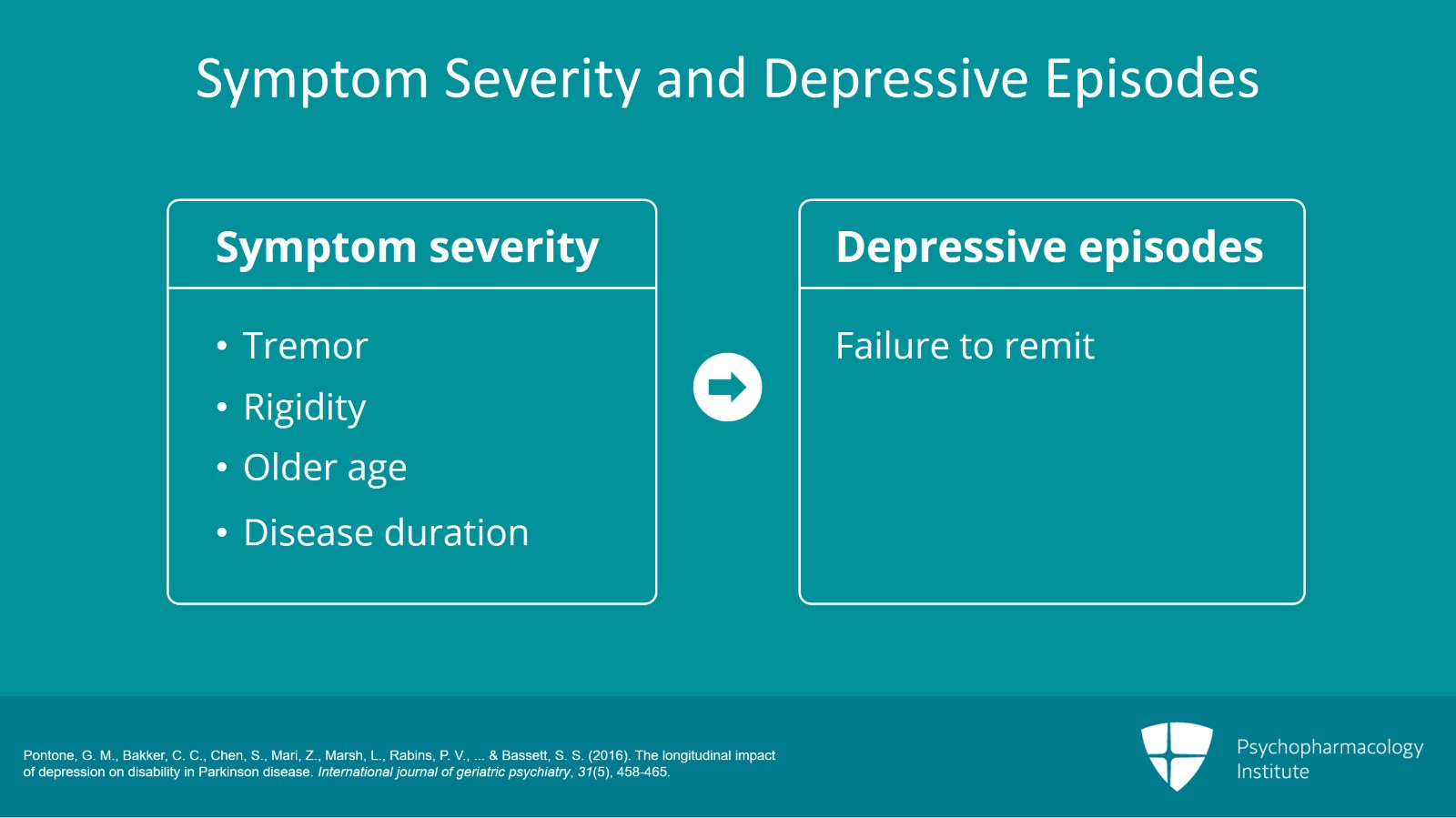
Slide 4 of 12
An association between the symptom severity so having maybe worse tremor or worse rigidity and depression, being older and having a longer duration of Parkinson’s predict a failure of depressive episodes to remit. So these are things that can influence the episodic nature of the depressive disturbance within Parkinson’s disease.
References:
- Pontone, G. M., Bakker, C. C., Chen, S., Mari, Z., Marsh, L., Rabins, P. V., … & Bassett, S. S. (2016). The longitudinal impact of depression on disability in Parkinson disease. International journal of geriatric psychiatry, 31(5), 458-465.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 5 of 12
And depression, it is clearly associated with the motor deficits and disability of Parkinson’s. And originally, we thought this might be just a unidirectional association but we actually conducted a study that I’ll talk about now that showed that this was a bidirectional relationship between depression and physical disability.
