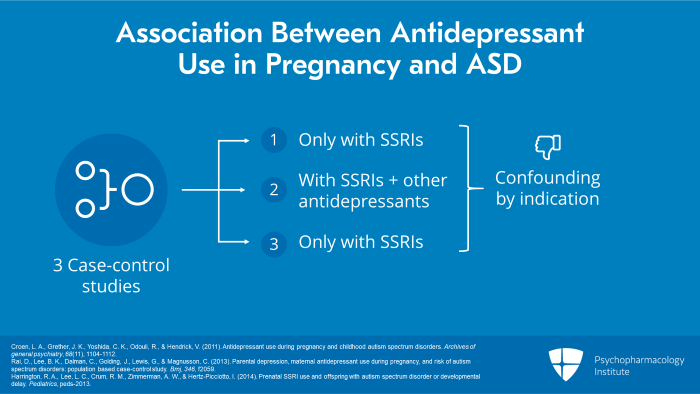
So let’s look at yet another concern that has arisen lately with regard to the use of SSRIs in pregnancy and that is possible association with autism. Some years ago, there were three case-control studies, one at Kaiser in Northern California, one in Sweden and one in the State of California called the CHARGE Study. All of these were case-control studies, tried to control for a number of confounders and they suggested possible association between antidepressant use in pregnancy and ASD. The Kaiser study found an association only with SSRIs. The Swedish study, an association with other antidepressants as well. And the California CHARGE Study, association with SSRIs for ASD and possibly development delay in boys. None of these studies suggested that this was enough to explain the huge rise in ASD since the 1980s and all of them had major problems with regard to confounding by indication.
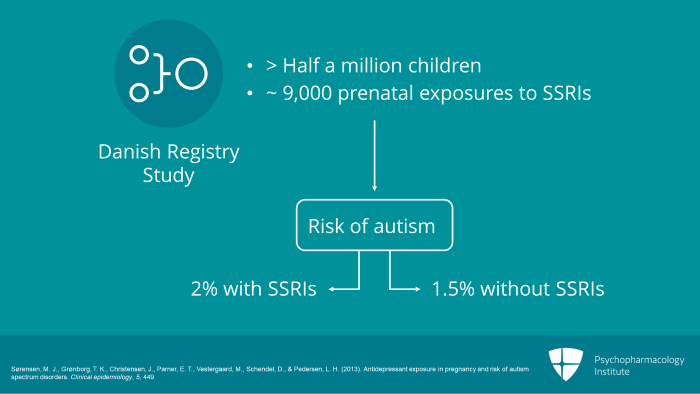
However, a new large Danish registry study was then published. It looked at data from more than half a million children born between 1996 and 2006 looking at nearly 9000 prenatal exposures to SSRIs with over 6000 with maternal affective histories. And what they found was with prenatal SSRI exposure, there was a 2% risk of autism as opposed to 1.5% without SSRIs.
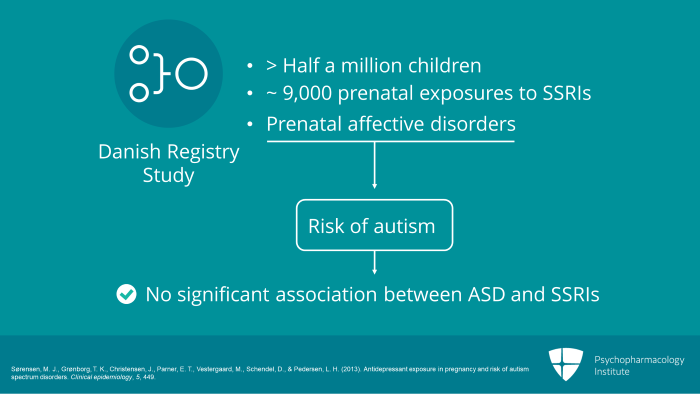
Now, if the data were restricted to children of mothers with prenatal affective disorders, there was no statistically significant risk in ASD with prenatal SSRI exposure and comparing siblings with and without ASD, prenatal SSRI exposures was not a significant contributor to ASD risk. So they concluded after confounding factors were controlled for that there was no significant association between prenatal SSRI exposure and ASD in offspring.
