Combination and Augmentation: Clarifying Concepts

This normally means going on with the current treatment which would generally be an antidepressant which hasn’t been particularly effective and to then add a second agent. Conventionally, the phrase combination treatment refers to adding a second drug that’s also an antidepressant in its own right, so a drug such as mirtazapine.

And this is probably because if you add something in, then you don’t lose the effects of the first treatment when you withdraw it as you might in a switch.
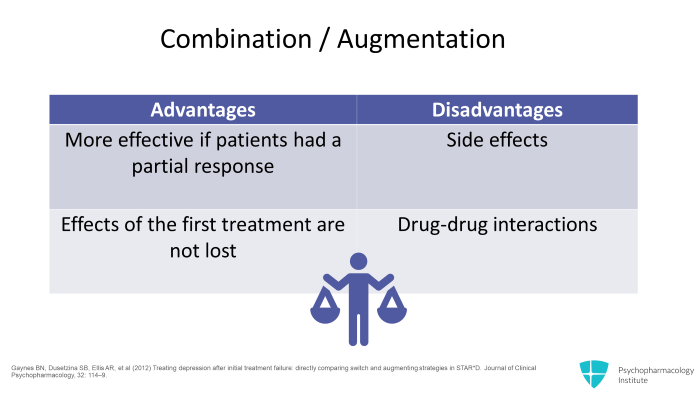
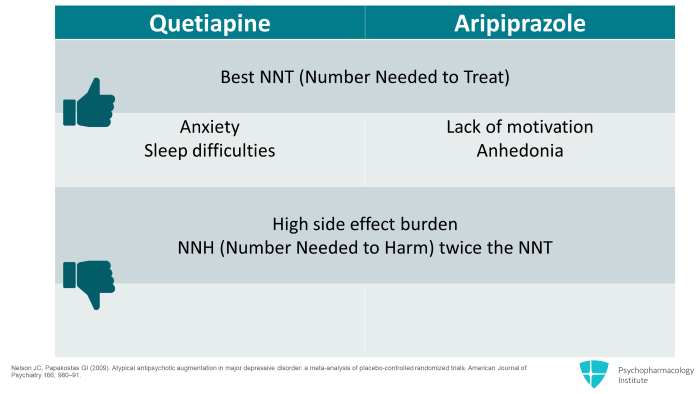
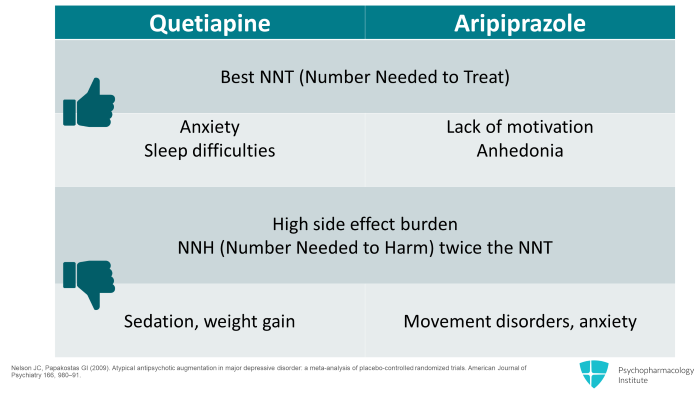
The problem with adding two drugs together is of course the side effect burden tends to be greater and the risk of interaction is there.

So just to summarize the key points there, adding a second drug in either combination or augmentation is slightly more effective and faster acting than a switch in treatment. On the other hand, there’s a greater risk of side effects and drug interaction.
Augmentation with Second-Generation Antipsychotics
So moving on to second-generation antipsychotic drugs. So the augmentation strategy with the best evidence base is the addition of atypical antipsychotic drugs.