References:
- Pontone, G. M., Bakker, C. C., Chen, S., Mari, Z., Marsh, L., Rabins, P. V., … & Bassett, S. S. (2016). The longitudinal impact of depression on disability in Parkinson disease. International journal of geriatric psychiatry, 31(5), 458-465.
Slide 6 of 12
I’d like to talk about a study that we conducted at my center on the longitudinal effects of depression status on physical activities of daily living and Parkinson’s disease. In this study, we looked at 136 individuals who are followed in our longitudinal study of Parkinson’s disease. And we let them enter the study at their first visit which we called baseline and then followed them at two-year intervals.
References:
- Pontone, G. M., Bakker, C. C., Chen, S., Mari, Z., Marsh, L., Rabins, P. V., … & Bassett, S. S. (2016). The longitudinal impact of depression on disability in Parkinson disease. International journal of geriatric psychiatry, 31(5), 458-465.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 7 of 12
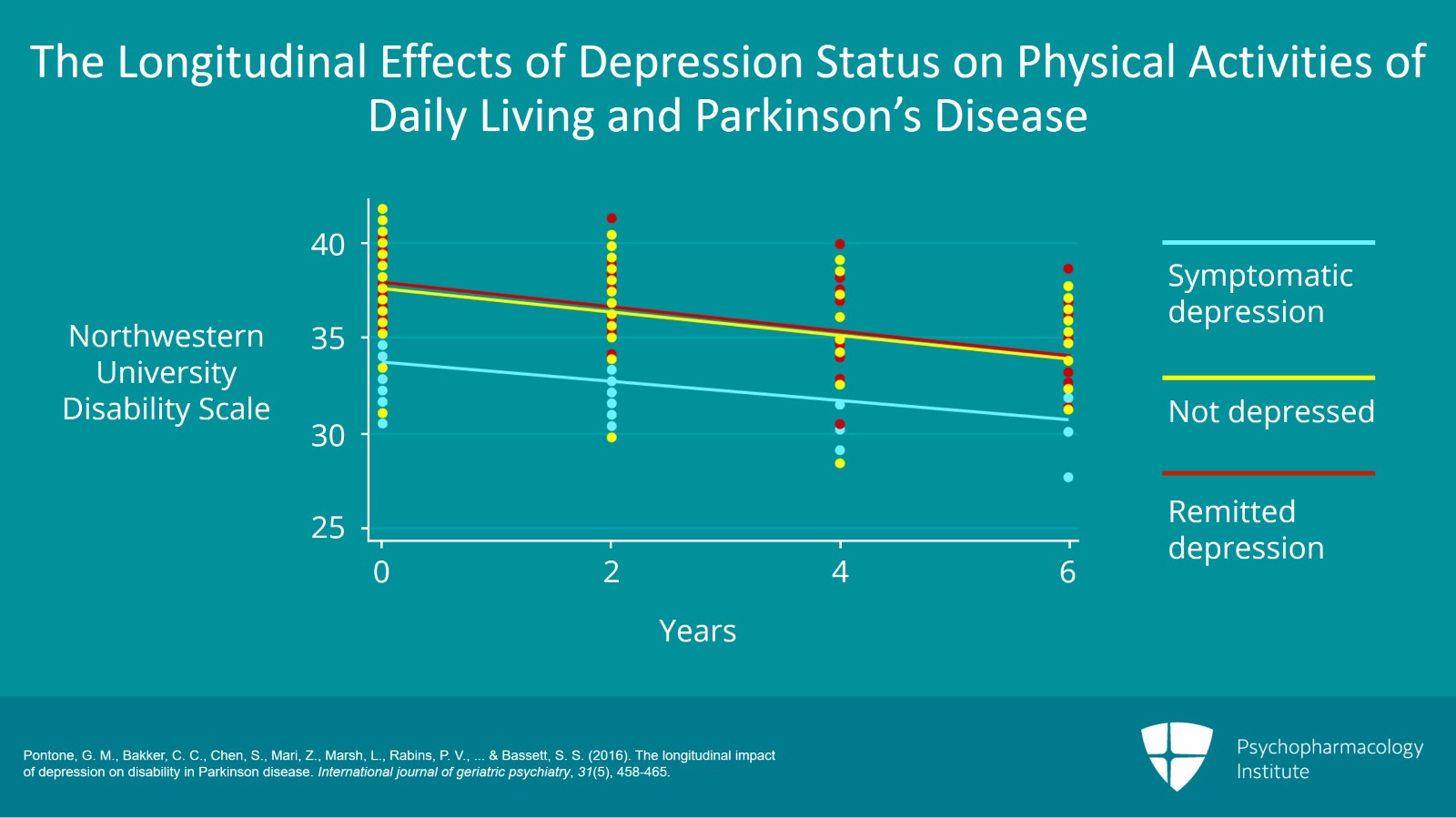
And this figure that I want to orient you to follows the first six years of their involvement in this study. On the Y axis, you can see that the activities of daily living were scored using something called the Northwestern University Disability Scale where basically the lower scores indicate greater disability and the higher scores are people who are more functional. Then the X axis is baseline which is time zero on the left all the way up to six years in the study. And I think the first thing that you can see is regardless of whether you’re symptomatically depressed, not depressed or had a depressive episode that remitted for any reason whether it was treated or untreated remission, you can see that the slope of all three lines declines over time. And that’s just the nature of a neurodegenerative disorder. There’s going to be some increase in physical impairment with time. What’s interesting though is if you look at this blue line which are people who are symptomatically depressed at any point whether at baseline or at two-, four- or six-year follow up, they are functioning physically and when I say physical activities, I mean things like walking, hygiene, feeding yourself, dressing