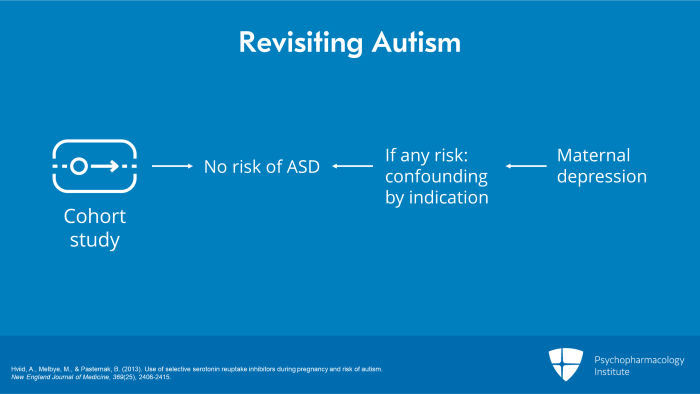
Revisiting the issue of autism yet again was a second new Danish study which also suggested no risk of ASD. This was a large cohort study and it found that SSRI exposure prior to pregnancy rather than during pregnancy was statistically significantly associated with an increased risk for ASD. They concluded that any increased risk was due to confounding by indication rather than by any effect of SSRIs, such as maternal depression. In other words, maternal depression, not antidepressants, increased the risk for ASD.
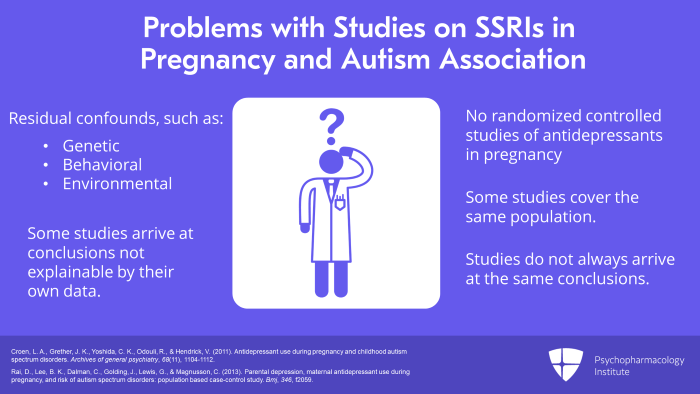
So what is the problem with the studies with regard to SSRIs in pregnancy and possible autism association? There are in fact no randomized controlled studies of antidepressants in pregnancy. Even though there have been attempts to address issues of confounding by indication, there is still a lot of residual confounding from unknown or unmeasured confounds, genetic, behavioral, environmental. Also numerous studies cover the same population so databases are not as large as they seem to be. And these studies actually did not always arrive at the same conclusions. And in fact, some of the studies arrived at conclusions that weren’t even explainable by their own data or findings.
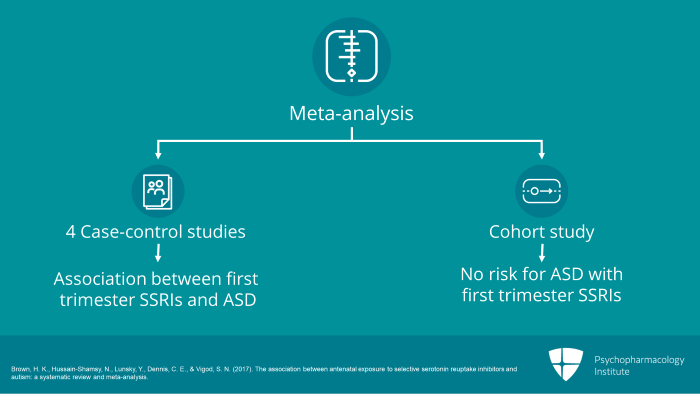
Most recently, new light has been further shed on SSRIs on the subject of autism. A meta-analysis done in 2017 published in JCP reviewed prior studies, the four case-control studies which did show an association between first trimester SSRIs and ASD and the one better cohort study which accounted for comprehensive confounders which found no risk for ASD with first trimester SSRIs.
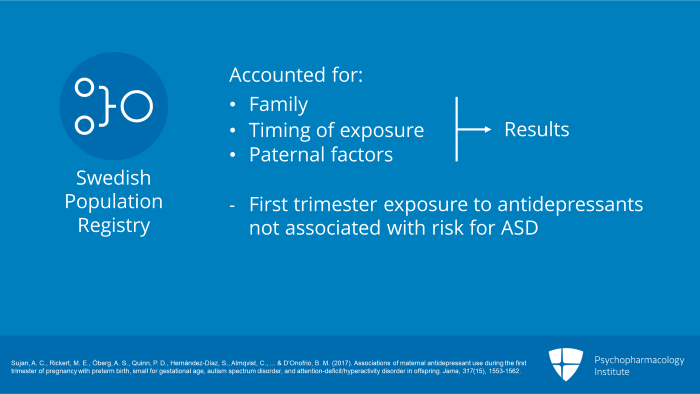
The data also in 2017 included an article that was published in the Journal of the American Medical Association by Sujan and others and it looked at more than a million and a half offspring from a Swedish population registry. It accounted for family, timing of exposure and paternal factors. And they found that first-trimester exposure to antidepressants was not associated with a risk for ASD. In fact, unexposed siblings were at equal risk for both ASD and ADHD.