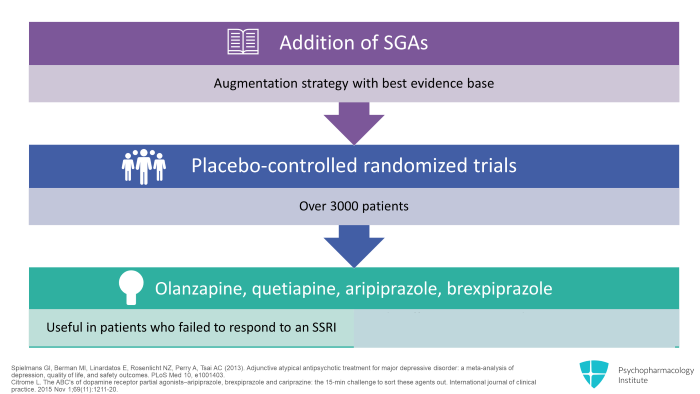
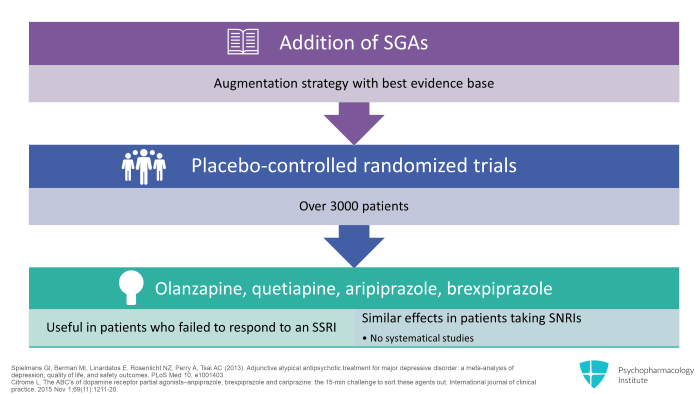
The same kind of effect seems to occur in patients taking SNRIs though this is not being studied so systematically.
The doses of atypicals used for this purpose are distinctly lower than those used to treat psychosis.
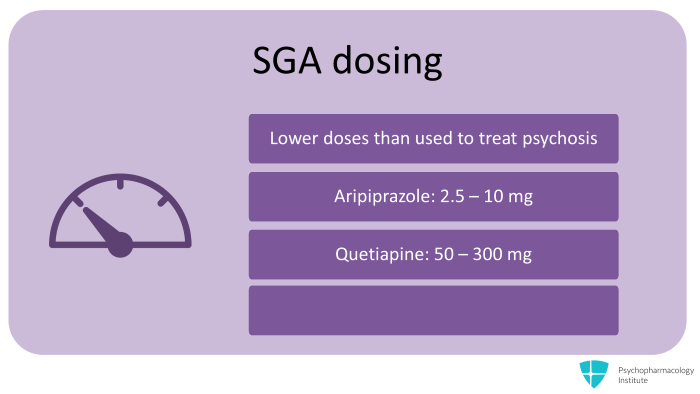
So one is thinking of a dose of about 2.5 to 10 mg of aripiprazole, 50 to 300 mg of quetiapine.
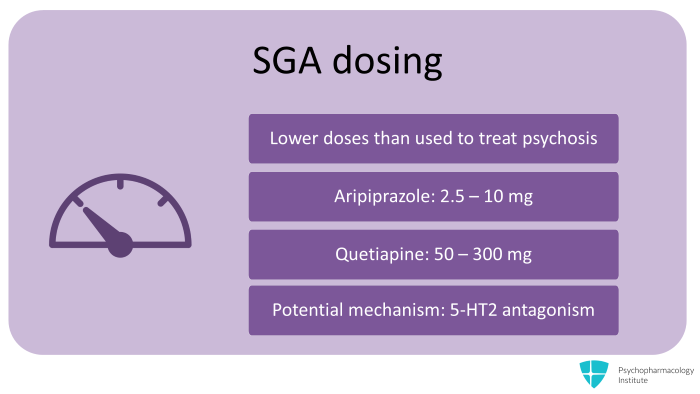
Pharmacologically, 5-HT2 receptor blockade has been implicated.
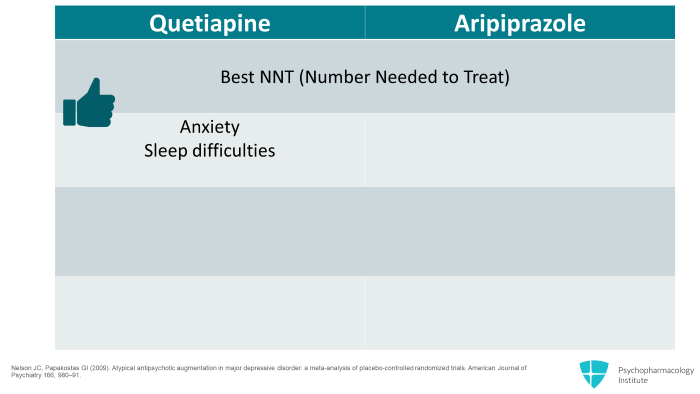
So for a patient who is sleeping poorly with anxiety, adding quetiapine at night might be helpful.