and speech, at a lower level than people who have no depression. And so essentially, we know that having a depressive illness directly influences your ability to function physically. And so this data was actually presented at the International Movement Disorder Society’s annual meeting plenary talk. And the good news clinically here is that if you treat people who have active depression or if they spontaneously remit, not only do they get relief from suffering from depression, their physical disability improves.
References:
- Pontone, G. M., Bakker, C. C., Chen, S., Mari, Z., Marsh, L., Rabins, P. V., … & Bassett, S. S. (2016). The longitudinal impact of depression on disability in Parkinson disease. International journal of geriatric psychiatry, 31(5), 458-465.
Slide 8 of 12
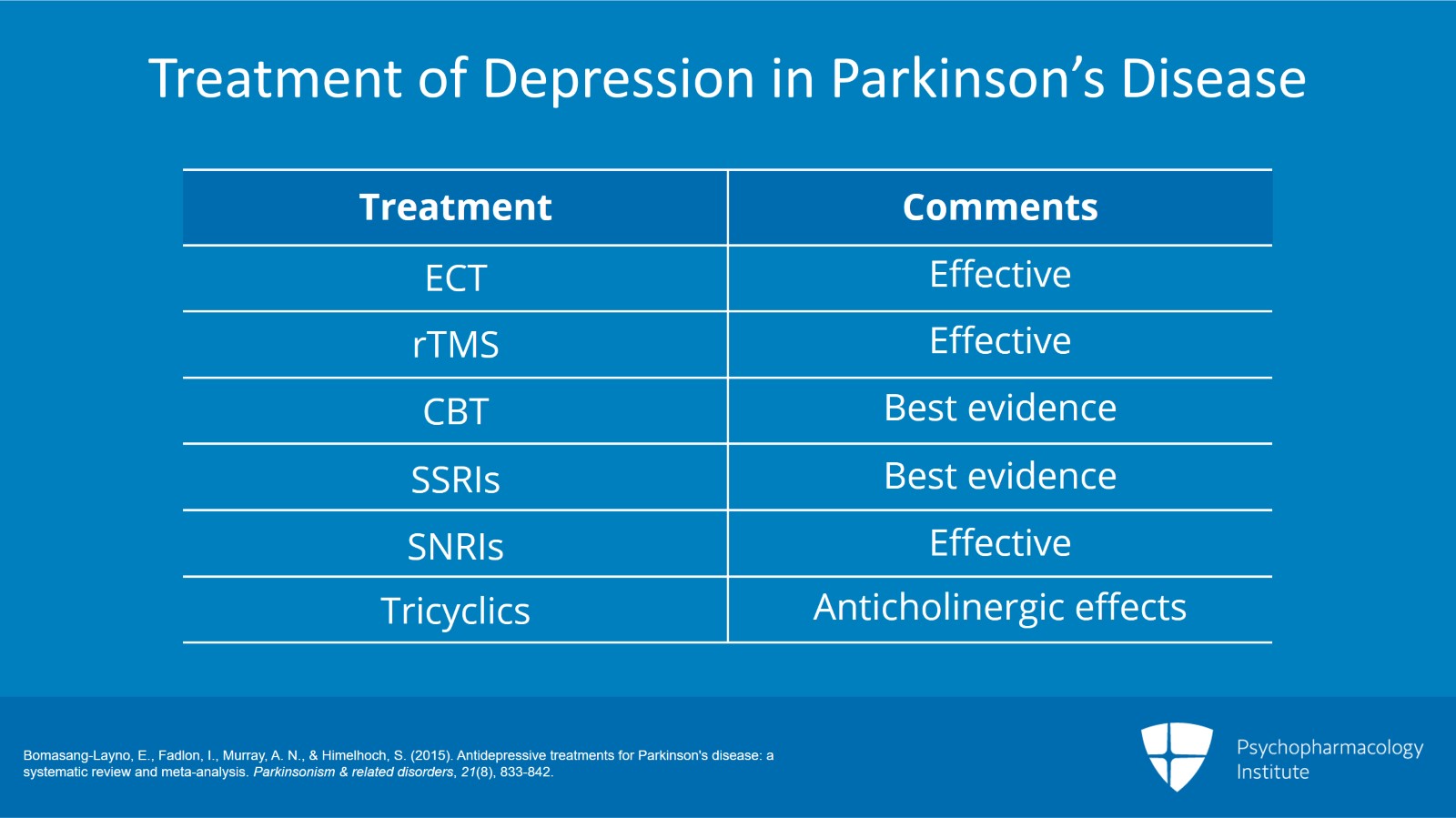
Now, the treatment of major depression in Parkinson’s has been studied over the years. And basically, the take home here is that almost all of the standard treatments in the general population for depression are reasonable to try in Parkinson’s disease. That includes ECT, rTMS, cognitive behavioral therapy, all the classes of antidepressants, SSRIs, SNRIs, tricyclics. However, with tricyclics, you just have to be a little careful because if they have anticholinergic side effects, the people with Parkinson’s are a little more likely to have both the confusional effects from the anticholinergic side effects but also increase their risk of falls. You can see here that the clear signal for efficacy is with the selective serotonin reuptake inhibitors and cognitive behavioral therapy. They both significantly improved depression in Parkinson’s. Now, those have best evidence. However, there is also good evidence for SNRIs like Effexor in individual studies. So in terms of having a first line treatment, the selective serotonin reuptake inhibitors and cognitive behavioral therapy should be chosen first because they also have a low side effect profile.
References:
- Bomasang-Layno, E., Fadlon, I., Murray, A. N., & Himelhoch, S. (2015). Antidepressive treatments for Parkinson's disease: a systematic review and meta-analysis. Parkinsonism & related disorders, 21(8), 833-842.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 9 of 12