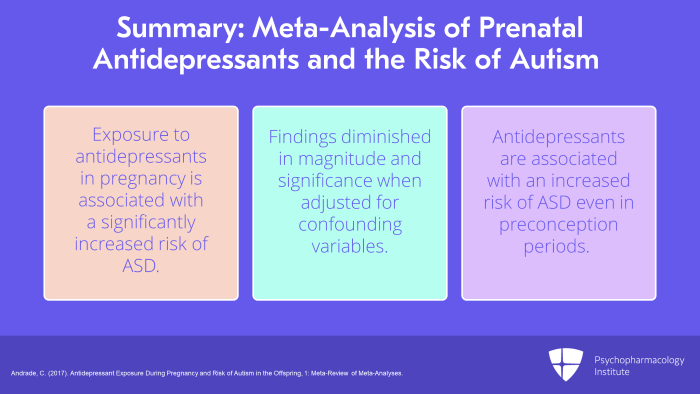
So I’d like to summarize for you the recent meta-analysis of prenatal antidepressants and the risk for autism as written in the Journal of Clinical Psychiatry by Dr. Andrade in 2017, an excellent review. And what he points out is as follows. Some studies have found that exposure to antidepressants in pregnancy in general or with SSRIs is associated with significantly increased risk of ASD. But findings diminished in magnitude and significance when the data was adjusted for confounding variables especially maternal mental illness. Antidepressants were associated with increased risk even when exposure was limited to preconception periods when drugs could never have possibly affected the fetus. He went on to say that just because antidepressants are associated with an increase in risk of ASD that doesn’t mean that antidepressants are responsible for that risk.
If antidepressants do increase the risk for ASD, of course, we need to discuss this with our patients but we have to remind them to keep in mind that although studies do not prove antidepressants increase ASD, it’s understandable that women are concerned. Although case control studies may identify associations, they often overestimate the magnitude of risk.
The key points then, number one, although some studies suggest an increased risk for ASD or autistic spectrum disorders with prenatal exposure to antidepressants, when confounders are addressed especially confounding by indication, this risk is reduced and often nonexistent. Treating maternal mental illness is important to address women’s psychiatric suffering and to reduce the risk for impairment and offspring outcomes due to parental depression, anxiety and associated maladaptive parenting behaviors.
References
- Croen, L. A., Grether, J. K., Yoshida, C. K., Odouli, R., & Hendrick, V. (2011). Antidepressant use during pregnancy and childhood autism spectrum disorders. Archives of general psychiatry, 68(11), 1104-1112.
- Rai, D., Lee, B. K., Dalman, C., Golding, J., Lewis, G., & Magnusson, C. (2013). Parental depression, maternal antidepressant use during pregnancy, and risk of autism spectrum disorders: population based case-control study . Bmj, 346, f2059.
- Harrington, R. A., Lee, L. C., Crum, R. M., Zimmerman, A. W., & Hertz-Picciotto, I. (2014). Prenatal SSRI use and offspring with autism spectrum disorder or developmental delay . Pediatrics, peds-2013.
- Sørensen, M. J., Grønborg, T. K., Christensen, J., Parner, E. T., Vestergaard, M., Schendel, D., & Pedersen, L. H. (2013). Antidepressant exposure in pregnancy and risk of autism spectrum disorders. Clinical epidemiology, 5, 449.
- Hviid, A., Melbye, M., & Pasternak, B. (2013). Use of selective serotonin reuptake inhibitors during pregnancy and risk of autism. New England Journal of Medicine, 369(25), 2406-2415.
- Brown, H. K., Hussain-Shamsy, N., Lunsky, Y., Dennis, C. E., & Vigod, S. N. (2017). The association between antenatal exposure to selective serotonin reuptake inhibitors and autism: a systematic review and meta-analysis.
- Sujan, A. C., Rickert, M. E., Öberg, A. S., Quinn, P. D., Hernández-Díaz, S., Almqvist, C., … & D’Onofrio, B. M. (2017). Associations of maternal antidepressant use during the first trimester of pregnancy with preterm birth, small for gestational age, autism spectrum disorder, and attention-deficit/hyperactivity disorder in offspring. Jama, 317(15), 1553-1562.
- Andrade, C. (2017). Antidepressant Exposure During Pregnancy and Risk of Autism in the Offspring, 1: Meta-Review of Meta-Analyses.