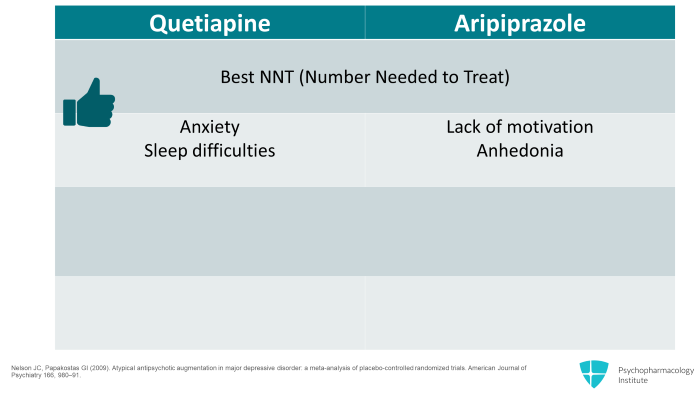
Patients who seem to have more problems with motivation and anhedonia can be helped by the addition of aripiprazole.
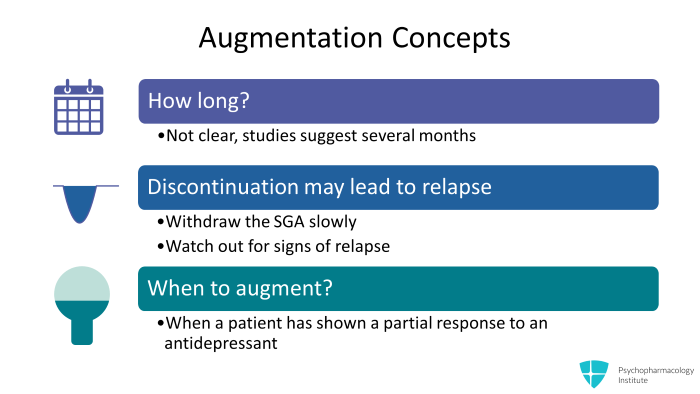
One thing that I’m sometimes asked is how long should patients stay on this augmentation, combination of treatments if they do respond to the addition of an atypical? The answer is that it’s not very clear at the moment. These studies and literature suggest that often the combined treatment needs to be carried on for several months

Another thing to add is particularly if you want to avoid weight gain, I would avoid mirtazapine with which that’s a major problem and go for something like aripiprazole or bupropion. Just another thing to mention is that bupropion is not licensed in the treatment of depression in the UK where it’s licensed only for the management of smoking cessation.
References
- Gaynes BN, Dusetzina SB, Ellis AR, et al (2012) Treating depression after initial treatment failure: directly comparing switch and augmenting strategies in STAR*D . Journal of Clinical Psychopharmacology, 32: 114–9.
- Spielmans GI, Berman MI, Linardatos E, Rosenlicht NZ, Perry A, Tsai AC (2013). Adjunctive atypical antipsychotic treatment for major depressive disorder: a meta-analysis of depression, quality of life, and safety outcomes . PLoS Med 10, e1001403.
- Citrome L. The ABC’s of dopamine receptor partial agonists–aripiprazole, brexpiprazole and cariprazine: the 15‐min challenge to sort these agents out . International journal of clinical practice. 2015 Nov 1;69(11):1211-20.
- Nelson JC, Papakostas GI (2009). Atypical antipsychotic augmentation in major depressive disorder: a meta-analysis of placebo-controlled randomized trials . American Journal of Psychiatry 166, 980–91.
- Pae CU, Wang SM, Han C, Lee SJ, Patkar AA, Masand PS (2015). Quetiapine augmentation for depression: dosing pattern in routine practice . International Clinical Psychopharmacology 30, 54-8.