And when you use antidepressants, there is a concern that they might interact with certain dopamine replacement therapies. Specifically, we often use things like rasagiline and selegiline to treat Parkinson’s disease. And these are MAO-B selective inhibitors, so monoamine oxidase B selective inhibitors, meaning they’re reversible. And even though there’s a theoretical warning of using these together, there are big clinical trials in Parkinson’s that show that they’re used concurrently in Parkinson’s without increasing the overall adverse effects. You should absolutely still exercise caution but I will tell you that in clinical practice in Parkinson’s, antidepressants are used in combination with these monoamine oxidase B selective inhibitors.
References:
- Bomasang-Layno, E., Fadlon, I., Murray, A. N., & Himelhoch, S. (2015). Antidepressive treatments for Parkinson's disease: a systematic review and meta-analysis. Parkinsonism & related disorders, 21(8), 833-842.
Slide 10 of 12
Interestingly, although it’s thought to be an antidepressant that probably has some pro-dopaminergic properties, there’s no evidence to suggest that bupropion has any additional benefit for depression in Parkinson’s over the other antidepressant classes. Also, there’s no evidence to say it’s any less efficacious. So I would say that it’s also a very reasonable choice to treat depression.
References:
- Bomasang-Layno, E., Fadlon, I., Murray, A. N., & Himelhoch, S. (2015). Antidepressive treatments for Parkinson's disease: a systematic review and meta-analysis. Parkinsonism & related disorders, 21(8), 833-842.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.
Slide 11 of 12
So the key points for this section are that depression has a greater adverse impact on quality of life than even the motor symptoms of Parkinson’s. Depression in Parkinson’s is associated with a greater overall physical disability. And selective serotonin reuptake inhibitors and cognitive behavioral therapy have the best evidence for efficacy and safety when treating depression in Parkinson’s disease.
Free Files
Download PDF and other files
Success!
Check your inbox, we sent you all the materials there.